Abstract
We analyzed data from the Israeli National Insurance Institute (NII). Autism Spectrum Disorder (ASD) incidence was calculated for all children born in Israel 1992-2009, and by population groups. Overall, 9,109 ASD cases among 2,431,649 children were identified. ASD cumulative incidence by age 8 years increased 10-fold during 2000-2011, from 0.049% to 0.49%, while other child disabilities in NII increased only 1.65-fold. There was a consistent increase in ASD incidence with advancing birth cohorts born 1992-2004, stabilizing among those born 2005-2009. ASD rates among Israeli Arabs were substantially lower, and increased about 10 years later than the general population. The findings suggest a role for ASD awareness, accessing of the government benefit, or the way the concept of ASD is perceived.
Keywords: autism, incidence, prevalence, Israel, sub-populations
Introduction
The reported prevalence and incidence estimates of autism spectrum disorders (ASD) are increasing in the United States, (Developmental Disabilities Monitoring Network Surveillance Year 2010 Principal Investigators & Centers for Disease Control and Prevention 2014; Investigators & Centers for Disease Control and Prevention 2012; Keyes et al. 2012; Schechter & Judith K. Grether 2008; Schieve et al. 2012; Yeargin-Allsopp et al. 2003) Europe, Asia and Australia. (Isaksen, Diseth, Schjølberg, & Skjeldal 2012, 2013; Kawamura, Takahashi, & Ishii 2008; Kim et al. 2011; Leonard et al. 2011; Saemundsen, Magnússon, Georgsdóttir, Egilsson, & Rafnsson 2013; Zaroff & Uhm 2012) Earlier age at diagnosis, diagnostic substitution, increased awareness, environmental factors and diagnostic criteria changes are some of the reasons that have been suggested as explanations for some of this increase. (Croen, Grether, Hoogstrate, & Selvin 2002; Hertz-Picciotto & Delwiche 2009; Hertz-Picciotto 2009; Hoffman, Kalkbrenner, Vieira, & Daniels 2012; King & Bearman 2009; Shattuck 2006) In many Western countries, ascertainment of ASD is associated with socio-demographic and cultural factors, probably due to the influence of awareness and accessibility factors. (Leonard et al. 2011; Pettygrove et al. 2012) This situation limits the ability to conclude whether a real increase in incidence (from biological influences) also contributes to this dramatic increase in reported prevalence and incidence rates. (Fombonne 2001, 2003, 2009; French, Bertone, Hyde, & Fombonne 2013; Isaksen et al. 2013; Wing & Potter 2002)
Most of the incidence studies of ASD were based on subpopulations and/or hospital sources, but several total population studies were published from California, (Keyes et al. 2012) Western Australia, (Nassar et al. 2009) Iceland, (Saemundsen et al. 2013) two counties in Norway(Isaksen et al. 2012) as well as the city of Toyota, Japan. (Kawamura et al. 2008) While these studies each add substantial contribution to the international literature on the epidemiology of ASD, their ability to accurately identify the population at risk, using individual level record linkage and accounting for in- and out-migration and deaths, is limited. In addition, the period covered by the birth cohorts in these studies is typically not long enough to draw conclusions about time trends of ASD incidence.
Israel presents a unique setting in which to examine ASD incidence time trends. Every Israeli-born child gets a unique identification number that stays with him or her for life. In addition, all Israel has had a national health insurance since January 1995, with highly accessible healthcare services from birth to death, including minimal copayment for diagnostic procedures related to ASD. Importantly, since 1981, the Israeli National Insurance Institute (NII) has provided to any Israeli family with a child with a confirmed ASD diagnosis a substantial monetary benefit, independent of eligibility for, or use of, services with ASD. Over the last decades, Israel has undergone a transition from a developing country into a modern life-style, industrial state with a unique multi-ethnic and multi-cultural society. (Rosen, Samuel, & Merkur 2009) There is a large minority of Israeli Arabs (IA) who are distinct by cultural, genetic and socio-demographic factors, more commonly live in rural areas, and have different patterns of health indicators and health care utilization form other Israelis. Another unique sub-population is that of ultra-orthodox Jews (UOJ), who choose to strictly maintain the Jewish religious law and refrain from modern life. For these reasons, these two populations are usually analyzed separately from the general population (GP) in Israel (i.e. those who are not IA or UOJ) with regards to health status when data permits.
A few studies have examined prevalence or incidence time trends of ASD in Israel, using various data sources. (Davidovitch, Hemo, Manning-Courtney, & Fombonne 2013; Gal, Abiri, Reichenberg, Gabis, & Gross 2012; Senecky et al. 2009) None of these studies, however, was able to calculate cumulative incidence rates in the total Israeli-born population while taking into account individual level data regarding population group, death, immigration and emigration. The latter two contribute to accurately calculating the population at risk for incidence rates. For this study, we used the NII data, which integrates individual-level data on all births in Israel, as well as deaths, immigration, emigration and ASD. This unique countrywide data source allowed us to conduct this total population retrospective cohort study, presenting ASD incidence and its time trends for the total population of children born in Israel 1992–2009 and followed until the end of 2011, and to examine the differences in incidence by the major Israeli population groups.
Method
Data source and case ascertainment
The data for this study were collected from the computerized records of the Israeli NII, a welfare governmental organization which is responsible for the social security of the residents of Israel. NII pays benefits to those eligible, assisting people financially at times of personal crisis such as work termination, disability and work injury. (“The National Insurance Institute - Benefits” n.d.) It has branches in all areas of Israel, a website in six languages, and written publications in its branches in Hebrew and Arabic. NII receives data about all births (including home births) from all Israeli hospitals and from the Ministry of Interior. In addition, in order to track payments dues and eligibility for benefits, the NII receives from the Ministry of Interior detailed data on all Israeli residents, including specific dates of migration in and out of Israel and deaths. In this way, NII records continuously track all current and former legal Israeli residents. These individual-level data enabled us to calculate numerators (number of children with ASD) and denominators (population at risk) for each birth cohort, based on actual residence in Israel at each follow up year. Emigration data, however, were unavailable for those who emigrated during 1992-1998, and were scarcely available for those who emigrated during 1999-2004.
A typical diagnosis of ASD in Israel will start by the primary pediatrician referring a child to one of many certified child development centers, where the diagnosis will be made by a multidisciplinary team, based on The Diagnostic and Statistical Manual of Mental Disorders (DSM) criteria. For the period of our study this was the 4th edition, revised (DSM-IV-TR). Once a child is diagnosed with ASD, his parents may submit a claim to NII, which will then be inspected by a NII professional committee on the basis of medical and developmental criteria. These committees, headed by a medical doctor (typically a pediatric psychiatrist or a pediatric neurologist), will either confirm the claim or deny it, based on the medical information from the diagnosing health professionals, submitted by the parents. The committee may ask for additional information, and in rare cases may also examine the child. Parents are allowed to appeal a denial decision. (“The National Insurance Institute - Appealing a decision” n.d.)
Since 2007, NII officially confirms ASD claims according to directions from the Israeli Ministry of Health(Israeli 2007), requiring all of the following criteria to be met:
The diagnosis is made by a pediatric psychiatrist, a pediatric neurologist or a pediatrician with at least 3 years of experience in a certified child development center. The evaluation will include a physical, neurological, and emotional-developmental medical examination.
Assessment by a developmental or a clinical psychologist, using psychological tests according to his functional age.
Inclusion of other health professional as needed.
Using at least one of the following diagnostic tools, according to the child’s age: Autism Diagnostic Interview, DSM IV, Gilliam Autism Rating Scale, Childhood Autism Rating Scale, Autism Diagnostic Observation Schedule, Play Observation Kit.
The professional reports include the diagnostic tools used and the deficiencies found by them.
Once a claim is confirmed, the committee will also decide about the eligibility date for the benefit, which will be the first date of symptoms, but not earlier than one year before the original claim submission date. Internal quality check is done by an NII medical doctor in approximately 5% of the claims.
Case status in this study was based on NII claim confirmations of child disability benefit for ASD. The benefit includes a monthly payment ($610 in 2013, equivalent to 25% of the average salary in Israel, and updated yearly) up to age 18, (“The National Insurance Institute (Disabled child - Benefit Rates)” n.d.) but also makes the parents eligible for substantial discounts in local and state taxes, discounts on electricity bills and other benefits from various public organizations. (“The National Insurance Institute - Take up of Rights (Hebrew)” n.d.) In order to be eligible for benefits, at least one of the parents must be an Israeli resident. Institutionalized children or those who grow up in foster families (a small portion of ASD cases) are not eligible for benefits(“The National Insurance Institute - Disabled child” n.d.), but will be recognized in the NII database as children with ASD if they were moved to a foster family or an institution after their claim to NII was confirmed. In addition, the benefit is independent of income, work, population group or other socio-economic characteristics. The details of these benefits have not changed substantially throughout the study period. NII does not provide any services to children with ASD, nor is the submission of claims for ASD, or the acceptance of claims related to services given by other authorities.
The completeness of ASD ascertainment in NII was confirmed, for the purpose of this study, using the independent database of Maccabi Healthcare Services (MHS), one of four Israeli Health Maintenance Organizations (HMOs) covering approximately 25% of the Israeli population countrywide. Among all children in MHS with an ASD diagnosis between the years 2003-2011 that was validated by a developmental pediatrician (N=1676, birth years 1995-2010), 97.0% (n=1625) were captured in the NII.
Study Population
The study population consisted of all children born in Israel 1992-2009, whose mother was an Israeli resident, and the follow up period was until December 31, 2011. These definitions enabled us to reasonably exclude relevant years before national health coverage was available, and include the last full year for which ASD eligibility dates were available (because a claim can be confirmed up to one year retrospectively). Identification of IA was based on father’s status as specified in their Israeli ID, and identification of UOJ is based on father’s or siblings’ studies at a religious college (“Yeshiva”), as these individuals are given a discount for NII premiums.
Statistical methods
We took a birth cohort approach, calculating incidence separately for each birth cohort at the end of each calendar year follow up, as the percentage of newly confirmed ASD cases from the birth cohort for that calendar year, among the relevant population at risk. The population at risk for a certain birth cohort and a certain follow up year was defined as the original number of children born in Israel at a given year, minus the number of children who died, left the country or were already diagnosed with ASD in previous years. Cumulative incidence for a certain birth cohort and a certain follow up year was defined as the sum of incidence for that follow up year and for all previous follow up years for that cohort. Calculation of incidence of other (non-ASD) child disabilities was done similarly. Incidence is presented first for the total population, and is further stratified by the three major population groups: IA, UOJ and the remaining majority (termed GP in this paper). Confidence intervals were not calculated since total population data is presented. Sex ratio of ASD cases was defined as the number of male ASD cases divided by the number of female ASD cases.
We analyzed time trends using general additive models with thin plate regression splines to allow for non-linear associations using R version 3.1.1 with package mgcv. (Wood 2012). The time trend of the sex ratio of ASD cases at age 8 was analyzed with year as the only predictor. Differences between population groups in time trends of cumulative incidence of ASD and, separately, other child disabilities, by age 8 were analyzed in models of incidence rate that included year and population group as predictors, and a multiplicative interaction term between those two variables.
Results
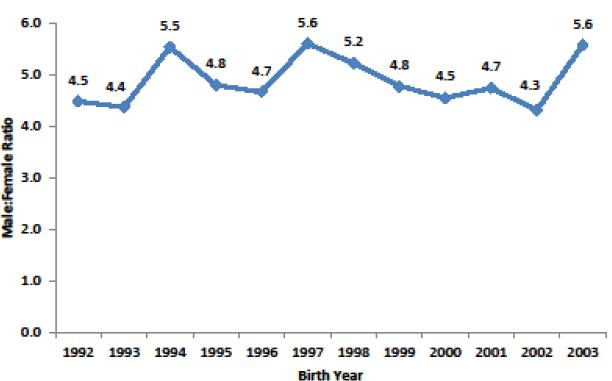
2,431,649 children were born in Israel during 1992-2009 (incidence analyses population), 28% of them were UOJ and 18% IA, with the rest (54%) comprising the GP. Among these children, 9,109 had ASD (Table 1). When examining the increase in cumulative incidence at age 8 throughout 1992-2003 birth cohorts followed until 2011, ASD increased 10-fold (from 0.049% to 0.49%) while NII non-ASD child disability benefits increased 1.65-fold (from 0.90% to 1.49%) (Figure 1). When stratifying cumulative incidence at age 8 by population groups, the time trend for other (non-ASD) child disabilities did not vary significantly among the three groups (p>0.1), while the time trend for ASD was significantly different for IA (p<0.001) but not for UOJ (p>0.1) in comparison with the GP (Online Resource 1). The sex ratio of ASD cases at age 8 generally remained stable throughout those years, ranging from 4.4-5.6 without a consistent time trend (p=0.54; Figure 2).
Table 1. Study population by group and gender: total population born in Israel, 1992-2009, followed until end of 2011.
| Total population | ASD cases | ||||
|---|---|---|---|---|---|
|
|
|||||
| N | % of total | N | % of total | ||
|
|
|||||
| Sex | Boys | 1,247,552 | 51% | 7,611 | 84% |
| Girls | 1,184,097 | 49% | 1,498 | 16% | |
|
Population
Group |
GP | 1,326,303 | 54% | 7,469 | 82% |
| IA | 674,679 | 18% | 584 | 6% | |
| UOJ | 430,667 | 28% | 1,056 | 12% | |
| Total | 2,431,649 | 100% | 9,109 | 100% | |
Abbreviations: ASD = Autism spectrum disorders; IA = Israeli Arabs; UOJ = Ultra-orthodox Jews; GP = General population (total population, excluding IA and UOJ).
Figure 1.
Cumulative incidence of ASD and non-ASD child disability benefits at NII at age 8 in the total population born in Israel 1992-2003 by birth year, as a percentage of 1992 cumulative incidence. ASD = Autism spectrum disorders; NII = National Insurance Institute of Israel.
Figure 2.
Male:Female ratio of autism spectrum disorders cases at age 8, total population born in Israel, 1992-2003.
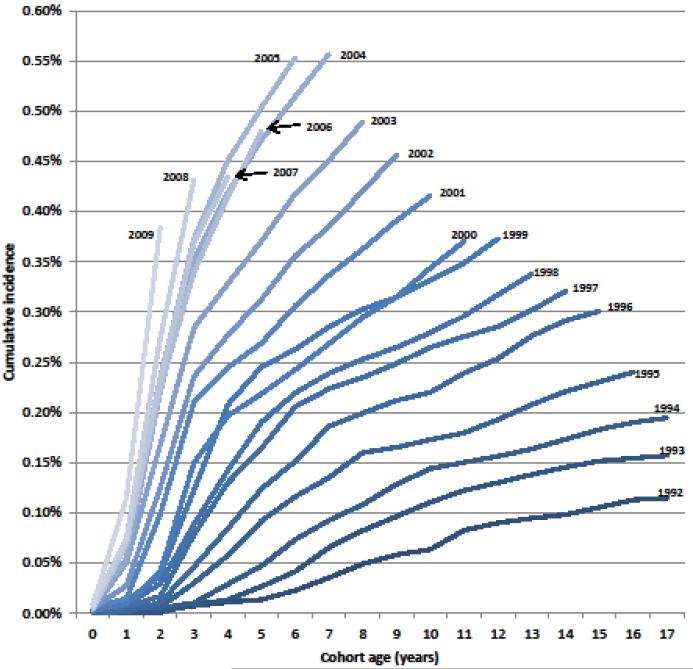
A steep and consistent increase in cumulative incidence of ASD is evident with advancing birth cohorts among children born 1992-2004, evidenced by lines that get steeper and end at higher incidence with advancing birth cohort year (figure 3). For those born 2005-2009, despite different follow-up periods, the incidence is almost identical when compared at the same ages, resulting in lines that generally overlap, suggesting stabilization of incidence among those birth cohorts (Figure 3). The age at which most cases were diagnosed gradually got younger over time as can be seen by the year in which the greatest rise in cumulative incidence occurs. For example, in the 1995 birth cohort, the diagnoses occurred most between the ages of 3-8 years, compared to ages 2-3 years for later birth cohorts.
Figure 3.
Cumulative incidence of Autism spectrum disorders in the total population born in Israel, 1992-2009. Different lines represent different birth cohorts, and are ordered from darkest to brightest. The birth cohort is noted at the end of each line, where the data for that year ends. The age of the children (cohort age) is indicated on the x-axis.
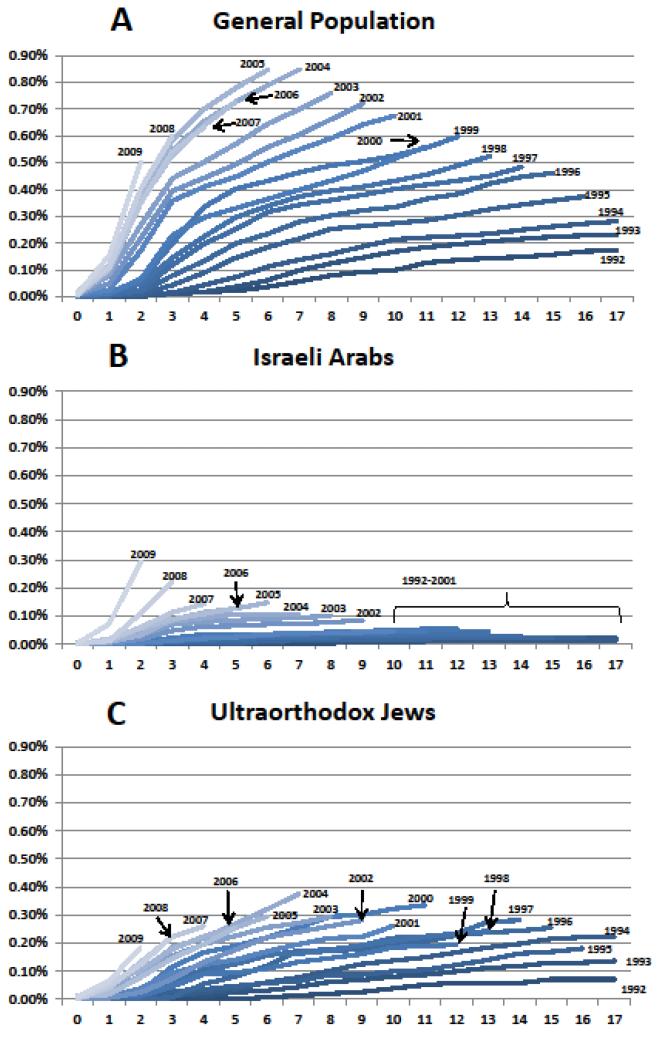
When stratifying cumulative incidence of ASD by population groups (Figure 4), there was a substantially lower incidence among the two minority groups, IA and UOJ, compared with the GP. While the GP demonstrates similar time trends as the total population, with a very steep increase during 1992-2004, but with higher incidence (peaking at 0.85% at cohort age 7 for children born in 2004, Figure 4A), the incidence among IA starts to rise steeply only for birth cohorts 2002-2009, reaching a peak of 0.29% at cohort age 2 for children born in 2009 (figure 4B). The cumulative incidence in IA at cohort age two increased 37-fold within 10 years (1999-2009) and fivefold within the last two years (2007-2009). The Incidence time trend among UOJ is somewhat similar to that of the GP, although the increase is less consistent after 1996, and the incidence rates remain lower, peaking at 0.37% at cohort age 7 for children born in 2004 (Figure 4C). Incidence time trends in IA and UOJ are more obvious when scaling the Y axis appropriately for their lower incidence levels (Online Resource 2).
Figure 4.
Cumulative incidence of autism spectrum disorders in the total population born in Israel 1992-2009, by birth cohort and population group. X axes represent cohort age (in years), Y axes represent cumulative incidence. Different lines represent different birth cohorts, and are ordered from darkest to brightest. The birth cohort is noted at the end of each line, where the data for that year ends. Y axes are kept in the same scale, for correct comparison of cumulative incidence levels. (A) General Population: Total population excluding Israeli Arabs and ultraorthodox Jews. (B) Israeli Arabs. (C) Ultraorthodox Jews.
Discussion
We found that in 2011, the cumulative incidence of ASD among the total population of 8 year olds born in Israel was 0.49% (1 in 203 children). This estimate is on the lower end of a survey of 11 US states in 2010 that used the same age grouping (Developmental Disabilities Monitoring Network Surveillance Year 2010 Principal Investigators & Centers for Disease Control and Prevention 2014) and is closer to recent estimates from samples in Europe, Japan and Canada (Norway: 0.51%; Portugal: 0.17%; United Kingdom: 0.22%, 0.39%; Sweden: 0.35%; Canada: 0.25%, 0.22%; Japan: 0.38%). (Baird et al. 2006; Gillberg, Cederlund, Lamberg, & Zeijlon 2006; Honda, Shimizu, & Rutter 2005; Isaksen et al. 2012; Lazoff, Zhong, Piperni, & Fombonne 2010; Oliveira et al. 2007; Williams, Thomas, Sidebotham, & Emond 2008) However, the exact age ranges considered for these estimates differed somewhat and so these comparisons are not exact. (French et al. 2013)
Our incidence estimates present a large increase in the incidence of diagnosed ASD in Israel, consistent with ASD incidence trends in other countries. (Gurney et al. 2003; Investigators & Centers for Disease Control and Prevention 2012; Kawamura et al. 2008; Keyes et al. 2012; Nassar et al. 2009; Saemundsen et al. 2013; Yeargin-Allsopp et al. 2003) This increase is not a part of a general increase in childhood disability benefits given by NII as its trends are dramatically distinct from other child disabilities. Among the GP most of the increase happens between birth cohorts 1992-2004, and little further rise in incidence rate is seen after that. The UOJ show a less consistent time trend, and the IA population presents a dramatic increase much later in time (relative to the GP), starting around 2002. This is the first report of which we are aware suggesting that the rising rates of ASD are levelling off, albeit we see this in the GP group only and not in the Israeli minority groups.
Previous studies that examined the country-wide prevalence and incidence of ASD in Israel have also indicated increases although these studies had limitations. An early study with NII data reported peak incidence of 0.019% of the children up to age 14 for the year 2004. (Senecky et al. 2009) This relatively low incidence can be explained by the early years this study covered, and the usage of questionable denominators, as noted in a later report. (Gal & Gross 2010) Another study with cases identified from the Israeli Ministry of Social Affairs (MOSA) registry, used birth cohort denominators from the Israeli Central Bureau of Statistics to calculate ASD prevalence in 2009 for children born in Israel 1986-2005. (Gal et al. 2012) The study reported a gradually increasing prevalence time trend, peaking at 0.36% for children born 2003. The limitations of this study were noted by the authors, and include: incomplete case registration at MOSA, problematic denominators (that do not take into account immigration and emigration, as well as death beyond the first year of life), no distinction between UOJ and the remaining GP, and the probable influence of time-varying MOSA benefits on case ascertainment. (Gal et al. 2012) Immigration is especially important, since there were substantial immigration waves to Israel during the last decades, and the documented prevalence of ASD in those immigrants was shown to be much lower. (Kamer et al. 2004) Most notably, though, MOSA data is based on requests for service that can be affected by eligibility for services, rather than the service eligibility-independent financial benefit of the NII that essentially requires only a verified medical diagnosis. The last paper to examine the issue in Israel was based on HMO data and demonstrated increasing cumulative incidence with advancing birth cohorts (born 2002-2006), but was limited only to those children who were members with that HMO (~25% of the relevant population) and some of the ASD diagnoses outside the HMO may not have been captured. (Davidovitch et al. 2013)
As with previous incidence studies, this study cannot give a definite answer regarding the factors that drive ASD incidence up so sharply. However, the distinct time trends among the different Israeli sub-populations do not seem compatible with changes in an Israel-wide environmental factor driving the increase. Since UOJ and IA live with the GP in many “mixed” Israeli urban areas, it seems unlikely that these time trends would be driven mainly by such Israel-wide environmental exposures. A contribution from environmental factors would have to relate to exposures experienced separately, and with distinct temporal patterns, by the different groups. Expanding diagnostic criteria and diagnostic substitutions could possibly contribute to some of the rise in incidence. However, the medical community serving these populations is to a large degree, although not completely, overlapping. Thus, such changes might be expected to affect all the sub-populations similarly rather than with distinct temporal patterns as we found. Differences in awareness, accessing of the government benefit, or the way the concept of ASD is perceived or accepted by the different groups may be the most likely explanation of a major component of the rise in incidence rates.
The IA population is an ethnic minority in Israel, and the UOJ population is a cultural minority that chooses to strictly maintain the Jewish religious law and distinguish themselves from modern life. Traditionally, mental disorders in these populations may be stigmatized and, especially in the UOJ population, might also negatively affect other family members’ arranged marriage processes. (Manor-Binyamini 2012; Shaked & Bilu 2006) IA and UOJ populations also tend to have lower trust in state agencies, and might minimize their contact with government institutions. These factors might reduce ascertainment of ASD in those communities and their awareness of the relevant benefit. On the other hand, both UOJ and IA have, on average, much lower income, so the disability benefit given for ASD (independently of income or other parameters) should be especially important for them. To the extent that differences in awareness or acceptance of ASD in the different Israeli sub-populations explain the differences in incidence time trends, this would suggest health and welfare disparities, despite universal health and insurance coverage. This emphasizes the need to strengthen efforts to minimize disparities, raising awareness and increase access to ASD diagnosis and services in the minority groups in Israel and in other countries.
A limitation of our study is the lack of codified criteria for the confirmation of ASD disability claims in the NII until 2007. However, our validation sub-study using MHS data showed that almost all (97%) of the children with confirmed ASD are captured in the NII database. In addition, if lack of codified criteria had a strong effect on case ascertainment we would have expected to see inflections at the point of codification in the different birth cohort lines, i.e. approximately 4 years before the end of each line (corresponding to 2007 for each birth cohort), but we did not. This suggests that there were no major changes introduced at the time of the codification of official criteria in 2007 or other possible point changes. Another limitation was that we did not have complete emigration data for the whole study period. However, the numbers of emigrating children was very small (no more than 600 per birth cohort per year) even in those years with complete data. Additionally, detailed data about ASD subtypes and medical diagnoses given to children with other child disabilities were not available at NII. The lack of these data restricted our ability to examine the incidence of various ASD subtypes (as defined in the era of DSM-IV) and to make comparisons of ASD incidence time trends with other specific disabilities (e.g. intellectual disability).
In comparison to previous studies from Israel and other countries, our study has the advantages of (a) showing total population data, (b) using a comprehensive national database of ASD cases, based on medical diagnoses rather than requests for services, (c) being able to define the population at risk using individual birth, immigration, emigration and death data, (d) stratifying reliably by major population groups, and (e) covering a long enough follow up time to isolate increasing incidence from earlier age of diagnosis (since follow up for most birth cohorts continued up to ages where very few children are diagnosed). These features minimize possible selection and information biases, and strengthen the internal validity of the study.
Our findings indicate a sharp rise in ASD incidence rates over time in Israel with a timing that differs by different Israeli sub-populations. Intriguingly, among the GP the rise in rates appears to end around 2004. The difference in timing of the trends by sub-population is compatible with differences in awareness or acceptance of ASD in the different groups playing an important role in the rising incidence trends. This does not mean that environmental agents, as well as genetic factors, do not have important roles in ASD, and further research into these possible risk factors for ASD is needed. The distinct cultural and genetic differences of the Israeli population may make this a particularly fruitful country for such research. The established database will serve us as a valuable infrastructure to study risk factors of ASD.
Supplementary Material
Acknowledgements
We wish to thank Daniel Gottlieb, Rivka Prior, Alex Gealia, Alina Milkin and Meira Schwartz from the Israeli National Insurance Institute for insightful discussions and assistance in data collection.
Acknowledgement and financial disclosures: This study was supported by the Environment and Health Fund (EHF, Israel), the Harvard-NIEHS center (P30-ES000002), and Mr. James Crystal in honor of Mrs. Lillian Yaros. Drs. Raz, Weisskopf and Levine, and Mr. Pinto report no other biomedical financial interests or potential conflicts of interest. We wish to thank Daniel Gottlieb, Rivka Prior, Alex Gealia, Alina Milkin and Meira Schwartz from the Israeli National Insurance Institute for insightful discussions and assistance in data collection.
Contributor Information
Dr. Raanan Raz, Department of Environmental Health at Harvard School of Public Health., Boston, MA, USA.
Dr. Marc G Weisskopf, Departments of Environmental Health and Epidemioloy at Harvard School of Public Health., Boston, MA, USA.
Dr. Michael Davidovitch, Department of Child Development, Medical Division, Maccabi Healthcare Services, Tel Aviv, Israel.
Mr. Ofir Pinto, Israeli National Insurance Institute in Jerusalem.
Dr. Hagai Levine, Braun School of Public Health and Community Medicine, Hebrew University-Hadassah, Jerusalem.
References
- Baird G, Simonoff E, Pickles A, Chandler S, Loucas T, Meldrum D, Charman T. Prevalence of disorders of the autism spectrum in a population cohort of children in South Thames: the Special Needs and Autism Project (SNAP) Lancet. 2006;368(9531):210–5. doi: 10.1016/S0140-6736(06)69041-7. doi:10.1016/S0140-6736(06)69041-7. [DOI] [PubMed] [Google Scholar]
- Croen L. a, Grether JK, Hoogstrate J, Selvin S. The changing prevalence of autism in California. J Autism Dev Disord. 2002;32(3):207–15. doi: 10.1023/a:1015453830880. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12757365. [DOI] [PubMed] [Google Scholar]
- Davidovitch M, Hemo B, Manning-Courtney P, Fombonne E. Prevalence and incidence of autism spectrum disorder in an Israeli population. J Autism Dev Disord. 2013;43(4):785–93. doi: 10.1007/s10803-012-1611-z. doi:10.1007/s10803-012-1611-z. [DOI] [PubMed] [Google Scholar]
- Developmental Disabilities Monitoring Network Surveillance Year 2010 Principal Investigators. Centers for Disease Control and Prevention Prevalence of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2010. Morbidity and mortality weekly report. Surveillance summaries (Washington, D.C.: 2002) 2014;63(Suppl 2(2)):1–21. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/24670961. [PubMed] [Google Scholar]
- Fombonne E. Is there an epidemic of autism? Pediatrics. 2001;107(2):411–2. doi: 10.1542/peds.107.2.411. Retrieved from http://pediatrics.aappublications.org/content/107/2/411.short. [DOI] [PubMed] [Google Scholar]
- Fombonne E. The prevalence of autism. JAMA. 2003;289(1):87–9. doi: 10.1001/jama.289.1.87. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/22836322. [DOI] [PubMed] [Google Scholar]
- Fombonne E. Commentary: on King and Bearman. Int J Epidemiol. 2009;38(5):1241–2. doi: 10.1093/ije/dyp259. author reply 1243-4. doi:10.1093/ije/dyp259. [DOI] [PubMed] [Google Scholar]
- French LR, Bertone A, Hyde KL, Fombonne E. Epidemiology of Autism Spectrum Disorders. In The Neuroscience of Autism Spectrum Disorders. 2013:3–24. Elsevier. doi:10.1016/B978-0-12-391924-3.00001-6. [Google Scholar]
- Gal G, Abiri L, Reichenberg A, Gabis L, Gross R. Time trends in reported autism spectrum disorders in Israel, 1986-2005. J Autism Dev Disord. 2012;42(3):428–431. doi: 10.1007/s10803-011-1252-7. doi:10.1007/s10803-011-1252-7. [DOI] [PubMed] [Google Scholar]
- Gal G, Gross R. Time trends in autism. Isr Med Assoc J. 2010;12(11):711–2. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/23959427. [PubMed] [Google Scholar]
- Gillberg C, Cederlund M, Lamberg K, Zeijlon L. Brief report: “the autism epidemic”. The registered prevalence of autism in a Swedish urban area. Journal of autism and developmental disorders. 2006;36(3):429–35. doi: 10.1007/s10803-006-0081-6. doi:10.1007/s10803-006-0081-6. [DOI] [PubMed] [Google Scholar]
- Gurney JG, Fritz MS, Ness KK, Sievers P, Newschaffer CJ, Shapiro EG. Analysis of prevalence trends of autism spectrum disorder in Minnesota. Arch Pediatr Adolesc Med. 2003;157(7):622–7. doi: 10.1001/archpedi.157.7.622. doi:10.1001/archpedi.157.7.622. [DOI] [PubMed] [Google Scholar]
- Hertz-Picciotto I. Commentary: Diagnostic change and the increased prevalence of autism. Int J Epidemiol. 2009;38(5):1239–41. doi: 10.1093/ije/dyp258. author reply 1243-4. doi:10.1093/ije/dyp258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hertz-Picciotto I, Delwiche L. The rise in autism and the role of age at diagnosis. Epidemiology. 2009;20(1):84–90. doi: 10.1097/EDE.0b013e3181902d15. doi:10.1097/EDE.0b013e3181902d15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman K, Kalkbrenner AE, Vieira VM, Daniels JL. The spatial distribution of known predictors of autism spectrum disorders impacts geographic variability in prevalence in central North Carolina. Environ Health. 2012;11(1):80. doi: 10.1186/1476-069X-11-80. doi:10.1186/1476-069X-11-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honda H, Shimizu Y, Rutter M. No effect of MMR withdrawal on the incidence of autism: a total population study. Journal of child psychology and psychiatry, and allied disciplines. 2005;46(6):572–9. doi: 10.1111/j.1469-7610.2005.01425.x. doi:10.1111/j.1469-7610.2005.01425.x. [DOI] [PubMed] [Google Scholar]
- Investigators, A. and D. D. M. N. S. Y. 2008 P. Centers for Disease Control and Prevention Prevalence of autism spectrum disorders--Autism and Developmental Disabilities Monitoring Network, 14 sites, United States, 2008. Centers for Disease Control and Prevention. Morbidity and mortality weekly report. Surveillance summaries (Washington, D.C.: 2002) 2012;61(3):1–19. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/22456193. [PubMed] [Google Scholar]
- Isaksen J, Diseth TH, Schjølberg S, Skjeldal OH. Observed prevalence of autism spectrum disorders in two Norwegian counties. Eur J Paediatr Neurol. 2012;16(6):592–8. doi: 10.1016/j.ejpn.2012.01.014. doi:10.1016/j.ejpn.2012.01.014. [DOI] [PubMed] [Google Scholar]
- Isaksen J, Diseth TH, Schjølberg S, Skjeldal OH. Autism Spectrum Disorders - Are they really epidemic? Eur J Paediatr Neurol. 2013;17(4):327–33. doi: 10.1016/j.ejpn.2013.03.003. doi:10.1016/j.ejpn.2013.03.003. [DOI] [PubMed] [Google Scholar]
- Israeli A. Ministry of Health; Israel: 2007. Diagnosis of children suffering from autism PDD (the autism spectrum) Retrieved from http://www.health.gov.il/hozer/mk13_2007.pdf. [Google Scholar]
- Kamer a, Zohar a H., Youngmann R, Diamond GW, Inbar D, Senecky Y. A prevalence estimate of pervasive developmental disorder among immigrants to Israel and Israeli natives-a file review study. Soc Psychiatry Psychiatr Epidemiol. 2004;39(2):141–5. doi: 10.1007/s00127-004-0696-x. doi:10.1007/s00127-004-0696-x. [DOI] [PubMed] [Google Scholar]
- Kawamura Y, Takahashi O, Ishii T. Reevaluating the incidence of pervasive developmental disorders: impact of elevated rates of detection through implementation of an integrated system of screening in Toyota, Japan. Psychiatry Clin Neurosci. 2008;62(2):152–9. doi: 10.1111/j.1440-1819.2008.01748.x. doi:10.1111/j.1440-1819.2008.01748.x. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Susser E, Cheslack-Postava K, Fountain C, Liu K, Bearman PS. Cohort effects explain the increase in autism diagnosis among children born from 1992 to 2003 in California. Int J Epidemiol. 2012;41(2):495–503. doi: 10.1093/ije/dyr193. doi:10.1093/ije/dyr193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim YS, Leventhal BL, Koh Y, Laska E, Lim E, Kim S, Grinker RR. Prevalence of Autism Spectrum Disorders in a Total Population Sample. Am J Psychiatry. 2011;168:904–912. doi: 10.1176/appi.ajp.2011.10101532. [DOI] [PubMed] [Google Scholar]
- King M, Bearman P. Diagnostic change and the increased prevalence of autism. Int J Epidemiol. 2009;38(5):1224–34. doi: 10.1093/ije/dyp261. doi:10.1093/ije/dyp261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazoff T, Zhong L, Piperni T, Fombonne E. Prevalence of pervasive developmental disorders among children at the English Montreal School Board. Canadian journal of psychiatry. Revue canadienne de psychiatrie. 2010;55(11):715–20. doi: 10.1177/070674371005501105. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/21070699. [DOI] [PubMed] [Google Scholar]
- Leonard H, Glasson E, Nassar N, Whitehouse A, Bebbington A, Bourke J, Stanley F. Autism and intellectual disability are differentially related to sociodemographic background at birth. PloS one. 2011;6(3):e17875. doi: 10.1371/journal.pone.0017875. doi:10.1371/journal.pone.0017875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manor-Binyamini I. Parental coping with developmental disorders in adolescents within the ultraorthodox Jewish community in Israel. Journal of autism and developmental disorders. 2012;42(5):815–26. doi: 10.1007/s10803-011-1313-y. doi:10.1007/s10803-011-1313-y. [DOI] [PubMed] [Google Scholar]
- Nassar N, Dixon G, Bourke J, Bower C, Glasson E, de Klerk N, Leonard H. Autism spectrum disorders in young children: effect of changes in diagnostic practices. Int J Epidemiol. 2009;38(5):1245–54. doi: 10.1093/ije/dyp260. doi:10.1093/ije/dyp260. [DOI] [PubMed] [Google Scholar]
- Oliveira G, Ataíde A, Marques C, Miguel TS, Coutinho AM, Mota-Vieira L, Vicente AM. Epidemiology of autism spectrum disorder in Portugal: prevalence, clinical characterization, and medical conditions. Developmental medicine and child neurology. 2007;49(10):726–33. doi: 10.1111/j.1469-8749.2007.00726.x. doi:10.1111/j.1469-8749.2007.00726.x. [DOI] [PubMed] [Google Scholar]
- Pettygrove S, Pinborough-Zimmerman J, John Meaney F, Van Naarden Braun K, Nicholas J, Miller L, Rice C. Predictors of Ascertainment of Autism Spectrum Disorders Across Nine US Communities. J Autism Dev Disord. 2012 doi: 10.1007/s10803-012-1732-4. doi:10.1007/s10803-012-1732-4. [DOI] [PubMed] [Google Scholar]
- Rosen B, Samuel H, Merkur ES. Israel: Health system review. Health Systems in Transition. 2009;11(2):1–226. [PubMed] [Google Scholar]
- Saemundsen E, Magnússon P, Georgsdóttir I, Egilsson E, Rafnsson V. Prevalence of autism spectrum disorders in an Icelandic birth cohort. BMJ open. 2013;3(6):1–6. doi: 10.1136/bmjopen-2013-002748. doi:10.1136/bmjopen-2013-002748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schechter R, Judith K. Grether. Continuing Increases in Autism Reported to California’s Developmental Services System. Arch Pediatr Adolesc Med. 2008;65(1):19–24. doi: 10.1001/archgenpsychiatry.2007.1. [DOI] [PubMed] [Google Scholar]
- Schieve L. a, Rice C, Yeargin-Allsopp M, Boyle C. a, Kogan MD, Drews C, Devine O. Parent-reported prevalence of autism spectrum disorders in US-born children: an assessment of changes within birth cohorts from the 2003 to the 2007 National Survey of Children’s Health. Matern Child Health J. 2012;16(Suppl 1):S151–7. doi: 10.1007/s10995-012-1004-0. doi:10.1007/s10995-012-1004-0. [DOI] [PubMed] [Google Scholar]
- Senecky Y, Chodick G, Diamond G, Lobel D, Drachman R, Inbar D. Time trends in reported autistic spectrum disorders in Israel, 1972-2004. Isr Med Assoc J. 2009;11(1):30–3. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/19344009. [PubMed] [Google Scholar]
- Shaked M, Bilu Y. Grappling with affliction: autism in the Jewish ultraorthodox community in Israel. Culture, medicine and psychiatry. 2006;30(1):1–27. doi: 10.1007/s11013-006-9006-2. doi:10.1007/s11013-006-9006-2. [DOI] [PubMed] [Google Scholar]
- Shattuck PT. The contribution of diagnostic substitution to the growing administrative prevalence of autism in US special education. Pediatrics. 2006;117(4):1028–37. doi: 10.1542/peds.2005-1516. doi:10.1542/peds.2005-1516. [DOI] [PubMed] [Google Scholar]
- The National Insurance Institute Appealing a decision. (n.d.) Retrieved November 19, 2013, from http://www.btl.gov.il/EnglishHomepage/Benefits/Disabledchild/Pages/Appealingadecision.aspx.
- The National Insurance Institute Benefits. (n.d.) Retrieved November 19, 2013, from http://www.btl.gov.il/EnglishHomepage/Benefits/Pages/default.aspx.
- The National Insurance Institute Disabled child. (n.d.) Retrieved November 19, 2013, from http://www.btl.gov.il/EnglishHomepage/Benefits/Disabledchild/Pages/default.aspx.
- The National Insurance Institute Take up of Rights (Hebrew). (n.d.) Retrieved November 19, 2013, from http://www.btl.gov.il/AllRights/Pages/mosdot.aspx.
- The National Insurance Institute (Disabled child - Benefit Rates). (n.d.) Retrieved November 19, 2013, from http://www.btl.gov.il/EnglishHomepage/Benefits/Disabledchild/Pages/BenefitRates.aspx.
- Williams E, Thomas K, Sidebotham H, Emond A. Prevalence and characteristics of autistic spectrum disorders in the ALSPAC cohort. Developmental medicine and child neurology. 2008;50(9):672–7. doi: 10.1111/j.1469-8749.2008.03042.x. doi:10.1111/j.1469-8749.2008.03042.x. [DOI] [PubMed] [Google Scholar]
- Wing L, Potter D. The epidemiology of autistic spectrum disorders: is the prevalence rising? Ment Retard Dev Disabil Res Rev. 2002;8(3):151–61. doi: 10.1002/mrdd.10029. doi:10.1002/mrdd.10029. [DOI] [PubMed] [Google Scholar]
- Wood S. 2012 Package mgcv. Retrieved from http://cran.r-project.org/web/packages/mgcv/index.html.
- Yeargin-Allsopp M, Rice C, Karapurkar T, Doernberg N, Boyle C, Murphy C. Prevalence of autism in a US metropolitan area. JAMA. 2003;289(1):49–55. doi: 10.1001/jama.289.1.49. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12503976. [DOI] [PubMed] [Google Scholar]
- Zaroff CM, Uhm SY. Prevalence of autism spectrum disorders and influence of country of measurement and ethnicity. Soc Psychiatry Psychiatr Epidemiol. 2012;47(3):395–8. doi: 10.1007/s00127-011-0350-3. doi:10.1007/s00127-011-0350-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.