Abstract
Background and Objective:
Despite the prevalence of hysterectomy for treatment of benign gynecologic conditions, providers nationwide have been slow to adopt minimally-invasive surgical techniques. Our objective is to investigate the impact of a department for minimally invasive gynecologic surgery (MIGS) on the rate of laparoscopic hysterectomy at an academic community hospital without robotic technology.
Methods:
This retrospective observational study included all patients who underwent hysterectomy for benign indications from January 1, 2004, through December 31, 2012. The primary outcome was route of hysterectomy: open, laparoscopic, or vaginal. Secondary outcomes of interest included length of stay and factors associated with an open procedure.
Results:
In 2004, only 24 (8%) of the 292 hysterectomies performed for benign conditions at Newton-Wellesley Hospital (NWH) were laparoscopic. The rate increased to more than 50% (189/365) by 2008, and, in 2012, 72% (316/439) of hysterectomies were performed via a traditional laparoscopic approach. By 2012, more than 93% (411/439) of all hysterectomies were performed in a minimally invasive manner (including total laparoscopic hysterectomy [TLH], laparoscopic supracervical hysterectomy [LSH], total vaginal hysterectomy [TVH], and laparoscopy-assisted vaginal hysterectomy [LAVH]). More than 85% of the hysterectomies at NWH in 2012 were outpatient procedures. By this time, the surgeon's preference or lack of expertise was rarely cited as a factor leading to open hysterectomy.
Conclusions:
A large diverse gynecologic surgery department transformed surgical practice from primarily open hysterectomy to a majority (>72%) performed via the traditional laparoscopic route and a large majority (>93%) performed in a minimally invasive manner in less than 8 years, without the use of robotic technology. This paradigm shift was fueled by patient demand and by MIGS department surgical mentorship for generalist obstetrician/gynecologists.
Keywords: Laparoscopic hysterectomy, Benign hysterectomy, Minimally-invasive, Surgical mentorship
INTRODUCTION
At least 430,000 hysterectomies are performed each year in the United States, and more than 80% are for treatment of benign diseases, such as leiomyoma, abnormal uterine bleeding, pelvic organ prolapse, and endometriosis.1,2 Hysterectomy is the second most common surgery undergone by women and accounts for $5 billion dollars annually in U.S. health care spending.3,4 The first laparoscopic hysterectomy was described in 1989; however, by 2003, only about 11% of the nation's hysterectomies were performed laparoscopically.1,5 By 2010, this number had increased only somewhat, to 20% to 30%.2,4,6 Despite consensus statements by both the American Association of Gynecologic Laparoscopists (AAGL) and the American Congress of Obstetricians and Gynecologists (ACOG) stating that minimally invasive hysterectomy should be the standard of care, more than 50% of hysterectomies for benign indications are still open procedures.7,8 From 2003 through 2010, rates of vaginal hysterectomy have remained fairly constant nationwide at 10% to 15%.9
U.S. Food and Drug Administration approval of robotic technology for hysterectomy in 2005 brought with it the promise of increased ease of minimally invasive hysterectomy: 3-dimensional optics, wristlike motion with robotic instruments, and shorter learning curves than traditional laparoscopy.10 Despite this new technology, the high rates of open hysterectomy persist. For example in one study at an academic teaching hospital with robotic technology, the percentage of hysterectomies performed with robotic assistance increased from 2.5% to 24.8% between 2007 and 2009, but despite marketing campaigns in favor of this minimally invasive technique, the rate of open procedures remained virtually unchanged at approximately 45%.11
The advantages of minimally invasive hysterectomy are well-documented: shorter hospitalization, faster recovery, more rapid return to normal activities, and fewer postoperative infections.1,8 A meta-analysis comparing total laparoscopic hysterectomy (TLH) with total abdominal hysterectomy (TAH) showed a reduction in morbidity—specifically, fewer perioperative complications (pooled odds ratio, 0.31), lower estimated blood loss (≤180 mL), and shorter hospital stay.5
Slow adoption of minimally invasive hysterectomy among practicing obstetrician-gynecologists (OB/GYNs), specifically conventional “straight-stick” laparoscopic hysterectomy, has been attributed to long learning curves and insufficient laparoscopic training in OB/GYN residencies.12 Notably, a survey of OB/GYN physicians showed that surgeons would prefer the laparoscopic or vaginal route for hysterectomy for themselves (40%) or their spouses (55%). Despite this result, the surveyed group cited limited training, technical difficulty, lack of personal surgical experience, and long operating times as substantial barriers to performing minimally invasive hysterectomy.13 Similarly, the general public's awareness of laparoscopic hysterectomy has been slow to develop; however, with the well-documented advantages of this technique, the demand is now increasing rapidly, just as it did for laparoscopic cholecystectomy in the early 1990s.
Hysterectomy via a laparoscopic approach can be performed safely as an outpatient surgery, as shown in a feasibility study by Morrison and Jacobs14 more than 10 years ago. This advantage is a major one for patients, hospitals, and payers. A more recent study comparing outcomes of outpatient (40%) laparoscopic hysterectomies to inpatient (60%) procedures demonstrated significantly fewer 30-day complications in the outpatient group than in the inpatient group (4.5% vs. 7.2%; P < .001).15 Nationwide, from 2006 through 2010, rates of outpatient hysterectomy have increased from 17.5% to greater than 44%. Moreover, same-day discharge protocols have been repeatedly shown to be well-tolerated and safe, with high rates of patient satisfaction.16–19
Given excellent clinical outcomes and high rates of patient satisfaction, we expected public demand to increase at our community hospital. To accommodate this increase, an informal mentorship program was started by the division of minimally invasive gynecologic surgery (MIGS) to expand the surgical skills of community OB/GYN generalists and increase our rates of laparoscopic hysterectomy without the assistance of robotic technology. The primary objective of this retrospective review is to document the trends in techniques for hysterectomy performed during 8 years for benign indications in a community teaching hospital without robotic technology.
MATERIALS AND METHODS
All women more than 18 years of age who underwent hysterectomy for benign indications at Newton-Wellesley Hospital (NWH) from January 1, 2004, through December 31, 2012, were included in this retrospective observational study. The patients were identified by International Classification of Diseases, Ninth Revision (ICD-9) procedure codes in operating room records, and data were collected, including patient age, date of surgery, date of hospital discharge, surgeon, preprocedure ICD-9 diagnostic code, and Current Procedural Terminology (CPT)/ICD-9 codes. Select operative reports were reviewed to verify the accuracy of the operating room database. The primary outcome was route of hysterectomy: open, laparoscopic, or vaginal. Laparoscopic hysterectomy included both total laparoscopic hysterectomy (TLH) and laparoscopic supracervical hysterectomy (LSH). Vaginal hysterectomy included both total vaginal hysterectomy (TVH) and laparoscopy-assisted vaginal hysterectomy (LAVH). Preprocedure diagnoses of malignancy were excluded; however, postprocedure diagnoses of malignancy were included in the analysis. Secondary outcomes, including length of stay and factors associated with the need for an open procedure, were investigated. An outpatient was defined as having a length of stay of 0 days (ie, date of admission and date of discharge were the same). This study was submitted to and accepted by the NWH Institutional Review Board.
RESULTS
NWH is a 313-bed academic community hospital and a member of the Partners Healthcare Network. At NWH, 300 to 440 hysterectomies are performed annually. Our gynecology department includes 42 community-based generalist OB/GYNs and, starting in 2002, a gynecology division devoted to MIGS. The MIGS department expanded from 1 full-time surgeon to 2 full-time surgeons in 2005, with the goals of making NWH a referral center for challenging gynecologic laparoscopy and hysteroscopy cases and of expanding the surgical skills of interested generalist OB/GYN physicians at the hospital.
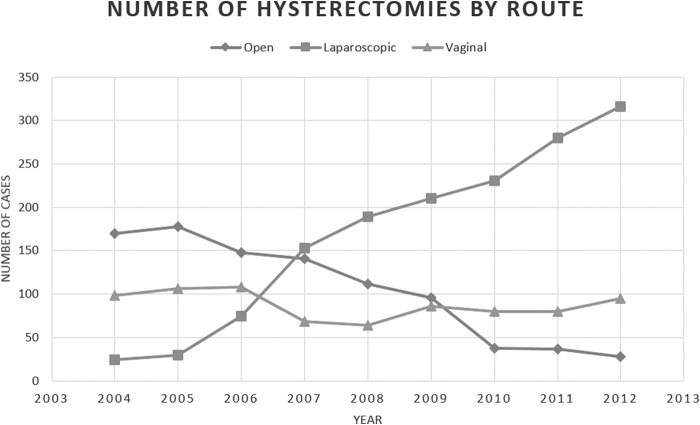
In 2004, at NWH, only 24 (8%) of the 292 hysterectomies performed for benign indications were laparoscopies. This number increased to more than 50% (189/365) by 2008, and, in 2012, 72% (316/439) of benign-indication hysterectomies were performed by laparoscopy. More than 93% (411/439) of all hysterectomies by 2012 were minimally invasive, including TLH, LSH, TVH, and LAVH. The number of LAVHs and TVHs combined did not change significantly from 2004 through 2012, with an average of 98 TVHs+LAVHs performed annually, accounting for 22% to 33% of the volume of hysterectomies. There was, however, a transient downward trend during 2007 and 2008, with only 64 and 68 vaginal procedures performed in those years, respectively (Figure 1). From 2004 through 2012, the annual number of total hysterectomies performed for benign indications at NWH gradually increased from 292 to 439.
Figure 1.
The rate of open hysterectomy declined by year while the rate of laparoscopic hysterectomy increased and vaginal hysterectomy (LAVH+TVH) remained relatively constant at Newton-Wellesley Hospital.
The average age of patients who underwent hysterectomy was 41.3 years. The most frequent ICD-9 preprocedure diagnostic codes were leiomyoma, uterine endometriosis, and excessive menstruation or menstrual disorder not otherwise specified. Factors associated with open hysterectomy in 2011 and 2012 included intraoperative suspicion of malignancy, large fibroid uterus (greater than at 18 weeks' gestation), extensive intra-abdominal adhesions due to endometriosis, or a history of prior surgeries, the most common being cesarean delivery. By 2011, the surgeon's preference or lack of expertise was rarely cited as a factor leading to an open procedure.
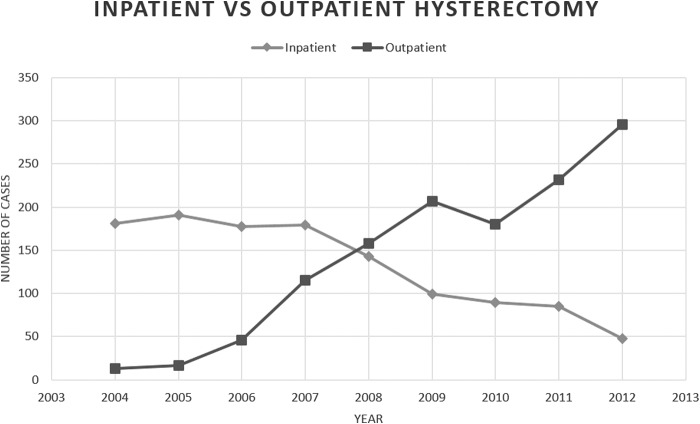
In 2004, only 2 of 194 laparoscopic hysterectomies were performed on an outpatient basis. By 2010, 60% (163/269) were outpatient, and by 2012, the frequency grew to more than 85% (293/344; Figure 2).
Figure 2.
Increasing rate of outpatient laparoscopic hysterectomy compared to declining inpatient laparoscopic hysterectomy by year at Newton-Wellesley Hospital.
DISCUSSION
This retrospective observational study clearly demonstrates the ability of a large diverse gynecologic surgery department to transform its surgical practice from primarily open hysterectomies to a majority (72%) performed via a traditional laparoscopic route and a large majority (93%) via a minimally invasive technique (TLH, LSH, TVH, LAVH) in less than 8 years. This rate of laparoscopic hysterectomy is far higher than rates reported in the current literature. The study results show a drastic increase in the adoption of laparoscopic hysterectomy in our community hospital, even without the use of robotic technology.
The implementation of a robust MIGS department should be given credit for the transformation to a greater than 72% laparoscopic hysterectomy rate at NWH. The MIGS department was started in 2002 and expanded in scope in 2004, with the additional of an AAGL MIGS fellowship program. The MIGS expert laparoscopic surgeons have mentored interested generalist gynecologic surgeons in an effort to improve the latter's laparoscopic surgical skills. This voluntary mentorship program has allowed interested generalist OB/GYNs who were inadequately trained or needed further experience in performing laparoscopic procedures to gain confidence and hone their skills. One or 2 generalists from each private practice group at NWH chose to participate in the informal mentorship program. After these surgeons felt confident in their skills, they began to schedule surgeries with members of their own groups acting as surgical assistants. As a result, by 2012 nearly all of our generalist gynecology groups had practitioners who were able to offer and safely perform minimally invasive hysterectomies. With an MIGS mentorship program and fellowship, minimally invasive hysterectomy is now the surgical standard of care at NWH.7,8
Similar rapid increases in laparoscopic hysterectomy rates have been achieved in other hospital systems without the use of robotic technology. An increase in traditional laparoscopic hysterectomy was demonstrated by the Kaiser Permanente Southern California group. Among more than 300 surgeons, rates of laparoscopic hysterectomy increased from 38% to 78% over a 5-year period with the use of a structured program of didactics and surgical mentorship.20,21 Likewise, the same evolution has occurred at Brigham & Women's Hospital in Boston, where most hysterectomies are performed via a traditional laparoscopic route.22
As patients become more vocal about their desire for laparoscopic hysterectomy, their expectation of having an outpatient surgery should increase in parallel. In 3 large-scale studies, outpatient hysterectomy rates have been as high as 44% to 52%.15,19,23
In our experience, more than 85% of patients have an outpatient procedure. The paradigm shift from inpatient to outpatient laparoscopic hysterectomy is fueled by excellent patient education regarding patients' postoperative expectations of the surgeon and ancillary staff such as clinic personnel and surgical nurses. Patients are medicated before surgery with the goals of preventing postoperative nausea and vomiting and reducing pain. Medications are tailored to the individual and may include a scopolamine patch, oral acetaminophen, and pregabalin. Postoperative pain management includes the use of nonsteroidal anti-inflammatory drugs and limited narcotics. The safety of outpatient hysterectomy is ensured by applying strict postanesthesia care unit discharge criteria. Although not specifically investigated in this study, our anecdotal experience confirms high rates of patient satisfaction, similar to those reported in the literature.
This study documents a paradigm shift in route of hysterectomy over an 8-year span at our hospital. We argue that this increase in rates of laparoscopic hysterectomy can happen on a larger scale, irrespective of the availability of robotic surgical technology, fueled largely by patients' demand for minimally invasive surgery and by mentorship programs to broaden the skills of less experienced laparoscopists. We have demonstrated the ability to teach laparoscopic hysterectomy techniques to interested generalist gynecologists with the goal that these providers will offer minimally invasive hysterectomy to their patients. The creation of an MIGS department with the addition of two MIGS surgeons to the NWH staff made this mentorship program possible. This is our department's greatest strength, as other groups or physician organizations can emulate similar mentorship techniques. As Steege and Einarsson22 asserted in their recent editorial, “physicians and patients would be better served by retraining programs for practicing gynecologists who have sufficient surgical volume to maintain and enhance their skills.” Of note, the reputation of the MIGS department made NWH a community referral center for cases requiring difficult laparoscopy, thus accounting for the increase in the volume of hysterectomies from 2004 through 2012. Despite the presence of the MIGS department, non–fellowship-trained generalist OB/GYNs continue to perform more than 55% of all laparoscopic hysterectomies at NWH.
The weaknesses of this study stem from its observational design. Surgical details such as uterine weight and estimated blood loss were not available. Similarly, we were not privy to patients' characteristics such as body mass index or surgical history because of the way cases were queried with ICD-9 codes, billing data, and operating room records alone. Perspective bias also cannot be completely eliminated from a retrospective, single-center study. Although we attempted to address all confounding factors, it is possible that some confounders were not identified.
CONCLUSIONS
A heterogeneous group of general-practice gynecologists can perform a majority (>72% at NWH) of hysterectomies laparoscopically without the use of robotic technology and a larger majority (>93% at NWH) of hysterectomies with minimally invasive techniques. The transformation from open surgery to conventional laparoscopic hysterectomy at NWH was fueled by informal MIGS department mentorship, as well as the presence of an MIGS fellowship. With this setup, barriers to laparoscopic hysterectomy were conquered and patient demands were satisfied.
Contributor Information
Megan Loring, Center for Minimally Invasive Gynecologic Surgery Newton-Wellesley Hospital, Newton, Massachusetts..
Stephanie N. Morris, Center for Minimally Invasive Gynecologic Surgery Newton-Wellesley Hospital, Newton, Massachusetts..
Keith B. Isaacson, Center for Minimally Invasive Gynecologic Surgery Newton-Wellesley Hospital, Newton, Massachusetts..
References:
- 1. Wu JM, Wechter ME, Geller EJ, Nguyen TV, Visco AG. Hysterectomy rates in the United States, 2003. Obstet Gynecol. 2007;100:1091–1095. [DOI] [PubMed] [Google Scholar]
- 2. Wright JD, Ananth CV, Lewin SN, et al. Robotically assisted vs laparoscopic hysterectomy among women with benign gynecologic disease. JAMA. 2013;309:689–698. [DOI] [PubMed] [Google Scholar]
- 3. Wright KN, Jonsdottir GM, Jorgensen S, Shah N, Einarsson JI. Costs and outcomes of abdominal, vaginal, laparoscopic and robotic hysterectomies. JSLS. 2012;16:519–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rosero EB, Kho KA, Joshi GP, Giesecke M, Schaffer JI. Comparison of robotic and laparoscopic hysterectomy for benign gynecologic disease. Obstet Gynecol. 2013;122:778–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Walsh CA, Walsh SR, Tang TY, Slack M. Total abdominal hysterectomy versus total laparoscopic hysterectomy for benign disease: a meta-analysis. Eur J Obstet Gynecol. 2009;144:3–7. [DOI] [PubMed] [Google Scholar]
- 6. Cohen SL, Vitonis AF, Einarsson JI. Updated hysterectomy surveillance: factors associated with minimally invasive hysterectomy, a cross-sectional analysis. JSLS. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. AAGL Position Statement. Route of hysterectomy to treat benign uterine disease. J Minim Invasive Gynecol. 2011;18:1–3. [DOI] [PubMed] [Google Scholar]
- 8. Choosing the route of hysterectomy for benign disease. ACOG Committee Opinion 444. Obstet Gynecol. 2009;144:1156–1158. [DOI] [PubMed] [Google Scholar]
- 9. Lee J, Jennings K, Borahay MA, et al. Trends in the national distribution of laparoscopic hysterectomies from 2003 to 2010. J Minim Invasive Gynecol. 2014;21:656–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Smorgick N, Patzkowsky KE, Hoffman MR, Advincula AP, Song AH, As-Sanie S. The increasing use of robot-assisted approach for hysterectomy results in decreasing rates of abdominal hysterectomy and traditional laparoscopic hysterectomy. Arch Gynecol Obstet. 2014;289:101–105. [DOI] [PubMed] [Google Scholar]
- 11. Matthews CA, Reid N, Ramakrishnan V, Hull K, Cohen S. Evaluation of the introduction of robotic technology on route of hysterectomy and complications in the first year of use. Am J Obstet Gynecol. 2010;203:491–495. [DOI] [PubMed] [Google Scholar]
- 12. Jacoby VL, Autry A, Jacobson G, Domush R, Nakagawa S, Jacoby A. Nationwide use of laparoscopic hysterectomy compared with abdominal and vaginal approaches. Obstet Gynecol. 2009;114:1041–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Einarsson JI, Matteson KA, Schulkin J, Chavan NR, Sangi-Haghpeykar H. Minimally invasive hysterectomies: a survey on attitudes and barriers among practicing gynecologists. J Minim Invasive Gynecol. 2010;17:167–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Morrison JE, Jacobs VR. Outpatient laparoscopic hysterectomy in a rural ambulatory surgery center. J Am Assoc Gynecol Laparosc. 2004;3:359–364. [DOI] [PubMed] [Google Scholar]
- 15. Khavanin N, Mlodinow A, Milad M, Bilimoria KY, Kim JYS. Comparison of perioperative outcomes in outpatient and inpatient laparoscopic hysterectomy. J Minim Invasive Gynecol. 2013;20:604–610. [DOI] [PubMed] [Google Scholar]
- 16. Kisic-Trope J, Qvigstat E, Ballard K. A randomized trial of day-case vs inpatient laparoscopic supracervical hysterectomy. Am J Obstet Gynecol. 2001;204:301–308. [DOI] [PubMed] [Google Scholar]
- 17. Thiel J, Gamelin A. Outpatient total laparoscopic hysterectomy. J Am Assoc Gynecol Laparosc. 2003;10:481–483. [DOI] [PubMed] [Google Scholar]
- 18. de Lappase C, Rabischong B, Bolandard F, et al. Total laparoscopic hysterectomy and early discharge: satisfaction and feasibility study. J Minim Invasive Gynecol. 2008;15:20–25. [DOI] [PubMed] [Google Scholar]
- 19. Schiavone MB, Herzog TJ, Anath CV, et al. Feasibility and economic impact of same-day discharge for women who undergo laparoscopic hysterectomy. Am J Obstet Gynecol. 2012;207:382–398. [DOI] [PubMed] [Google Scholar]
- 20. Hoffman CP, Kennedy J, Borschel L, Burchette R, Kidd A. Laparoscopic hysterectomy: the Kaiser San Diego experience. J Minim Invasive Gynecol. 2005;12:16–24. [DOI] [PubMed] [Google Scholar]
- 21. Andryjowitz E, Wray T. Regional expansion of minimally invasive surgery for hysterectomy: implementation and methodology in a large multispecialty group. Perm J 2011;15:42–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Steege JF, Einarsson JI. Robotics in benign gynecologic surgery: where should we go? Obstet Gynecol. 2014;123:1–2. [DOI] [PubMed] [Google Scholar]
- 23. Perron-Burdick M, Yamamoto M, Zaritsky E. Same-day discharge after laparoscopic hysterectomy. Obstet Gynecol. 2011;117:1136–1141. [DOI] [PubMed] [Google Scholar]