Abstract
OBJECTIVES:
As Afghans make up the largest group of foreign nationals in Iran, the aim of this study was to assess the proportion of Afghan immigrants among those afflicted by the most prevalent infectious diseases in Iran.
METHODS:
National and international online scientific databases were searched through November 2013. The reference lists of included studies were also searched. All descriptive studies concerning the most common infectious diseases in Iran, including tuberculosis, multiple-drug-resistant tuberculosis, malaria, cholera, Crimean-Congo hemorrhagic fever, leishmaniasis, and hepatitis B were retrieved. The nationality of patients was not considered. The selection of studies and data extraction was performed separately by two authors. Results were reported using a random effect model with a 95% confidence interval (CI).
RESULTS:
The overall proportion of Afghan immigrants with the aforementioned infectious diseases was 29% (95% CI, 21 to 37). According to a stratified analysis, the proportion of Afghan immigrants afflicted with tuberculosis was (29%), multiple-drug-resistant tuberculosis (56%), malaria (40%), cholera (8%), Crimean-Congo hemorrhagic fever (25%), leishmaniasis (7%), and hepatitis B (14%).
CONCLUSIONS:
It is highly recommended to monitor the health status of the Afghan immigrants when entering Iran, to reduce the spread of communicable diseases, which are viewed as serious in international health regulations.
Keywords: Afghan, Immigrant, Infection, Health, Systematic review, Iran
INTRODUCTION
According to statistics released by the United Nations in 2013, an estimated 232 million people were classified as immigrants. This amounts to approximately three percent of the world’s population [1]. Illegal immigration is considered a punishable crime by many governments [2]. Illegal immigrants, also referred to as undocumented immigrants, constitute, under certain conditions, a refugee population in a host country. Since reliable statistics are not available regarding undocumented immigration, it can only be estimated that about twenty to thirty million illegal immigrants exist worldwide [3]. Afghans account for the majority of the immigrants in Iran [4].
After Iraq and Turkmenistan, Afghanistan shares the longest border with Iran. Due to the occupation of Afghanistan by the Union of Soviet Socialist Republics between 1980 and 1989 and subsequent internal wars in Afghanistan, around 2.9 million Afghans have immigrated to Iran [5]. Over recent years, although a myriad of encouragements as well as threats have been presented to these nationals to return to Afghanistan, the repatriation process has been extremely slow. Poverty, unemployment, and a lack of security in Afghanistan are among the most important factors that prevent Afghans from returning to their own country. The Iranian government began implementing plans for Afghans’ gradual return in 1995 after the exit of the Soviet Union from Afghanistan. In a census conducted in 2001, 2.5 million foreign nationals were counted, and by 2007, this figure had decreased to one million. Of these, more than 940,000 were Afghan. However, this figure reflects the official statistics; the number of undocumented nationals is much higher [5,6]. Four hundred thousand Afghan residents are born in Iran and the mean duration of their residence is over fifteen years [7].
In spite of the longstanding presence of Afghan immigrants, they remain in the lower levels of social, political, and economic life in Iran. Afghan immigrants in Iran work predominantly in jobs requiring few or no skills [8].
The presence of these foreign nationals has imposed multiple challenges, such as new health risks, social problems, and cultural incompatibilities. Among these challenges, the spread of infectious disease is a significant problem [9,10].
Immigration can negatively affect the state of health of immigrants, because of the lack of availability of health services [11]. The Iranian government has practiced health surveillance and treatment of all foreign nationals regardless of their nationality. Immigration, particularly of Afghans, has been associated with an increase in the number of reports of some diseases in Iran. Since the first wave of Afghan immigrants came to Iran (more than 30 years ago), immigrants have had access to essential health care and, education services [12].
According to the World Health Organization (WHO) report, the burden of most infectious diseases, including tuberculosis (TB), leishmaniasis, and malaria, in Afghanistan is greater than in Iran [13-15].
Several studies concerning infectious diseases conducted in Iran have addressed the proportion of Afghan immigrants among the patients. However, results have been inconsistent, and thus there is no accurate estimation of Afghan immigrants with infectious diseases in Iran. The aim of this meta-analysis was to estimate the overall proportion of Afghan immigrants with infectious diseases in Iran.
MATERIALS AND METHODS
To conduct this study, the list of all major infectious diseases that Afghans could potentially be infected with was drawn up. This list was extracted via a web-based search and a primary search of related articles. Using the Delphi method and after consulting with ten experts in the Ministry of Health of Iran, the infectious diseases of greatest importance were selected.
Searching
The major national and international databases were searched using the following key words: emigrants and immigrants, refugees, Afghan, Iran, prevalence, incidence, tuberculosis, human immunodeficiency virus (HIV), acquired immunodeficiency syndrome, malaria, cholera, Crimean-Congo hemorrhagic fever (CCHF), hepatitis B, hepatitis C, and leishmaniasis. The international databases included the Web of Knowledge (January 1945 to November 2013), ScienceDirect (January 1823 to November 2013), Medline (January 1950 to November 2013), and Scopus (January 1973 to November 2013). Moreover, the following national databases were searched: Science Information Database (up to November 2013), MagIran (up to November 2013), IranMedex (up to November 2013), and Medlib (up to November 2013).
The reference lists of all included studies were searched in order to obtain additional articles. We also contacted the authors of the included studies.
Criteria for including studies
All descriptive studies regarding the most significant infectious diseases in Iran, namely, tuberculosis, cholera, hemorrhagic fever, malaria, HIV/acquired immune deficiency syndrome (AIDS), hepatitis B, hepatitis C, and leishmaniasis, were retrieved irrespective of the nationality of the subjects and language of the study. The main point of interest was the proportion of Afghan immigrants with the listed diseases in Iran.
Data collection and validity assessment
Two authors (Pourhossein, Doosti Irani) independently screened the title and abstract of all obtained studies and then reviewed the full texts of the retrieved studies that met the inclusion criteria of this review.
The authors were not blinded to the names of the studies’ authors and journals. All disagreements between the authors about the final selection of studies were resolved by negotiation with a third author (Mostafavi). The agreement rate of the two authors was 88.44%, and the kappa statistic for checking reliability was 76.47%.
The variables that were extracted for data analysis included: study design, year and location of the study, type of infectious disease, nationality of participants, sample size, number of Afghan patients, and number of Iranian patients.
Six items from the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement checklist [16] were selected and used for assessing the quality of reporting. They included the following: (a) describe the setting, location and related times; (b) describe the demographic characteristics of the people that participated in the study; (c) give the inclusion and exclusion criteria; (d) describe the methods for the measurement of the outcome; (e) present the key element of the study design; and (f) state how the study sample size was derived.
The studies that fulfilled all items were classified as high quality, studies that did not meet one item were classified as intermediate quality, and studies that did not fulfill more than one item were classified as low quality.
The studies with a small number of patients were excluded from this review. For this purpose, a minimum sample of 18 was considered the cut-off point for estimating the proportion of Afghan patients in Iran (assuming p to be 85% with a statistical power of 80% and significance level of 5%). Thus, the studies with a sample size <18 were not eligible for this study and excluded from analysis.
Statistical methods
The measure of interest was the proportion of Afghan immigrants afflicted with infectious diseases including TB, multiple-drug-resistant tuberculosis (MDR TB), cholera, CCHF, malaria, hepatitis B, and leishmaniasis with a 95% confidence interval (CI). Statistical heterogeneity was explored using Cochran’s Q test and Higgins’ I2 statistic. The analysis was performed using the STATA version 11 (StataCorp, College Station, TX, USA). The random effects model was used with a 95% CI.
RESULTS
Description of studies
We extracted 223 studies up to November 2013, including 101 through searching the international databases, 103 through searching national databases, 8 through checking the reference lists of the included studies, and 11 through contact with the authors of the selected studies (Figure 1).
Figure 1.
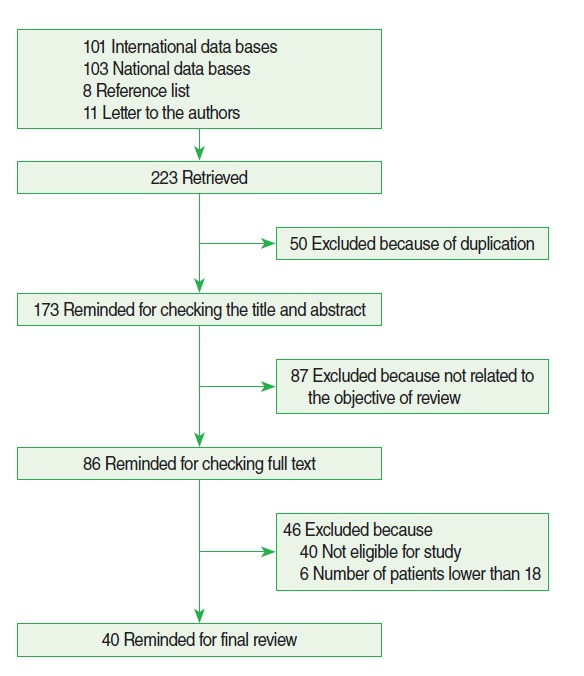
Flow diagram showing the phases of retrieving articles, checking eligibility criteria, and including the articles into the meta-analysis.
Of the 223 extracted studies, 50 studies were excluded because of duplication, 87 studies were excluded because they did not support the objective of this review, 40 studies did not meet the eligibility criteria for this review, and 6 studies had too small of a sample size. In the end we included 40 studies [17-56] in this review (Table 1). The combined included studies involved 125,248 participants.
Table 1.
Characteristics of the included studies in meta-analysis
| Author (published year) [Ref] | Location | Type of the disease | Sex | Sample size | Afghan patients (%) | Iranian patients (%) |
|---|---|---|---|---|---|---|
| Abbasi et al. (2004) [17] | Gorgan | Leishmaniasis | M, F | 175 | 2.29 | 97.71 |
| Alavi-Naini et al. (2006) [18] | Zabol & Zahedan | CCHF | M, F | 255 | 25.5 | 74.5 |
| Aminzadeh & Akhyani (2005) [19] | Tehran | Tuberculosis | M, F | 81 | 17.28 | 82.72 |
| Amirmozafari et al. (2006) [20] | Tehran | Tuberculosis | M, F | 439 | 21.18 | 78.82 |
| Ayatollahi et al. (2010) [21] | Yazd | Tuberculosis | M, F | 32 | 21.88 | 78.12 |
| Ayatollahi et al. (2010) [21] | Shiraz | Tuberculosis | M, F | 104 | 45.2 | 54.8 |
| Barati et al. (2010) [22] | Karaj | Cholera | M, F | 54 | 7.4 | 92.6 |
| Doroudchi et al. (2000) [23] | Shiraz | Tuberculosis | M, F | 101 | 20.79 | 79.2 |
| Ebrahimzadeh et al. (2009) [24] | Birjand | Tuberculosis | M, F | 840 | 3.93 | 96.07 |
| Farnia et al. (2006) [25] | Tehran | MDR TB | M, F | 263 | 66.54 | 33.46 |
| Farnia et al. (2006) [25] | Tehran | Tuberculosis | M, F | 1479 | 33.34 | 66.66 |
| Faenia et al. (2008) [26] | Tehran | Tuberculosis | M, F | 199 | 22.61 | 77.39 |
| Fathimoghaddam et al. (2011) [27] | Mashhad | Hepatitis B | M, F | 22 | 13.64 | 86.36 |
| Forotani (2007) [28] | Larestan | Malaria | M, F | 80 | 33.75 | 66.25 |
| Izadi et al. (2004) [29] | Zahedan & Zabol | CCHF | M, F | 24 | 20.8 | 79.2 |
| Jonaidi et al. (2007) [30] | National | Cholera | M, F | 1115 | 2.24 | 97.76 |
| Kadivar et al. (2007) [31] | Shiraz | Tuberculosis | M, F | 1026 | 36.16 | 63.84 |
| Khalifesoltani et al. (1997) [32] | Kashan | Tuberculosis | M, F | 183 | 32.79 | 67.21 |
| Khatami et al. (2008) [33] | Tehran | Tuberculosis | M, F | 30 | 36.67 | 63.33 |
| Khazaei et al. (2005) [35] | Zabol | Cholera | M, F | 362 | 18.78 | 81.22 |
| Khazaei et al. (2005) [34] | Zabol | Tuberculosis | M, F | 2731 | 23.51 | 76.49 |
| Mansoori et al. (2003) [36] | National | Tuberculosis | M | 373 | 31.5 | 68.49 |
| Mohammadi Anzi et al. (2008) [37] | Damghan | Tuberculosis | M, F | 89 | 222.47 | 77.53 |
| Mohammadi Anzi et al. (2010) [38] | Damghan | Leishmaniasis | M, F | 465 | 4.3 | 95.7 |
| Momeni & Aminjavaheri (1994) [39] | Isfahan | Leishmaniasis | M, F | 1250 | 13.2 | 86.8 |
| Moshfe et al. (2003) [40] | Kohgiluyeh & Boyer-Ahmad | Malaria | M, F | 485 | 37.32 | 62.68 |
| Mousavi et al. (2009) [41] | Kashan | Tuberculosis | M, F | 196 | 54.59 | 45.81 |
| Najafi et al. (2006) [42] | Mazandaran | Malaria | M, F | 518 | 80.31 | 19.69 |
| Raeisi et al. (2009) [43] | National 2002 | Malaria | M, F | 15378 | 42.13 | 57.87 |
| Raeisi et al. (2009) [43] | National 2003 | Malaria | M, F | 25027 | 21.9 | 78.1 |
| Raeisi et al. (2009) [43] | National 2004 | Malaria | M, F | 13166 | 30.49 | 69.51 |
| Raeisi et al. (2009) [43] | National 2005 | Malaria | M, F | 19285 | 13.5 | 86.5 |
| Raeisi et al. (2009) [43] | National 2006 | Malaria | M, F | 15896 | 10.39 | 89.61 |
| Raeisi et al. (2009) [43] | National 2007 | Malaria | M, F | 16647 | 7.45 | 92.55 |
| Ramazanzadeh et al. (2006) [44] | National | Tuberculosis | M, F | 345 | 25.22 | 74.78 |
| Ranjbar et al. (2010) [45] | Karaj | Cholera | M, F | 110 | 4.55 | 95.45 |
| Salarri & Kalantari (2004) [46] | Yazd | Tuberculosis | M, F | 600 | 36.34 | 63.66 |
| Salehi & Pourahmad (2001) [47] | Isfahan | Tuberculosis | M, F | 164 | 45.12 | 54.88 |
| Setoudeh Maram & Fararoei (1999) [48] | Fars | Tuberculosis | M, F | 977 | 13.2 | 86.79 |
| Shamaei et al. (2009) [49] | National | Tuberculosis | M, F | 548 | 33.94 | 66.06 |
| Sharifi-Mood (2006) [57] | Zahedan | Tuberculosis | M, F | 195 | 16.92 | 83.08 |
| Soleimanifard et al. (2011) [51] | Isfahan | Malaria | M, F | 675 | 97.92 | 3.55 |
| Tajadin et al. (2008) [52] | Tehran | Tuberculosis | M, F | 191 | 38.22 | 61.78 |
| Velayati et al. (2009) [53] | National | MDR TB | M, F | 146 | 44.52 | 55.47 |
| Yazdanpanah et al. (2003) [54] | Tehran | Tuberculosis | F | 481 | 27.65 | 72.35 |
| Yazdanpanah et al. (2003) [54] | Tehran | Tuberculosis | M | 547 | 35.28 | 64.72 |
| Youssefi & Taghi (2011) [55] | Sistan & Baluchestan | Malaria | M, F | 1461 | 3.35 | 82.68 |
| Zia-Sheikholeslami & Rezaeian (2010) [56] | Rafsanjan | Malaria | M, F | 742 | 98.92 | 1.08 |
Ref, reference; CCHF, Crimean-Congo hemorrhagic fever; MDR TB, multiple-drug-resistant tuberculosis; M, male; F, female.
We assessed the quality of included studies based on a STROBE checklist. Twenty-nine percent of included studies were high statement quality, 42% were intermediate quality, and 29% were low quality.
In this study, we performed a stratified analysis according to the quality of the studies, date of performance of the study, and type of infectious disease.
Proportion of Afghan immigrants with tuberculosis and MDR tuberculosis in Iran
Twenty-two studies [19-21,23-26,31-34,36,37,41,44,46-50, 52,54] addressed the number of Afghan immigrants in Iran with TB from 1997 to 2010. The pooled proportion estimation of Afghan immigrants with TB on the basis of random effect was 29% (95% CI, 0.23 to 0.34). The lowest proportion, 4%, was reported by Ebrahimzadeh et al. [24] in 2009 and the highest proportion, 55%, was reported in the Kashan study [41] in 2009. Two studies addressed the number of Afghan immigrants with MDR TB [29,53]. The pooled proportion estimation of Afghan immigrants in Iran with MDR TB on the basis of random effect was 56% (95% CI, 0.34 to 0.77) (Table 2).
Table 2.
Subgroup analysis of proportion of Afghan immigrant population with infectious diseases by quality of the included studies, year of studies conduction and type of infectious diseases
| Afghan immigrants |
p-value1 | ||
|---|---|---|---|
| Proportion | 95% CI | ||
| Quality of included studies | |||
| Low risk | 0.206 | 0.146, 0.267 | 0.001 |
| Intermediate | 0.305 | 0.218, 0.392 | 0.001 |
| High risk | 0.354 | 0.108, 0.601 | 0.001 |
| Year of study conduction | |||
| 1994-2000 | 0.118 | 0.132, 0.244 | 0.001 |
| 2000-2007 | 0.307 | 0.221, 0.393 | 0.001 |
| 2007-2011 | 0.277 | 0.053, 0.607 | 0.001 |
| Type of diseases | |||
| Tuberculosis | 0.288 | 0.233, 0.344 | 0.001 |
| MDR TB | 0.557 | 0.341, 0.773 | 0.001 |
| Malaria | 0.398 | 0.230, 0.566 | 0.001 |
| Cholera | 0.082 | 0.004, 0.159 | 0.001 |
| Crimean Congo Hemorrhagic fever | 0.25 | 0.200, 0.301 | 0.59 |
| Leishmaniasis | 0.066 | 0.000, 0.132 | 0.001 |
CI, confidence interval; MDR TB, multiple-drug-resistant tuberculosis.
p-value for chi square test for heterogeneity.
Proportion of Afghan immigrants with malaria in Iran
Six studies [28,42,43,51,55,56] addressed the number of Afghan immigrants in Iran with malaria from 2003 to 2011. The pooled proportion estimation of Afghan immigrants in Iran with malaria on the basis of random effect was 40% (95% CI, 0.23 to 0.57). The lowest proportion, 4%, was in the Sistan and Baluchistan study [55] in 2011, and the highest proportion, 99%, was in the Rafsanjan study [56] in 2010 (Table 2).
Proportion of Afghan immigrants with Crimean-Congo hemorrhagic fever in Iran
Two studies addressed the number of Afghan immigrants in Iran with CCHF [18,29]. The pooled proportion estimation of Afghan immigrants among patients with CCHF was 25% (95% CI, 0.20 to 0.30) (Table 2).
Proportion of Afghan immigrants with cholera in Iran
Four studies addressed the number of Afghan immigrants among people in Iran with cholera [22,30,35,45]. The pooled proportion estimation of Afghan immigrants with cholera in Iran on the basis of random effect was 8% (95% CI, 0.004 to 0.16). The lowest proportion, 2%, was in a national study [30] in 2007, and the highest proportion, 19%, was in the Zabol study [35] in 2005 (Table 2).
Proportion of Afghan immigrants with leishmaniasis in Iran
We found three studies concerning leishmaniasis that addressed the number of Afghan immigrants with leishmaniasis [17, 38,39]. The pooled proportion estimation of Afghan immigrant with leishmaniasis was 7% (95% CI, 0.00 to 0.13). The lowest estimate, 2%, was related by the Gorgan study [17] in 2004, and highest estimate was related by the Isfahan study [39] in 1994 (Table 2).
Proportion of Afghan immigrants with hepatitis B in Iran
One study concerning hepatitis B had eligibility criteria for inclusion in this review [27]. The proportion of Afghan immigrants in Iran with hepatitis B reported in that study was 14%.
DISCUSSION
TB, MDR TB, malaria, cholera, CCHF, leishmaniasis, and hepatitis B are the major infectious diseases among Afghan immigrants in Iran. Iran spends much annually for the prevention, control, and treatment of these infectious diseases. It has been estimated that the government spends more than 100,000 US dollars annually just to treat Afghan immigrants with TB [57, 58]. The results of this meta-analysis indicated that a high proportion of cases of serious infectious disease in Iran are Afghan immigrants; in fact, Afghan nationals comprised 29% of patients with infectious diseases in Iran. Furthermore our findings indicated that the infectious diseases with the highest proportion of Afghan immigrants were MDR TB (56%), malaria (40%), TB (29%), and CCHF (25%), in that order.
It should also be noted that the proportion of Afghan immigrants with infectious diseases in Iran has been increasing since 1994. This means that the high proportion of Afghan immigrants with infectious diseases is a critical public health issue in Iran. Health behavior and health care access factors may be related to the high proportion of Afghan immigrants in major infectious diseases in Iran. It has been noted that Afghan immigrants have little interaction with health care centers in Iran [59] and therefore do not receive adequate health care and treatment. This, in turn, facilitates the spread of infectious diseases in the community.
Afghanistan is known as a country with a high prevalence of TB. The latest reports indicate the annual incidence of TB in Afghanistan is 325 cases out of 100,000 members of the general population [60]. Over recent years, TB has been well controlled in Iran, but due to extensive migration of Afghans infected with TB, Iran is once again facing a spread of the disease [34]. The prevalence of MDR TB among the TB patients in Iran is reported to be 5.1% [25]. This meta-analysis found that 29% of TB patients and 55% of MDR TB patients in Iran are Afghan immigrants. Poor health conditions and services over the past three decades in Afghanistan have caused an increase in MDR TB among Afghans. Some of the immigrants to Iran lack a stable residence. This factor may cause a situation in which Iranian health service personnel cannot follow up during the treatment period [58,61].
One study conducted in Golestan province in north-east Iran also revealed that the incidence rate of all types of TB in Afghan families was significantly higher than in Persian families (42 and 17 cases in each 100 members of the population, respectively) [62]. A study in the city of Tehran carried out on 1,028 patients with TB showed that Afghan patients with pulmonary TB were younger than Iranian patients, and Afghan patients with a positive smear had a more severe type of the disease according to the degree of their sputum smear [58]. The proportion of Afghan immigrants in malaria cases in recent years in Iran was 40%. The reason for this high proportion may be due to the high incidence of malaria in Afghanistan—around 300 to 400 thousand cases yearly [63]. Frequent travel among foreign nationals and immigrants from eastern neighboring countries has become a major barrier to successfully controlling malaria in Iran [28]. A study in southeast Iran indicated that Afghan immigrants have significantly less knowledge of malaria transmission, and they have not implemented prevention practices to the extent of the general Iranian population. In addition, 37.9% of Iranians reported using bed nets, whereas only 10.3% of the Afghans did [59]. Previous experience has revealed that controlling the eastern borders and limiting extensive travel of Afghan nationals have been extremely effective in controlling the distribution of infectious diseases. Likewise, reported cases of malaria in Rafsanjan, in eastern Iran, were 62,000 in 2001, but this figure dropped to 29,000 in 2006 after the return of Afghans to their country [56].
CCHF is known to be a major endemic disease in Afghanistan. The results of this meta-analysis show that 25% of CCHF cases in Iran were in Afghan immigrants. The most important factor for this high proportion is that most cases of CCHF in Iran have been reported from Sistan and Baluchistan province, neighboring Afghanistan and Pakistan; most of the nationwide studies have noted trafficking of infected livestock from Afghanistan and Pakistan to be one of the main reasons for epidemics of this disease [64,65].
Our findings indicated 8% of cholera patients in Iran were Afghan immigrants. Afghanistan is one of the six countries accounting for 80% of all reported cases of cholera worldwide [66]. Therefore, it appears that Afghan immigrants may play a role in the initiation of cholera outbreaks in Iran [30].
The proportion of Afghan immigrants in Iran with leishmaniasis in this review was 7%. Infected humans can act as a reservoir for this disease. According to a report published by the WHO in 2002, leishmaniasis cases were estimated to be 200,000 in Kabul [67]. Most of the outbreaks reported were anthroponotic cutaneous leishmaniasis and zoonotic cutaneous leishmaniasis originating from various regions of Afghanistan between 1987 and 2006 [68], so Afghan immigrants with leishmaniasis could be major reservoirs of leishmaniasis in Iran.
Due to laboratory facility limitations, the real scope of the threat of hepatitis B in Afghanistan is not at all clear; therefore, the prevalence of hepatitis B may be underestimated in Afghanistan. However, it can be assumed that around 10% of Afghans are infected with hepatitis B [69]. Only one study [27] that met the criteria for inclusion in this review addressed the proportion of hepatitis B patients who were Afghan. According to that study, 14% of patients with hepatitis B were Afghan immigrants. The prevalence of hepatitis B virus infection among Afghan immigrants was significantly higher than that among Iranians (p= 0.046). The prevalence of hepatitis B in Afghan immigrants in Iran may be high due in particular to the greater prevalence of injection drug use among Afghan immigrants [70]. This may be an important reservoir of hepatitis B in Iran. In general, injection drug use is one of the main pathways by which hepatitis B spreads [69].
There have been several educational workshops for social health workers, licensed health staff, and midwives to increase the health knowledge of more than three thousand Afghans living in Iran. It would seem advisable that such programs and similar educational plans be continued so as to increase the general knowledge of Afghan immigrants.
Although the studies reviewed in this article mainly discussed reported cases of different diseases among immigrant Afghans, it was rare to find studies that mentioned the incidence and prevalence of these diseases in this population and compared them with the Iranian population.
In this study, we only estimated the proportion of Afghan immigrants with certain infectious diseases (TB, MDR TB, malaria, CCHF, cholera, leishmaniasis and hepatitis B) in Iran. We could not estimate the proportion of Afghan immigrants in Iran with other infectious diseases such as HIV/AIDS and hepatitis C virus. Nor could we compare the prevalence of these diseases among the general Iranian population and the resident Afghan population in Iran. We did not have access to complete demographic information for the Afghan immigrants, such as age, education, or employment, so we could not interpret our results based on the demographic information of the Afghan immigrants.
CONCLUSION
The overall pooled estimated proportion of Afghan immigrants in Iran with TB, MDR TB, malaria, CCHF, cholera, leishmaniasis, and hepatitis B was 29%. However, it seems that this estimate was lower than the true proportion. Considering the long common border between Iran and Afghanistan and the high prevalence of travel between these two countries, it is crucial to develop and equip surveillance centers on the borders for early diagnosis of suspicious cases of infections and also for the prevention of the distribution of disease from these locations to other points in Iran. During epidemics of infectious diseases in Afghanistan, careful attention should be paid to the entry points and regulations should be strengthened for examining those people intending to enter Iran from Afghanistan.
In general, more studies on knowledge, attitude and practice among Afghan nationals and a comparison between them and the Iranian population with regard to infectious disease is absolutely necessary to gain enough evidence for better interventions.
Acknowledgments
The authors of this study would like to express their gratitude to Dr. A. Akbar Haghdoost and Dr. Ali Mirzazadeh from Kerman University of Medical Sciences for reading the first draft of this article and sharing their invaluable comments.
This work was financially supported by the Pasteur Institute of Iran (Grant No. 582).
Footnotes
The authors have no conflicts of interest to declare for this study.
REFERENCES
- 1.United Nations Number of international migrants rises above 232 million. 2013 [cited 2014 Nov 14]. Available from: http://www.un.org/en/development/desa/news/population/number-of-international-migrants-rises.html.
- 2.Crisp J, Jacobsen K. Refugee camps reconsidered. Forced Migr Rev. 1998;3:27–30. [Google Scholar]
- 3.Zimmerman C, Kiss L, Hossain M. Migration and health: a framework for 21st century policy-making. PLoS Med. 2011;8:e2015002. doi: 10.1371/journal.pmed.1001034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Naeeni M. Consequences of unauthorized entry and residence of foreign nationals in Iran. Nameh-Ye-Mofid. 2005;11:47–64. (Persian) [Google Scholar]
- 5.Abbasi-Shavazi MJ, Glazebrook D. Continued protection, sustainable reintegration: Afghan refugees and migrants in Iran. 2006 [cited 2014 Jan 26]. Available from: http://www.refworld.org/pdfid/47c3f3c51a.pdf.
- 6.Van Engeland-Nourai A. Repatriation of Afghan and Iraqi refugees from Iran: when home is no longer home. Int J Multicult Soc. 2008;10:145–168. [Google Scholar]
- 7.Afghanistan Research and Evaluation Unit (AREU) Second-generation Afghans in Iran: integration, identity and return. [cited 2014 Dec 20]. Available from: http://www.refworld.org/docid/4846b2062.html.
- 8.Omidvar N, Ghazi-Tabatabie M, Sadeghi R, Mohammadi F, Abbasi-Shavazi MJ. Food insecurity and its sociodemographic correlates among Afghan immigrants in Iran. J Health Popul Nutr. 2013;31:356–366. doi: 10.3329/jhpn.v31i3.16828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sengupta B. Earnings and sectoral choice of low-skill Afghan workers in iran: evidence from micro-level survey data. Public Policy Admin Res. 2011;1:35–42. [Google Scholar]
- 10.Karimi-Moughari Z. Influence of Afghan refugees on wages and employment in Iran. Iran Econ Res J. 2004;18:57–88. [Google Scholar]
- 11.Rezaeian M, Salem Z, Shahi Gh, Shamsaee A, Zareh R. Nutritional status of Afghan refugee children residing in the city of Shahriar, using body mass index. PAYESH. 2008;7:8–23. (Persian) [Google Scholar]
- 12.Koepke B. The situation of Afghans in the Islamic Republic of Iran nine years after the overthrow of the Taliban regime in Afghanistan. 2011 [cited 2014 Dec 26]. Available from: http://www.refugeecooperation.org/publications/afghanistan/pdf/03_koepke.pdf.
- 13.World Health Organization Tuberculosis country profiles. [cited 2014 Dec 26]. Available from: http://www.who.int/tb/country/data/profiles/en/
- 14.World Health Organization Cutaneous leishmaniasis country profiles. [cited 2014 Dec 26]. Available from: http://www.emro.who.int/neglected-tropical-diseases/information-resources-leishmaniasis/
- 15.World Health Organization World malaria report 2014. [cited 2014 Dec 26]. Available from: http://www.who.int/malaria/publications/world_malaria_report_2014/en/
- 16.Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Ann Intern Med. 2007;147:e2015002. doi: 10.7326/0003-4819-147-8-200710160-00010-w1. W194. [DOI] [PubMed] [Google Scholar]
- 17.Abbasi A, Ganbary MR, Kazem Nezhad K. The epidemiology of cutaneous leishmaniasis in Gorgan, 1998-2001. J Army Univ Med Sci IR Iran. 2004;1:275–278. (Persian) [Google Scholar]
- 18.Alavi-Naini R, Moghtaderi A, Koohpayeh HR, Sharifi-Mood B, Naderi M, Metanat M, et al. Crimean-Congo hemorrhagic fever in Southeast of Iran. J Infect. 2006;52:378–382. doi: 10.1016/j.jinf.2005.07.015. [DOI] [PubMed] [Google Scholar]
- 19.Aminzadeh Z, Akhyani H. Clinical manifestations of extra pulmonary tuberculosis in Loghman-Hakim hospital. Tabibe Shargh. 2005;4:283–288. (Persian) [Google Scholar]
- 20.Amirmozafari N, Ramezanzadeh R, Farnia P, Ghazi F. The frequency of Beijing genotype of Mycobacterium tuberculosis isolated from tuberculosis patients. Razi J Med Sci. 2006;13:7–17. (Persian) [Google Scholar]
- 21.Ayatollahi J, Sharifi MR, Razmi H, Mahmoodiardekani B. The survey of tuberculosis patients in Yazd and Shiraz. Q Res J Yazd. 2010;9:1–7. (Persian) [Google Scholar]
- 22.Barati HA, Golmohmmadi A, Momeni I, Mpradi G. A cholera outbreak investigation in Karaj district in 2008. Iran J Epidemiol. 2010;6:28–34. (Persian) [Google Scholar]
- 23.Doroudchi M, Kremer K, Basiri EA, Kadivar MR, Van Soolingen D, Ghaderi AA. IS6110-RFLP and spoligotyping of Mycobacterium tuberculosis isolates in Iran. Scand J Infect Dis. 2000;32:663–668. doi: 10.1080/003655400459595. [DOI] [PubMed] [Google Scholar]
- 24.Ebrahimzadeh A, Sharifzadeh GR, Eshaghi S. The epidemiology of Tuberculosis in Birjand (1996-2006) J Birjand Univ Med Sci. 2009;16:31–38. (Persian) [Google Scholar]
- 25.Farnia P, Masjedi MR, Mirsaeidi M, Mohammadi F, Vincent V, Bahadori M, et al. Prevalence of Haarlem I and Beijing types of Mycobacterium tuberculosis strains in Iranian and Afghan MDR-TB patients. J Infect. 2006;53:331–336. doi: 10.1016/j.jinf.2005.12.020. [DOI] [PubMed] [Google Scholar]
- 26.Farnia P, Masjedi MR, Varahram M, Mirsaeidi M, Ahmadi M, Khazampour M, et al. The recent-transmission of Mycobacterium tuberculosis strains among Iranian and Afghan relapse cases: a DNA-fingerprinting using RFLP and spoligotyping. BMC Infect Dis. 2008;8:109. doi: 10.1186/1471-2334-8-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fathimoghaddam F, Hedayati-Moghaddam MR, Bidkhori HR, Ahmadi S, Sima HR. The prevalence of hepatitis B antigen-positivity in the general population of Mashhad, Iran. Hepat Mon. 2011;11:346–350. [PMC free article] [PubMed] [Google Scholar]
- 28.Forootani MR. Malaria infestation in foreign immigrants residing Larestan township in 2003-2004. Bimonth J Hormozgan Univ Med Sci. 2007;11:229–236. (Persian) [Google Scholar]
- 29.Izadi S, Naieni KH, Madjdzadeh SR, Nadim A. Crimean-Congo hemorrhagic fever in Sistan and Baluchestan Province of Iran, a case-control study on epidemiological characteristics. Int J Infect Dis. 2004;8:299–306. doi: 10.1016/j.ijid.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 30.Jafari NJ, Radfar MH, Ghofrani H, Asl HM. (2007). Epidemiological and bacteriological features of the cholera outbreak in Iran (2005) J Med Sci. 2007;7:645–649. [Google Scholar]
- 31.Kadivar MR, Ghaneh-Shirazi R, Khavandegaran F, Karimi M. Epidemiology of tuberculosis among Afghan immigrants in Fars province, southern Islamic Republic of Iran. East Mediterr Health J. 2007;13:758–764. [PubMed] [Google Scholar]
- 32.Khalife Soltani SA, Afzali H, Arbabi M. Epidemiology of tuberculosis in TB Center in Kashan in 1993 to 1996. FEYZ. 1997;4:81–88. (Persian) [Google Scholar]
- 33.Khatami A, Sabouri S, Ghoroubi J, Rassouli N, Gorji FA. Radiological findings of pulmonary tuberculosis in infants and young children. Iran J Radiol. 2008;5:231–234. [Google Scholar]
- 34.Khazaei HA, Rezaei N, Bagheri GR, Dankoub MA, Shahryari K, Tahai A, et al. Epidemiology of tuberculosis in the Southeastern Iran. Eur J Epidemiol. 2005;20:879–883. doi: 10.1007/s10654-005-2152-y. [DOI] [PubMed] [Google Scholar]
- 35.Khazaei HA, Rezaei N, Bagheri GR, Mahmoudi M, Moin AA, Dankoub MA, et al. The epidemiology of vibrio cholerae in Zabol city, southeast of Iran. Arch Iran Med. 2005;8:197–201. [Google Scholar]
- 36.Mansoori SD, Arami S, Mirabolhasani Z, Farnia P, Velayati AA. The pattern of drug resistance among newly diagnosed and old cases of pulmonary tuberculosis in NIRITLD. Arch Iran Med. 2003;6:255–260. [Google Scholar]
- 37.Mohamadi Azni S, Mansourian AA, Nokandeh Z. Epidemiological study of tuberculosis in Damghan city (Iran) during 2003-2007. J Semnan Univ Med Sci. 2008;9:315–320. (Persian) [Google Scholar]
- 38.Mohammadi Azni S, Nokandeh Z, Khorsandi AA, Sanei Dehkordi AR. Epidemiology of cutaneous leishmaniasis in Damghan. Iran J Mil Med. 2010;12:131–135. [Google Scholar]
- 39.Momeni AZ, Aminjavaheri M. Clinical picture of cutaneous leishmaniasis in Isfahan, Iran. Int J Dermatol. 1994;33:260–265. doi: 10.1111/j.1365-4362.1994.tb01039.x. [DOI] [PubMed] [Google Scholar]
- 40.Moshfe A, Abolghasem Hosseini S, Karimi Z. Demographic pattern of malaria in Kohgiloyeh and Boyerahmad province in 1996-2003. J Yasuj Univ Med Sci. 2003;8:27–39. (Persian) [Google Scholar]
- 41.Mousavi GA, Saberi H, Sharif A, Ghorbani F, Shadkam M, Vojdani S, et al. A comparative study of patients with pulmonary tuberculosis and extrapulmonary tuberculosis in Kashan during 2002-7. J Kashan Univ Med Sci. 2009;13:235–241. (Persian) [Google Scholar]
- 42.Najafi N, Ghasemian R, Farahmand M. Epidemiology of malaria in Mazandaran province during 1999-2003. J Mazandaran Univ Med Sci. 2006;50:125–132. (Persian) [Google Scholar]
- 43.Raeisi A, Nikpoor F, Ranjbar Kahkha M, Faraji L. The trend of Malaria in I.R. Iran from 2002 to 2007. Hakim Res J. 2009;12:35–41. (Persian) [Google Scholar]
- 44.Ramazanzadeh R, Farnia P, Amirmozafari N, Ghazi F, Ghadertotonchi Z, Kamran J, et al. Comparison between molecular epidemiology, geographical regions and drug resistance in Mycobacterium tuberculosis strains isolated from Iranian and Afghan patients. Chemotherapy. 2006;52:316–320. doi: 10.1159/000095971. [DOI] [PubMed] [Google Scholar]
- 45.Ranjbar M, Rahmani E, Nooriamiri A, Gholami H, Golmohamadi A, Barati H, et al. High prevalence of multidrug-resistant strains of Vibrio cholerae, in a cholera outbreak in Tehran-Iran, during June-September 2008. Trop Doct. 2010;40:214–216. doi: 10.1258/td.2010.100015. [DOI] [PubMed] [Google Scholar]
- 46.Salarri MH, Kalantari AB. Characteristics of tuberculosis patients in Yazd province, Islamic Republic of Iran, 1997-99. East Mediterr Health J. 2004;10:175–179. [PubMed] [Google Scholar]
- 47.Salehi H, Pourahmad M. Demographic characters of patients with tubercolosis: Isfahan 1998-1999. J Res Med Sci. 2001;6:151–152. [Google Scholar]
- 48.Setoudeh Maram E, Fararoei M. Incidence of tuberculosis in cities of Fars. J Qazvin Univ Med Sci Health Serv. 1999;11:67–74. (Persian) [Google Scholar]
- 49.Shamaei M, Marjani M, Chitsaz E, Kazempour M, Esmaeili M, Farnia P, et al. First-line anti-tuberculosis drug resistance patterns and trends at the national TB referral center in Iran--eight years of surveillance. Int J Infect Dis. 2009;13:e2015002. doi: 10.1016/j.ijid.2008.11.027. e240. [DOI] [PubMed] [Google Scholar]
- 50.Metanat M, Salehi M. Prevalence of extrapulmonary tuberculosis in children, Zahedan, Iran. J Med Sci. 2006;6:52–54. [Google Scholar]
- 51.Soleimanifard S, Akbari M, Sabetghadam M, Saberi S. Malaria situation in Isfahan in the last five years. J Isfahan Med Sch. 2011;29:273–280. (Persian) [Google Scholar]
- 52.Tajadin E, Farnia P, Kargar M, Nawrozi J, Ramazanzadeh R, Kazempour M, et al. Assessment of genetic pattern of mycobactrium TB isolated from Iranian and Afghan TB patients by means of VNTR typing. Sci J Kurdistan Univ Med Sci. 2008;13:53–61. (Persian) [Google Scholar]
- 53.Velayati AA, Masjedi MR, Farnia P, Tabarsi P, Ghanavi J, Ziazarifi AH, et al. Emergence of new forms of totally drug-resistant tuberculosis bacilli: super extensively drug-resistant tuberculosis or totally drug-resistant strains in Iran. Chest. 2009;136:420–425. doi: 10.1378/chest.08-2427. [DOI] [PubMed] [Google Scholar]
- 54.Yazdanpanah M, Masjedi H, Hosseini M, Velayati AA, Masjedi MR. Tuberculosis status among iranian and Afghan patients referred to the national research institute of tuberculosis and lung disease during 1998-2000. HAKIM. 2003;5:241–246. (Persian) [Google Scholar]
- 55.Youssefi MR, Taghi RM. Prevalence of malaria infection in Sarbaz, Sistan and Bluchistan province. Asian Pac J Trop Biomed. 2011;1:491–492. doi: 10.1016/S2221-1691(11)60107-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zia-Sheikholeslami N, Rezaeian M. The retrospective epidemiological study of malaria in Rafsanjan, Kerman province, from 1999 to 2005. J Hyg Health. 2010;1:24–30. (Persian) [Google Scholar]
- 57.Sharifi-Mood B, Alavi-Naini R, Metanat M. Tuberculosis and drug resistance in Iran. Zahedan J Res Med Sci. 2010;12:2–6. (Persian) [Google Scholar]
- 58.Panahi M, Masjedi H, Hoseini M, Velayeti A, Masjedi M. Iranian and Afghan TB patients referred to the teaching, research and treatment of tuberculosis and lung disease 1999-2001. HAKIM. 2001;5:241–246. (Persian) [Google Scholar]
- 59.Baseri H, Holakouee K, Raeesi A, Shahandeh S, Akbarzadeh K, Ranjbar M, et al. Comparison of knowledge, attitude and performances of Afghanians to Iranians to prevention of malaria transmission in the Iranshahr, 2006-2007. Iran J Epidemiol. 2008;3:7–13. (Persian) [Google Scholar]
- 60.Khan IM, Laaser U. Burden of tuberculosis in Afghanistan: update on a war-stricken country. Croat Med J. 2002;43:245–247. [PubMed] [Google Scholar]
- 61.Rieder HL, Zellweger JP, Raviglione MC, Keizer ST, Migliori GB. Tuberculosis control in Europe and international migration. Eur Respir J. 1994;7:1545–1553. doi: 10.1183/09031936.94.07081545. [DOI] [PubMed] [Google Scholar]
- 62.Salek S, Masjedi MR, Salek S, Emami H. Incidence rate of pulmonary tuberculosis among different ethnicities in Golestan province from 1999 to 2003. Iran J Epidemiol. 2008;3:15–20. (Persian) [Google Scholar]
- 63.Kolaczinski J, Graham K, Fahim A, Brooker S, Rowland M. Malaria control in Afghanistan: progress and challenges. Lancet. 2005;365:1506–1512. doi: 10.1016/S0140-6736(05)66423-9. [DOI] [PubMed] [Google Scholar]
- 64.Bokaie S, Mostafavi E, Haghdoost AA, Keyvanfar H, Gooya MM, Meshkat M, et al. Crimean Congo hemorrhagic fever in northeast of Iran. J Animal Vet Adv. 2008;7:354–361. [Google Scholar]
- 65.Izadi S, Holakouie-Naieni K, Majdzadeh SR, Chinikar S, Nadim A, Rakhshani F, et al. Seroprevalence of Crimean-Congo hemorrhagic fever in Sistan-va-Baluchestan province of Iran. Jpn J Infect Dis. 2006;59:326–358. [PubMed] [Google Scholar]
- 66.Ahmad K. Public health in Afghanistan plunges to new depths. Lancet. 2001;358:301. doi: 10.1016/S0140-6736(01)05521-0. [DOI] [PubMed] [Google Scholar]
- 67.Reithinger R, Mohsen M, Aadil K, Sidiqi M, Erasmus P, Coleman PG. Anthroponotic cutaneous leishmaniasis, Kabul, Afghanistan. Emerg Infect Dis. 2003;9:727–729. doi: 10.3201/eid0906.030026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Faulde M, Schrader J, Heyl G, Amirih M, Hoerauf A. Zoonotic cutaneous leishmaniasis outbreak in Mazar-e Sharif, northern Afghanistan: an epidemiological evaluation. Int J Med Microbiol. 2008;298:543–550. doi: 10.1016/j.ijmm.2007.07.015. [DOI] [PubMed] [Google Scholar]
- 69.Wallace MR, Hale BR, Utz GC, Olson PE, Earhart KC, Thornton SA, et al. Endemic infectious diseases of Afghanistan. Clin Infect Dis. 2002;34:e2015002. doi: 10.1086/340704. S207. [DOI] [PubMed] [Google Scholar]
- 70.Behzadi MA, Ziyaeyan M, Asaei S. Hepatitis B virus DNA level among the seropositive Afghan immigrants, southern Iran. Jundishapur J Microbiol. 2014;7:e2015002. doi: 10.5812/jjm.10127. [DOI] [PMC free article] [PubMed] [Google Scholar]


