Abstract
Background
Dome liver lesions (those in segments VII or VIII) pose a challenge to standard laparoscopic resection. The use of additional intercostal and transthoracic trocars (ITTs) potentially facilitates resection over standard subcostal laparoscopic (SSL) techniques.
Methods
A retrospective review of a prospectively collected liver resection database was performed, selecting all minor resections of segments VII and VIII using the ITT and SSL approaches. The techniques of intercostal transdiaphragmatic access are described and the surgical outcomes of the two groups compared.
Results
A total of 19 patients were analysed. The ITT group included 8 patients and the SSL group included 11. The groups were comparable in median lesion size (20 mm in the ITT group and 26 mm in the SSL group). Blood loss, operative times, morbidity and conversion rates were similar. There was no lung injury or postoperative clinical pneumothorax in any patient undergoing transdiaphragmatic access. Median hospital stay was significantly shorter in the ITT group (2 days) than in the SSL group (6 days) (P = 0.032).
Conclusions
The ITT approach is safe, effective and complementary to standard laparoscopic techniques for the resection of small tumours in segments VII and VIII.
Introduction
Laparoscopic liver resection has been demonstrated to be safe and effective in the removal of malignant liver tumours.1–5 Lesions in segments VII and VIII, however, pose a challenge to standard laparoscopic techniques. One obstacle to safe resection is the often limited view of the lesion, even with high subcostal port placement. Additionally, the enforced angle of transection imposed by the ribs can lead to an unnecessarily generous anterior margin to ensure a negative margin (R0) resection. In the authors' experience, both bleeding requiring conversion and margin involvement have led to the abandonment of a purely laparoscopic approach to the resection of dome lesions.
The ribcage and diaphragm should not be considered as barriers to laparoscopic access and the placement of ports through the intercostal spaces can be performed with minimal morbidity. With a direct view of the lesion, additional ports through intercostal spaces allow the placement of instruments along all transection planes.
This report describes an experience in eight patients in whom the use of additional intercostal transdiaphragmatic and sometimes transthoracic ports allowed for the safe resection of dome lesions with minimal access. This paper describes the key technical points involved in achieving these resections and compares the outcomes in this group with those in a group of patients submitted to standard laparoscopic approaches for similarly placed lesions.
Materials and methods
All patients were retrospectively identified from a prospectively collected database of 340 laparoscopic liver resections performed from 1997 to 2013. Patients who underwent laparoscopic liver resection of lesions located solely in segments VII and/or VIII using intercostal and transthoracic trocars (ITTs) were selected. All surgeries in the ITT group were performed by a single surgeon (NO'R) between March 2011 and May 2013. Outcomes in these patients were compared with those in patients with similarly located lesions resected using standard subcostal laparoscopic (SSL) techniques during the period from July 2004 to September 2012. Data on patient demographics, clinical status, diagnosis, operative parameters and clinical outcomes were studied. The Brisbane nomenclature was used to describe the resections performed.6 Ethics approval was obtained prior to the commencement of this study.
Outcome measures included median operating time, median length of stay (LoS), median blood loss, median resection margin and conversions. A positive margin was defined as a surgical margin of <1 mm. Complications were classified according to Dindo–Clavien scores.7
Statistical analysis
Statistical analysis was performed using spss Version 13.0 (SPSS, Inc., Chicago, IL, USA). Continuous variables were expressed as the median (range) and compared using the Mann–Whitney U-test. Categorical variables were analysed using the chi-squared or Fisher's exact test as indicated. A P-value of <0.05 was considered to indicate statistical significance.
Laparoscopic resection using the ITT technique
Initial (abdominal) laparoscopy
General anaesthesia is induced, routinely using a single lumen endotracheal tube. Single lung ventilation, although generally unnecessary, was used in one case. The patient is positioned in a ‘lazy’, left lateral decubitus position (allowing rotation from almost supine to almost left lateral positions) and secured to the table using beanbags and belts, with the right arm placed in an arm gutter (Fig. 1a).
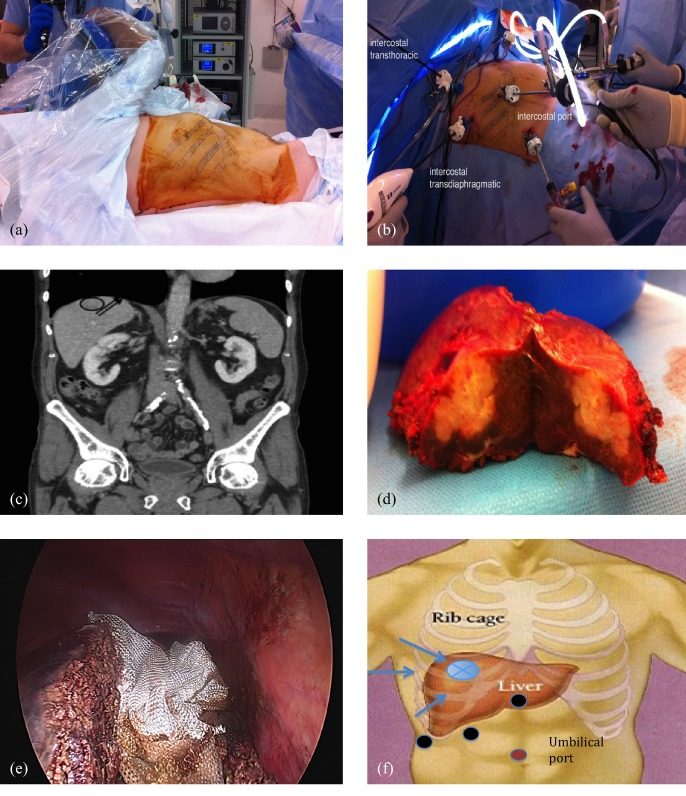
Figure 1.
Resection of dome lesion segment VII. (a) The patient is positioned in a ‘lazy’ left lateral decubitus position. (b) All three levels of intercostal port combined with laparoscopic ports are used in this patient. (c) The position of tumour is observed on a coronal section in computed tomography. The right hepatic vein is marked with two black arrows. (d) The resected specimen. (e) ‘End on’ view obtained with intercostal trocars. (f) Schematic comparison of the positions of standard subcostal trocars (in the standard subcostal laparoscopic approach; black dots) and intercostal trocars (in the intercostal transthoracic trocar approach; blue arrows) for resection of a dome lesion (blue dot). Initial abdominal access is achieved using an umbilical approach (pink dot)
Initial access is obtained by standard abdominal laparoscopic techniques in order to visually assess the liver and its surroundings. The liver can be mobilized as required. Laparoscopic ultrasound is used to define the size and location of hepatic lesions, and their proximity to major vascular structures, and to ensure that an adequate oncologic margin can be obtained.
For large or complex resections, an inflow control sling is placed around the porta hepatis. In the event of significant bleeding during parenchymal transection, a vascular clamp (Eisner USA, LLC, Crystal Lake, IL, USA) can be rapidly applied directly to the porta, using the sling as a guide to prevent damage to the vena cava and the duodenum.
Intercostal ports
Additional 5-mm trocars are inserted through the intercostal spaces to allow instrument access and the use of a 5-mm laparoscope to further assess the dome of the liver.
There are three methods of intercostal port placement, which differ in their relation to the diaphragm: (i) ports can be placed between the ribs below the diaphragm; (ii) ports can be placed between the ribs and through the diaphragm with instrument pressure on the diaphragm imposed from below to push it against the chest wall to ensure that the lung is pushed away and not injured, and (iii) ports can be optically inserted between the ribs into the thoracic cavity and then through the diaphragm. This will require an additional laparoscopic stack, but offers a better view and line of resection for posteromedial tumours.
In the latter two methods, 5-mm balloon ports (Applied Medical Resources Corp., Rancho Santa Margarita, CA, USA) are ideal as the balloon can be inflated and ports retracted, pulling the diaphragm back against the chest wall and enlarging the field of view. All three of these methods may be employed in a single patient depending on the technical requirements of the resection, such as in Fig. 1b. Transiting the chest cavity, as in method (iii), is used for lesions located more posteromedially.
Parenchymal transection
The line of transection is marked with diathermy and parenchymal transection performed with a 5-mm dolphin tip laparoscopic LigaSure™ ‘V’ (Covidien, Inc., Mansfield, MA, USA). This energy device works best when saline is applied simultaneously, which can be done through a suction–irrigation device, or by placing a saline infusion to the port holding the LigaSure™ to allow saline to drip down the device. Saline irrigation allows for clear visualization through the transection plane and also prevents coagulated tissue from adhering to the jaws. The margin is confirmed with laparoscopic ultrasound. Hem-o-Lok® clips (Weck Surgical Instruments, Teleflex Medical, Inc., Durham, NC, USA) can be applied to larger vessels. These also help to define oncologic margins as they are hyperechoic under ultrasound, and allow for the definition of the transection plane, even when the specimen is compressed against the liver.
Port removal
Transdiaphragmatic ports are removed under direct vision. Closure of the diaphragmatic port sites is performed from below, laparoscopically, with non-absorbable sutures after suctioning of the pleural space. The specimen is usually extracted in a retrieval bag through an extension of the 12-mm port at the midline. Drains are not routinely used.
Standard subcostal laparoscopic technique
Initial positioning and subumbilical access are similar to those used in the ITT technique. Additional 5-mm ports are inserted in the epigastric and right subcostal region. A Pringle's sling using a vessel loop secured with a Hem-o-Lok® clip is routinely prepared to guide portal clamping if necessary. Full mobilization of the right lobe of the liver is performed. The margin of the resection is marked under direct ultrasound guidance. Parenchymal transection is performed with a laparoscopic LigaSure™. Larger vessels or bile ducts are clipped with ligaclips, Hem-o-Lok® clips or surgical staplers. The specimen is placed in a retrieval bag and is extracted through a pre-existing scar or an extension of a port site wound. Drains are not routinely placed.
Results
A total of 19 patients underwent laparoscopic resection of dome lesions; the ITT technique was used in eight and the SSL technique in 11 patients. The clinical and tumour characteristics of both groups were similar. The differences in median operating time, blood loss and resection margin were not statistically significant. However, hospital LoS was shorter in the ITT group (Table 1).
Table 1.
Characteristics of patients submitted to laparoscopic liver resections with intercostal transthoracic trocars (ITTs) or a standard subcostal laparoscopic (SSL) technique
| ITT group (n = 8) | SSL group (n = 11) | P-value | |
|---|---|---|---|
| Age, years, median (range) | 61 (25–71) | 66 (53–76) | 0.230 |
| Sex, male, n | 5 | 3 | 0.181 |
| Histology, n | CLM: 5 | CLM: 11 | 0.058 |
| Other malignancy: 3 | |||
| Lesion diameter, mm, median (range) | 20 (6–34) | 26 (10–50) | 0.246 |
| Patients with multiple lesions, n | 1 | 1 | 0.816 |
| Operating time, min, median (range) | 105.0 (50–150) | 115 (45–255) | 0.907 |
| Blood loss, ml, median (range) | 220 (50–300) | 200 (10–1200) | 0.953 |
| Resection margin, mm, median (range) | 3.5 (1–11) | 6 (5–28) | 0.245 |
| Dindo–Clavien classes 1 and 2/3 and 4, n | 0/0 | 2/0 | |
| LoS, days, median (range) | 2 (1–4) | 6 (2–24) | 0.032 |
| Conversions, n | 0 | 2 | 0.485 |
CLM, colorectal liver metastases; LoS, length of hospital stay.
There were no occurrences of lung injury, clinical pneumothorax or significant pleural effusion in the ITT group. No patient suffered severe or chronic pain from the intercostal port sites.
Discussion
This is the first published report to include a detailed technical description of the use of laparoscopy with intercostal transthoracic ports in a series of patients, and to compare the outcomes of this approach with those of standard laparoscopic techniques.
Laparoscopic liver resection has been performed by the present group since 1997; the technique used and the results of laparoscopic right hepatectomy have been published previously.8–10 Like others, the authors had been frustrated by the difficulties of removing small lesions from segments VII and VIII laparoscopically. Options include hand-assisted approaches to pull the liver caudal, but this is not easy, and a hand size incision is needed for a small resection. Other approaches include the use of a formal segmental resection,11,12 which significantly increases the amount of parenchymal sacrifice when performed for small lesions. Other authors11,13–17 have suggested a variety of approaches, each with its own limitations; these are listed in Table 2.
Table 2.
Summary of studies of laparoscopic resection of dome lesions in segments VII and VIII
| Reference | Patients, n | Indication | Tumour location, segment | Method | Type of resection | Lesion size, mm | Operating time, min | Blood loss, ml | Margin |
|---|---|---|---|---|---|---|---|---|---|
| Teramoto et al (2003)13 | 3 | HCC | VIII | Transthoracic/transdiaphragmatic | Wedge resection | 17, 14, 16 | 230, 310, 198 | 50, 650, 450 | Clear |
| Cho et al (2009)11 | 6 | ND | VII, VIII | Conventional laparoscopic | Segmentectomy/tumorectomy | ND | 321.7 | 709.1 | Clear |
| Cheng et al (2011)14 | 1 | HCC | VII | Posterior laparoscopic | Segmentectomy | 26 | 510 | 800 | Clear |
| Ishizawa et al (2012)15 | 7 | ND | VII, VIII | Transthoracic/laparoscopic | Segmentectomy (2 wedge) | ND | 180–240 (seg VII) | 100–1200 (seg VII) | ND |
| 132–240 (seg VIII) | 100–1100 (seg VIII) | ||||||||
| Cloyd & Visser (2012)16 | 2 | HCC | VII, VIII | Transthoracic/transdiaphragmatic | Wedge resection | 21, 30 | ND | ND | Clear |
| Umemura et al (2013)17 | 1 | Metastatic melanoma | VII | Conventional laparoscopic | PLPS | 70 | 291 | 187 | Clear |
| Current series | 8 | Mixed | VII, VIII | Transthoracic/laparoscopic | Wedge resection | 6–34 | 50–150 | 50–300 | Clear |
HCC, hepatocellular carcinoma; ND, not documented; PLPS, pure laparoscopic posterior sectionectomy; Seg, liver segment.
Ishizawa et al.15 previously described a similar technique using an application of the intercostal transdiaphragmatic approach. Upon viewing a video made by one of the authors (Brice Gayet) of this paper,15 the authors were led to attempt and further define this technique. Initial concern was the transgression of another body cavity, which carries attendant risks for bilothorax or oncologic disaster.
However, the technique is remarkably easy and is well tolerated by patients, as long as the surgeon is careful to select small superficial lesions and to continuously confirm the depth of resection with ultrasound. For larger lesions that are closer to the right hepatic vein, it is helpful to enter the chest at a higher point and then to pierce the diaphragm to achieve an even better view. The view and working space can be further improved by using balloon ports to retract the diaphragm.
In an effort to prove the benefits of this approach, the current study compared the initial experience of the present group with that in a series of patients with similarly placed lesions submitted to laparoscopic resection at the study institution prior to the introduction of this new technique. There are obvious limitations to such a comparison because improvements in technology and ability accrue over time. However, even in small numbers, it is apparent that LoS is much improved, which reflects the study group's impression of the ease of this procedure.
The superior visualization offered by the ITT technique can be seen in Fig. 1e. Figure 1f depicts the difference in the access to dome lesions afforded by subcostal and intercostal transthoracic ports, respectively. A short video (Video S1, online) further illustrates the improved views and placement of instruments for resection of these lesions.
Success fuels ambition, but at present the ITT approach remains reserved for lesions of <4 cm in the posterosuperior segments. Larger lesions are generally resected by formal (laparoscopic or open) right hepatectomy.
Conclusions
The use of ITTs for the resection of difficult liver dome lesions is safe, effective and complementary to conventional laparoscopic subcostal approaches. It allows the laparoscopic liver surgeon a broader armamentarium for the resection of these lesions.
Conflicts of interest
None declared.
Supporting Information
Video S1. Video illustrating the improved views and placement of instruments in the resection of dome liver lesions using the intercostal transthoracic trocar approach.
References
- Nguyen KT, Geller DA. Outcomes of laparoscopic hepatic resection for colorectal cancer metastases. J Surg Oncol. 2010;102:975–977. doi: 10.1002/jso.21655. [DOI] [PubMed] [Google Scholar]
- Tranchart H, Di Giuro G, Lainas P, Roudie J, Agostini H, Franco D, et al. Laparoscopic resection for hepatocellular carcinoma: a matched-pair comparative study. Surg Endosc. 2010;24:1170–1176. doi: 10.1007/s00464-009-0745-3. [DOI] [PubMed] [Google Scholar]
- Viganò L, Tayar C, Laurent A, Cherqui D. Laparoscopic liver resection: a systematic review. J Hepatobiliary Pancreat Surg. 2009;16:410–421. doi: 10.1007/s00534-009-0120-8. [DOI] [PubMed] [Google Scholar]
- Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection – 2804 patients. Ann Surg. 2009;250:831–841. doi: 10.1097/SLA.0b013e3181b0c4df. [DOI] [PubMed] [Google Scholar]
- Lai EC, Tang CN, Yang GP, Li MK. Minimally invasive surgical treatment of hepatocellular carcinoma: longterm outcome. World J Surg. 2009;33:2150–2154. doi: 10.1007/s00268-009-0155-7. [DOI] [PubMed] [Google Scholar]
- Strasberg SM. Nomenclature of hepatic anatomy and resections: a review of the Brisbane 2000 system. J Hepatobiliary Pancreat Surg. 2005;12:351–355. doi: 10.1007/s00534-005-0999-7. [DOI] [PubMed] [Google Scholar]
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Rourke N, Fielding G. Laparoscopic right hepatectomy: surgical technique. J Gastrointest Surg. 2004;8:213–216. doi: 10.1016/j.gassur.2003.11.008. [DOI] [PubMed] [Google Scholar]
- O'Rourke N, Shaw I, Nathanson L, Martin I, Fielding G. Laparoscopic resection of hepatic colorectal metastases. HPB. 2004;6:230–235. doi: 10.1080/13651820410023978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dagher I, O'Rourke N, Geller DA, Cherqui D, Belli G, Gamblin TC, et al. Laparoscopic major hepatectomy: an evolution in standard of care. Ann Surg. 2009;250:856–860. doi: 10.1097/SLA.0b013e3181bcaf46. [DOI] [PubMed] [Google Scholar]
- Cho JY, Han HS, Yoon YS, Shin SH. Outcomes of laparoscopic liver resection for lesions located in the right side of the liver. Arch Surg. 2009;144:25–29. doi: 10.1001/archsurg.2008.510. [DOI] [PubMed] [Google Scholar]
- Cho JY, Han HS, Yoon YS, Shin SH. Experiences of laparoscopic liver resection including lesions in the posterosuperior segments of the liver. Surg Endosc. 2008;22:2344–2349. doi: 10.1007/s00464-008-9966-0. [DOI] [PubMed] [Google Scholar]
- Teramoto K, Kawamura T, Takamatsu S, Noguchi N, Nakamura N, Arii S. Laparoscopic and thoracoscopic partial hepatectomy for hepatocellular carcinoma. World J Surg. 2003;27:1131–1136. doi: 10.1007/s00268-003-6936-5. [DOI] [PubMed] [Google Scholar]
- Cheng KC, Yeung YP, Hui J, Ho KM, Yip AW. Multimedia manuscript: laparoscopic resection of hepatocellular carcinoma at segment 7: the posterior approach to anatomic resection. Surg Endosc. 2011;25:3437. doi: 10.1007/s00464-011-1685-2. [DOI] [PubMed] [Google Scholar]
- Ishizawa T, Gumbs AA, Kokudo N, Gayet B. Laparoscopic segmentectomy of the liver: from segment I to VIII. Ann Surg. 2012;256:959–964. doi: 10.1097/SLA.0b013e31825ffed3. [DOI] [PubMed] [Google Scholar]
- Cloyd JM, Visser BC. Video-assisted thoracoscopic transdiaphragmatic liver resection for hepatocellular carcinoma. Surg Endosc. 2012;26:1772–1776. doi: 10.1007/s00464-011-2062-x. [DOI] [PubMed] [Google Scholar]
- Umemura A, Nitta H, Sasaki A, Takahara T, Hasegawa Y, Wakabayashi G. Pure laparoscopic posterior sectionectomy for liver metastasis resulting from choroidal malignant melanoma: a case report. Asian J Endosc Surg. 2013;6:318–321. doi: 10.1111/ases.12043. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video S1. Video illustrating the improved views and placement of instruments in the resection of dome liver lesions using the intercostal transthoracic trocar approach.