Summary
Population-based studies from Europe have suggested that obesity is associated with more advanced stage colorectal cancer on presentation. Obesity is an even more prevalent issue in North America, but comparable data on associations with cancer are lacking. We reviewed the cases of 672 patients with colon cancer diagnosed between 2004 and 2008 in the province of Manitoba who underwent surgical resection at a Winnipeg Regional Health Authority–affiliated hospital. We tested if obesity was associated with more advanced cancer stage or grade. On multivariate analysis, after adjusting for age, sex, tumour location and socioeconomic status, we were unable to show any significant associations between body mass index of 30 or more and advanced stage or grade cancer on presentation. The reasons for the lack of association are likely multifactorial, including the pathophysiology of the disease and process factors, such as screening habits and colonoscopic diagnostic success rates in obese patients.
Colorectal cancer (CRC) is the third most common cancer1 and the second most frequent cause of cancer-related death among men and women in Western countries.2 There appears to be an obesity-related risk associated with many cancers. The strongest associations with obesity observed in men include esophageal, thyroid and colon cancer; in women, the strongest associations include endometrial and gall bladder cancer.3 Several authors have proposed that in patients with colon cancer, obesity may be associated with the formation of advanced adenomatous polyps, its precursor lesion. Siddiqui and colleagues4 found that for every 1-unit increase in body mass index (BMI) above 30, there was a corresponding 1% increase in the frequency of finding advanced adenomatous polyps.
More recent literature suggests that obesity may be associated with not only the development of CRC, but also with more advanced cancers on presentation. A prospective population-based study from Sweden by Brändstedt and colleagues,5 which included 28 098 patients, demonstrated an association between obesity and increased risk of more advanced-stage CRC (T3/T4, N1, or M1 disease), especially in men. This association was seen in all anthropometric factors, including weight, hip circumference, waist circumference, BMI, and waist:height ratio measurements, except body fat percentage. These authors also found sex-related differences in the association between obesity and expression of various CRC-associated mutations, including catenin, cyclin D1, p53 and microsatellite instability screening status, as well as BRAF and KRAS profiles.6,7
Obesity is an important issue in Canada that is growing at an alarming rate, with a prevalence of 25%, as reported by the Public Health Agency of Canada and the Canadian Institute for Health Information in 2011. However, comparable data sets examining obesity and risk of more advanced CRC in Canadian populations are lacking. We therefore performed a large-scale review of patients undergoing surgery for colon cancer in Manitoba, Canada, investigating the association between BMI and colon cancer stage and grade; the primary outcome was the odds of presenting with higher stage (Stage III/IV), and the secondary outcome was the odds of presenting with higher grade (Grade 3) colon cancer. Our study included 687 patients who underwent surgery for colon cancer in Winnipeg Regional Health Authority (WRHA)–affiliated hospitals between 2004 and 2008. Data were abstracted from the Manitoba Cancer Registry and from the patient charts. Two logistic regression models were built, 1 for testing the risk of having a more advanced stage and 1 for having a higher grade of tumour. In our cohort, 358 (53%) patients had stage I–II disease, and 314 (47%) had higher stage (237 Stage III, 77 Stage IV) disease. Lower grade cancer was found in 545 (81%) patients, while high grade cancer was found in 127 (19%) patients
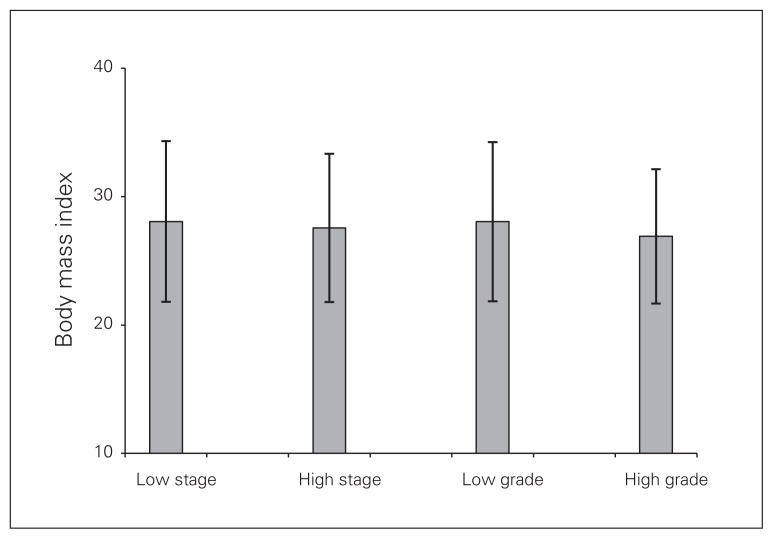
The mean BMI was 27.9 in the overall cohort (28.1 in those with lower stage and 27.6 in those with higher stage cancers, and 28.0 in those with lower grade and 26.9 in those with higher grade cancers; Fig. 1). On multivariate analysis, after adjusting for age, sex, tumour location and socioeconomic status, we did not find any significant associations between obesity (BMI ≥ 30) and odds of presenting with higher stage (odds ratio [OR] 0.91, 95% confidence interval [CI] 0.64–1.30) or higher grade (OR 0.70, 95% CI 0.43–1.12) disease.
Fig. 1.
Mean body mass index of study population based on cancer stage and grade on presentation. Low stage includes Stage I/II. High stage includes Stage III/IV. Low grade includes Grade 1/2. High grade includes Grade 3. Error bars denote standard deviation.
There are several possible reasons for the differences in findings between our study and those of the Swedish study. First, BMI is a labile variable, especially in patients with cancer. It is affected by multiple factors, including individual eating habits, stress, level of physical activity and the biology of the disease itself. It may be difficult to distinguish between risk factors for advanced disease versus the consequences of progressing disease. It is possible that the cancer itself decreases BMI in some patients, owing to factors such as obstruction-related symptoms or cancer-induced cachexia, even before diagnosis. We chose to use patient BMIs recorded just before surgery as a snapshot for each patient in order to achieve some consistency in time points for BMI data collection before the effects of surgery and any adjuvant treatments could play a role. In comparison, the anthropometric factors in the Swedish study were collected prospectively as part of the Mälmo Diet and Cancer Study from a nationwide population-based cohort. The data were thereby collected before the diagnosis of cancer, which may be a better representation of the patients’ true BMI before any cancer effects on body mass. A further limitation to our study, considering the data were reviewed retrospectively, was that we could not verify whether all height and weight measurements were made directly by clinic staff in the preoperative anesthesia data forms as per protocol or whether patient estimates were included. A power calculation estimated the need for 400 of each high and low stage, as well as high and low grade cancers to demonstrate a statistically significant association with obesity, thereby rendering our study underpowered, especially for grade. Finally, we reviewed only patients who underwent surgical resection in order to obtain accurate information on tumour stage and grade from the pathology specimens. Other nonsurgical patients with colon cancer, many of whom likely had stage IV disease, were not included, possibly introducing selection bias.
Even if an association between obesity and more advanced colon cancer could have been demonstrated, as in the Swedish study, the question remains as to whether this association is due to the biology of the disease itself, such as invasiveness and proliferative ability, or other factors related to the processes of care in obese patients. The recent discoveries in associations between sex-specific anthropometric factors and biological activity of CRC cancer with respect to gene expression profiles are certainly intriguing.6,7 Another compelling and perhaps equally contributing theory is that the association is due to process variables, such as patient or practitioner-related screening habits or technical diagnostic success rates that may differ in obese patients. Colon cancer stage and grade at the time of diagnosis are likely a result of multiple factors, including biology of the disease; host characteristics, such as BMI; and diagnostic limitations and variability in patient behaviours relating to screening and frequency of health care visits. Further studies are needed to ascertain whether there is an association between obesity and risk of more advanced cancers. If we can unravel the mechanisms behind such an association, there may be areas to target, including process or biological factors, in improving primary or secondary prevention and in the treatment of the disease.
Footnotes
This work was presented in poster format at the Canadian Surgical Forum in Calgary, Alta., in September 2012, and at the American Society of Colon and Rectal Surgeons meeting in Phoenix, AZ, in April 2013.
Competing interests: None declared.
Contributors: All authors contributed substantially to writing and/or revising and to the conception and design of the manuscript and approved the final version submitted for publication.
References
- 1.American Cancer Society. Cancer statistics 2009. [accessed 2014 Dec. 12]. Available: www.cancer.org.
- 2.Parkin DM, Pisani P, Ferlay J. Global cancer statistics. CA Cancer J Clin. 1999;49:33–64. doi: 10.3322/canjclin.49.1.33. [DOI] [PubMed] [Google Scholar]
- 3.Renehan AG, Tyson M, Egger M, et al. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet. 2008;371:569–78. doi: 10.1016/S0140-6736(08)60269-X. [DOI] [PubMed] [Google Scholar]
- 4.Siddiqui A, Pena Sahdala HN, Nazario HE, et al. Obesity is associated with an increased prevalence of advanced adenomatous colon polyps in a male veteran population. Dig Dis Sci. 2009;54:1560–4. doi: 10.1007/s10620-009-0811-7. [DOI] [PubMed] [Google Scholar]
- 5.Brändstedt J, Wangefjord S, Nodin B, et al. Gender, anthropometric factors and risk of colorectal cancer with particular reference to tumour location and TNM stage: a cohort study. Biol Sex Differ. 2012;3:23. doi: 10.1186/2042-6410-3-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brändstedt J, Wangefjord S, Borgquist S, et al. Influence of anthropometric factors on tumor biological characteristics of colorectal cancer of men and women: a cohort study. J Transl Med. 2013;11:293. doi: 10.1186/1479-5876-11-293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brändstedt J, Wangefjord S, Nodin B, et al. Associations of anthropometric factors with KRAS and BRAF mutation status of primary colorectal cancer in men and women: a cohort study. PLoS One. 2014;6:1. doi: 10.1371/journal.pone.0098964. [DOI] [PMC free article] [PubMed] [Google Scholar]