Abstract
Protein tyrosine phosphatases (PTPs) are enzymes that remove phosphate from tyrosine residues in proteins. Recent whole-exome sequencing of human cancer genomes reveals that many PTPs are frequently mutated in a variety of cancers. Among these mutated PTPs, protein tyrosine phosphatase T (PTPRT) appears to be the most frequently mutated PTP in human cancers. Beside PTPN11 which functions as an oncogene in leukemia, genetic and functional studies indicate that most of mutant PTPs are tumor suppressor genes. Identification of the substrates and corresponding kinases of the mutant PTPs may provide novel therapeutic targets for cancers harboring these mutant PTPs.
Introduction
Protein tyrosine phosphorylation plays a critical role in virtually all human cellular processes that are involved in oncogenesis.1 Protein tyrosine phosphorylation is coordinately regulated by protein tyrosine kinases (PTKs) and protein tyrosine phosphatases (PTPs).1 While PTKs add phosphate to tyrosine residues in proteins, PTPs remove it. Many PTKs are well-documented oncogenes.1 Recent cancer genomic studies provided compelling evidence that many PTPs function as tumor suppressor genes, because a majority of PTP mutations that have been identified in human cancers are loss-of-function mutations. However, a few PTPs also function as oncogenes. A recent article by Michel Tremblay and colleagues comprehensively reviewed the roles of PTPs in human cancers.2 Here, this review focuses on somatic mutations of PTPs uncovered in human cancers by recent large-scale sequencing studies. This discussion considers the functional aspects of several frequently mutated PTPs in cancer.
The human tyrosine phosphatome
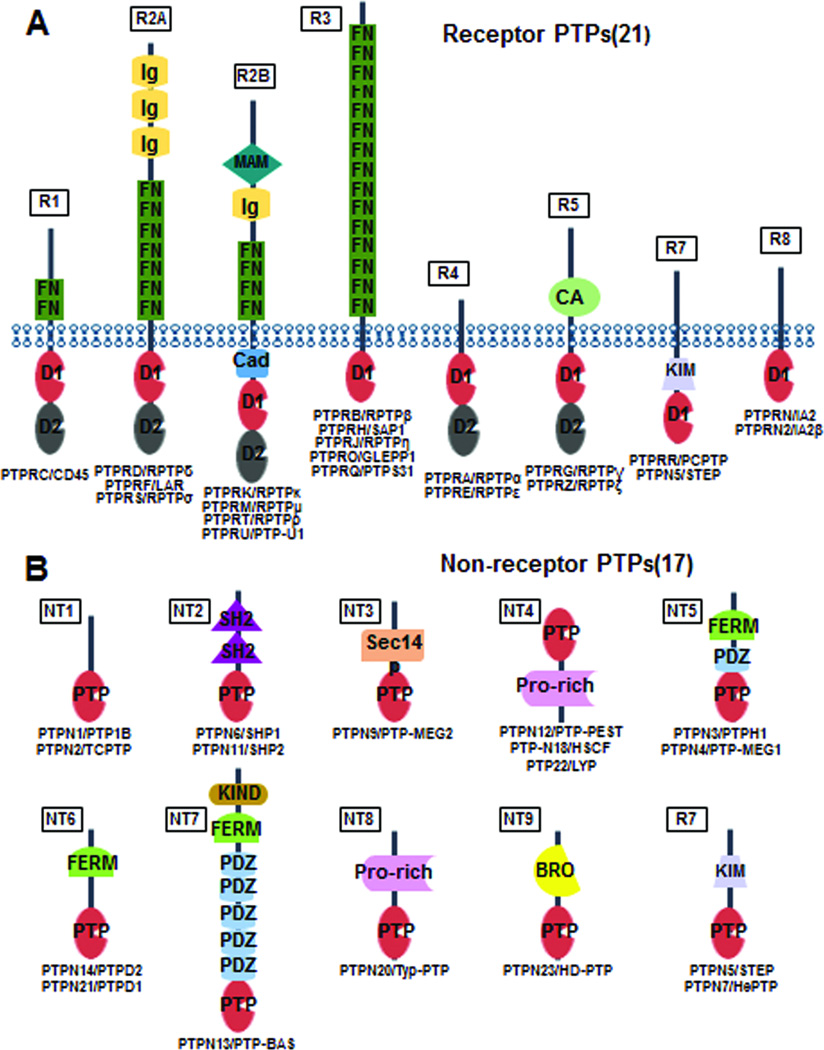
A tyrosine phosphatome refers to all PTPs in a given organism.3 The human genome encodes 107 PTPs.4 Based on the amino acid sequence similarity of their catalytic domains, the 107 PTPs can be divided into four classes:4 (1) Class I PTPs consist of 38 “classical” PTPs and 61 dual-specific protein phosphatases (DSPs). The classic PTPs (Figure 1) strictly recognize phospho-tyrosine residues as substrates and can be further grouped into receptor protein tyrosine phosphatases (RPTPs, 21 members) and non-receptor protein tyrosine phosphatase (NRPTPs, 17 members). The DSPs, in contrast, can remove a phospho-group from tyrosine, serine or threonine residues. (2) Class II PTP only has a single member, which is a low molecular weight PTP. Although it dephosphorylates tyrosine residues in proteins, its catalytic domain is related to bacterial arsenate reductase and differs dramatically from the classic PTPs. (3) Class III PTPs consist of three yeast CDC25 homologs (CDC25a, CDC25b and CDC25c), which are tyrosine/threonine specific phosphatases. (4) Class IV PTPs include four Drosophila Eya homologs (Eya1, Eya2, Eya3 and Eya4), which can dephosphorylate both tyrosine and serine residues.
Figure 1. Classic PTP family proteins.
BRO: baculovirus BRO homology; CA: carbonic anhydrase domain; D1, intracellular tandem phosphatase domain 1; D2, intracellular tandem phosphatase domain 2; FERM: band 4.1/ezrin/radixin/moesin homology; FN: fibronectin type III repeat; Ig: immunoglobulin domain; KIM, kinase interaction motif; KIND: kinase N lobe-like domain; MAM: Meprin, A5 protein, and protein tyrosine phosphatase Mu (MAM) domain; PDZ: postsynaptic density-95/discs large/ZO1 homology; Pro-rich: proline-rich; PTP: protein tyrosine phosphatase catalytic domain; Sec14p: S. cerevisiae phosphatidylinositol transfer protein (Sec14p)-like lipid-binding domain.
The three dimensional structure and catalytic mechanism of PTPs
The three-dimensional structures of the catalytic domains of classical PTPs (RPTPs and NRPTPs) are extremely well conserved.5 Even the catalytic domain structures of the DSPs, class II and III PTPs are variants of the classical PTPs.5 In this review, we focus on the classical PTPs. The overall structure of the catalytic domains of the classical PTPs are assembled by central β-sheets flanked by six α-helices.5 Six loops connect these secondary structures and form the active PTP catalytic core:5 (1) the phosphate-bind loop (P-loop) connects the α-helices 1 (α1)- and β-sheet 1 (β1), which contains the C(X)5R catalytic motif; (2) the Trp-Pro-Asp loop (WPD-loop) connects the α-helices 3 (α3) and β-sheet 5 (β5), which contains the catalytic aspartate residue; (3) the Q-loop contains a glutamine residue that facilitates the catalytic reaction; (4) the phospho-tyrosine (pY) recognition loop (PY-loop), (5) the E-loop connects β5 and β6, which contains a conserved glutamate, and (6) a recently validated second substrate recognition loop (second-site loop), which connects α1 and α2’. Although the topology of the catalytic domains of classic PTPs are well conserved,5 a recent large-scale structure analysis of 22 classic PTPs shows that the surface structures of these catalytic domains are very diverse, a property that may modulate the substrate specificity of different PTPs.
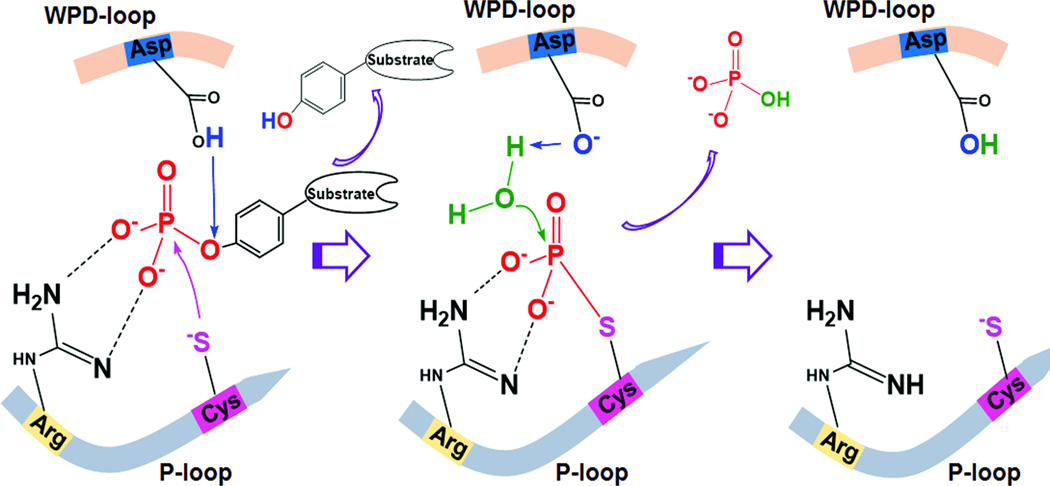
Based on structural and mutagenesis studies, the catalytic reaction of the classic cysteine-based phosphatases can be summarized by two critical steps (Figure 2):6
Nucleophilic attack. Firstly, the catalytic cysteine in the P-loop attacks the phosphorous atom on pY and initiates the breaking of the phosphorus–oxygen bond, whereas the catalytic aspartate in the WPD loop acts as a generate acid to donate a proton to the dephosphorylated tyrosine. This step generates a phosphocysteine intermediate and releases the dephosphorylated substrate. The guanidinium group of the arginine in the C(X)5R motif facilitates the binding of the phosphate group and stabilizes the transition state.
Cysteinyl-phosphate intermediate hydrolysis. Secondly, the catalytic aspartate acts as a general base to extract a proton from a water molecule and facilitates the hydrolysis of the phosphorous-sulfur bond. This reaction results in the release of free phosphate. The water molecule used for hydrolysis is positioned by a conserved glutamine located in the Q-loop.
Figure 2. Catalytic mechanism of PTPs.
The catalytic cysteine in the P-loop initiates the nucleophilic attack of the phosphorous atom on pY and thus breaks the phosphorus–oxygen bond, whereas the catalytic aspartate in the WPD loop acts as a generate acid to donate a proton to the dephosphorylated tyrosine. This step generates a phosphocysteine intermediate and releases the dephosphorylated substrate. This phosphocysteine intermediate is then cleaved by the action of the catalytic aspartate, which acts as a general base to extract a proton from a water molecule and facilitates the hydrolysis of the phosphorous-sulfur bond. This reaction results in the release of free phosphate.
PTP mutations in human cancers
Cancer, in essence, is a genetic disease that is driven by mutations in oncogenes and tumor suppressor genes.7 The first comprehensive effort to uncover somatic mutations of PTPs was performed by Wang et al in colorectal cancers (CRCs).3 We sequenced all PTP family genes and identified six PTPs, including PTPRT, PTPRF, PTPRG, PTPN3, PTPN13 and PTPN14, which are mutated in ~ 26% of CRCs.3 A recent study focusing on RPTPs also identified somatic mutations of PTPRT, PTPRC, PTPRD and PTPRM in head and neck squamous cell carcinomas (HNSCC).8 A series of recent publications has now reported whole-exome (including the PTP family genes) sequencing analyses of a variety of human cancers and most of those data are curated in the COSMIC (catalogue of somatic mutations in cancer) database.9, 10 We searched the latest version (V67) of COSMIC database for somatic mutations of PTP family genes identified in human cancers. A combination of literature review and this search of the COSMIC database (http://cancer.sanger.ac.uk/cancergenome/projects/cosmic/) is listed in table 1, which contains all of the PTP genes known to be mutated in 5% or more of any tumor type. It is evident from the table that PTPRT is the most frequently mutated PTP gene in human cancers. Notably, endometrium and colon cancers harbor many of PTP mutations, although the average numbers of somatic mutations per tumor in these two tumor types are not very high.9 Those data suggest that PTP genes mutations may play particularly important roles in endometrium and colon cancers.
Table 1.
Somatic mutations of PTP superfamily genes in human cancers
| Gene | Mutation frequency and tumor types |
|---|---|
| PTPRB | Angiosarcoma (26%), Colon (5%), Endometrium (10%), Lung (8%) |
| PTPRC | Colon (7%), Endometrium (6%), Lung (6%), Skin (6%), Stomach (6%) |
| PTPRD | Endometrium (9%), Colon (8%), Lung (10%), Esophagus (10%), Skin (10%) |
| PTPRF | Colon (6%), Endometrium (8%) |
| PTPRG | Endometrium (8%), Colon (6%) |
| PTPRH | Endometrium (5%) |
| PTPRJ | Colon (5%), Endometrium (6%) |
| PTPRK | Cervix (7%), Colon (8%), Endometrium (7%), Skin (6%) |
| PTPRM | Colon (8%), Endometrium (7%) |
| PTPRO | Endometrium (6%), Lung (5%), Skin (5%) |
| PTPRP | Colon (6%), Endometrium (6%), Lung (6%), Skin (5%) |
| PTPRQ | Colon (6%), Endometrium (6%) |
| PTPRS | Colon (7%), Endometrium (9%) |
| PTPRT | Bladder (6%), Colon (11%), Endometrium (8%), Esophagus (11%), Head and neck (6%), Lung (10%), Skin (7%), Stomach (9%) |
| PTPRU | Colon (6%), Endometrium (6%) |
| PTPRZ1 | Bladder (6%), Colon (8%), Endometrium (8%), Esophagus (5%), Lung (8%) |
| PTPN1 | Hodgkin Lymphoma and primary mediastinal B cell Lymphoma (20)% |
| PTPN11 | Colon (8%), Leukemia (7%) |
| PTPN13 | Colon (7%), Endometrium (9%) |
| PTPN14 | Colon (5%), Endometrium (8%) |
| PTPN22 | Endometrium (5%) |
| DUSP16 | Endometrium (5%), |
| DUSP27 | Colon (5%), Endometrium (7%), lung (9%) |
| SSH1 | Endometrium (6%) |
| SSH2 | Endometrium (5%) |
| TPIP | Endometrium (6%) |
| TPTE | Colon (6%), Esophagus (7%), Endometrium (8%), Lung (11%), Skin (7%) |
| TNS1 | Colon (9%), Endometrium (8%), Stomach (6%) |
| TNS3 | Bladder (6%), Endometrium (6%) |
| MTM1 | Endometrium (7%) |
| MTMR8 | Endometrium (8%) |
| MTMR13 | Endometrium (8%) |
| INPP4A | Endometrium (5%) |
| INPP4B | Endometrium (7%) |
Here, we provide a detailed review of the most frequently mutated and well-studied PTPs gene in human cancers. These include six RPTPs (PTPRT, PTPRD, PTPRK, PTPRM, PTPB, and PTPRJ) and four NRPTPs (PTPN11, PTPN1, PTPN13 and PTPN14). Table S1 lists all non-synonymous mutations identified in human cancers.
PTPRT
Recent sequencing studies showed that PTPRT is mutated in a variety of human cancers. PTPRT mutations have now been identified in 11% of colon, 6% of bladder, 8% of endometrium, 11% of esophagus, 6% of head and neck, 10% of lung, and 9% of stomach cancers (COSMIC database).3, 8 In addition, PTPRT is also mutated in a small fraction of leukemia, breast, kidney, liver, ovary, pancreas and prostate cancers (the COSMIC database). The tumor-derived mutations are largely missense mutations distributed throughout the protein (COSMIC database).3 However, a portion of PTPRT mutations are nonsense, insertion and deletion mutations that result in premature truncation of the protein,3 suggesting PTPRT may normally functions as a tumor suppressor. This notion is further supported by evidence that, in contrast to wild type mice, PTPRT knockout mice are susceptible to azoxymethane (AOM)-induced colon tumor formation.11 Moreover, unpublished data from our laboratory indicate that PTPRT knockout increases the size of colon tumors generated in mice with a APC+/min genetic background (Zhao Y, et al. unpublished data). Further, it is worth noting that promoter DNA methylation may be another mechanism that leads to loss of PTPRT function in human cancers, as recent studies showed that the promoter of PTPRT is methylated in colon and gastric cancers.12, 13
PTPRT, also known as PTPρ, belongs to the type IIB RPTP subfamily that includes PTPRK/PTPκ, PTPRM/PTPµ and PTPRU/PCP-2 (Figure 1). This subfamily of PTPs share similar structures that consist of an extracellular receptor, a transmembrane domain and a specific intracellular structure (Figure 1). The intracellular segment of the type IIB RPTP subfamily PTPs consists of a cadherin-like juxtamembrane domain and two phosphatase domains (Figure 1). It is generally believed that the membrane proximal PTP domains (D1) function as tyrosine phosphatase, whereas the second PTP domains (D2) have no phosphatase activity.6 However, many tumor derived mutations are located in the second catalytic domain (Table S1),3 suggesting that this domain may have important structural function or harbor yet unidentified enzymatic activity. The extracellular portion of the type IIB RPTPs consist of an MAM (meprin/A5/PTP µ) domain, an Ig domain and four FNIII (fibronectin type III) repeats (Figure 1). It has been shown that the extracellular parts of PTPRK, PTPRM and PTPRT mediate homophilic cell–cell adhesion.14 However, the extracellular part of PTPRU lacks such activity.14 Consistent with the notion that the extracellular domain of PTPRT mediates cell-cell adhesion, Besco et al showed that PTPRT interacts with adherence junction components, such as cadherin proteins and catenin proteins.15 Interestingly, most of the tumor-derived extracellular domain mutations of PTPRT impair cell-cell adhesion.16, 17
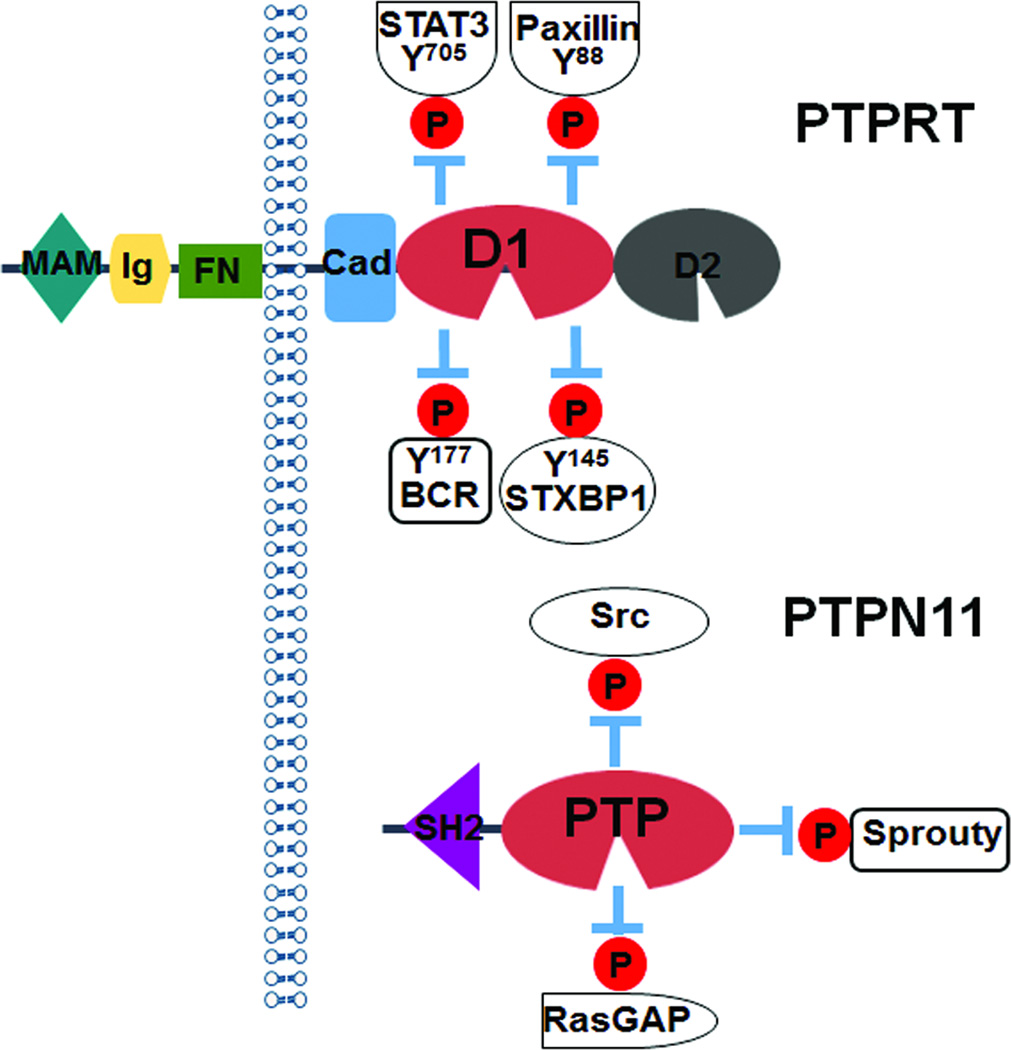
Two cancer-related substrates of PTPRT, STAT3 and paxillin (Figure 3), were identified by a phospho-proteomics approach that screened for loss of pY-containing peptides when the catalytic domains of PTPRT were overexpressed,11, 18 PTPRT dephosphorylates the well-characterized STAT3 Y705 residue in CRC cells.18 Phosphorylation of STAT3 Y705 is key to its activation.19 It has been shown that pY705 STAT3 is up-regulated in a variety of human cancers and that this phosphorylation plays an oncogenic role in tumor development.19 The relevance of STAT3 Y705 phosphorylation in CRC was demonstrated by Zhang et al who showed that STAT3 Y705F mutant knockin CRC cells reduce tumorigenicity.20 Furthermore, PTPRT-regulated STAT3 signaling appears to be critical for head and neck tumorigenesis, in a recent study that showed phospho-STAT3 is up-regulated in HNSCC tissues with PTPRT mutations.8 It is worth noting that up-regulation of STAT3 phosphorylation in the hypothalamus of PTPRT mice results in reduced food intake and renders those mice resistant to high-fat diet-induced obesity.21
Figure 3. Signaling pathways regulated by PTPRT and PTPN11/shp2.
PTPRT negatively regulated signaling transduction pathways by dephosphorylating STAT3, paxillin, BCR and STXBP1 proteins. PTPN11/shp2 positively regulates MAP kinase pathway through de-phosphorylation of inhibitory pY residues in Src, RasGAP and Sprouty.
In contrast to STAT3, the target site of PTPRT on paxillin was a previously uncharacterized Y88 residue.11 Evidence suggesting that the PTPRT-regulated paxillin Y88 phosphorylation may be crucial for colorectal tumorigenesis include the failure of paxillin Y88F knockin CRC cells to form xenograft tumors in nude mice and the up-regulation of pY88 paxillin in a majority of colorectal tumor tissue.11 In addition to STAT3 and paxillin, other substrates of PTPRT, including BRC and Syntaxin-binding protein 1,22, 23 were identified in brain tissue where PTPRT is abundantly expressed (Figure 3). However, the relevance of these substrates to cancer remains to be determined.
PTPRD
The first clue that PTPRD may function as a tumor suppressor came from a survey of homozygous deletions in large panel of human cancer cell lines, which identified PTPRD as a frequent target of deletion in human cancers.24 Subsequent studies further show that PTPRD is deleted in cutaneous squamous cell carcinoma (SCC),25 lung cancer,26 glioblstoma multiforme (GBM), head and neck SCC and laryngeal SCC,27. Somatic mutations of PTPRD was first identified in colorectal cancers.28 Later on, several studies show that PTPRD is mutated in lung cancer, GBM, neuroblastoma,29 melanoma, HNSCC, esophageal and endometrium cancers.30, 31 Aberrant DNA methylation inactivates PTPRD in a significant portion of human GBM, HNSCC, lung and colon cancers that are silenced through PTPRD promoter DNA methylation.31 Expression of PTPRD induces apoptosis30 and inhibits tumor growth in cultured cancer cells,31 consistent with the notion that PTPRD normally functions as a tumor suppressor. Further, a recent study demonstrated that PTPRD knockout enhances gliomagenesis in p16 deletion mice.32
PTPRD belong to the type IIA sub-family RPTPs (Figure 1). The extracellular part of these sub-family RPTPs consists of three Ig domains and 7 FNIII repeats, whereas the intracellular part contains two catalytic domains (Figure 1). The membrane proximal PTP D1 domain of PTPRD harbors phosphatase activity and the C-terminal D2 domain is phosphatase inactive. Like PTPRT, PTPRD can also dephosphorylate STAT3 at the Y705 residue.31, 33 Similarly, PTPRD is also required for appropriate cell-cell adhesion through its interaction with E-cadherin and β-catenin/TCF signaling.34 Overexpression of PTPRD suppressed colon cancer cell migration, suggesting that loss of PTPRD may enhance tumor metastasis.31 In addition, PTPRD may regulate cell migration through its interaction with an actin-binding protein MIM-B (mRNA Missing in Metastasis).35 However, it remains to be determined whether MIM-B is a phosphatase substrate of PTPRD. Recently, aurora kinase A (AURKA) was also identified as a substrate of PTPRD and overexpression of PTPRD destabilized AURKA in neuroblastoma cells.36
PTPRK
PTPRK, also known as PTPκ, is another member of type IIB RPTP subfamily PTPs (Figure 1). It has a similar domain structure to PTPRT. Like PTPRT, the extracellular part of PTPRK mediates homophilic cell-cell adhesion.37 PTPRK is reported to be mutated in breast, colon, cervical, endometrial and skin cancers (COMIC database). It is likely that these tumor-derived PTPRK mutations are loss-of-function mutations. Recently, recurrent PTPRK–RSPO3 gene fusion was found in colorectal cancers.38 In addition, loss of heterozygosity of the PTPRK locus frequently occurs in lymphomas39 and gliomas.40 However, no mouse genetic model has yet proven the tumor suppressive role PTPRK.
PTPRK regulates cell adhesion, migration and proliferation. PTPRK interacts and dephosphorylates EGFR and modulates EGFR signaling.41 Similarly, it also interacts with, and dephosphorylates HER2, thereby repressing basal HER2 signaling and inhibiting cell proliferation in breast cancer cells.42 PTPRK also dephosphorylates β-catenin and negatively regulates the transcriptional activity of β-catenin.43 Further, PTPRK is a transcriptional target of TGF-β signaling.44 Interestingly, EBV infection reduces expression of PTPRK through down-regulation of Smad2 protein levels.45 Moreover, PTPRK protein can be cleaved to generate an extracellular fragment and a transmembrane fragment containing its intracellular domains.46
PTPRM
PTPRM, also known as PTPµ, is the prototype of the type IIB RPTP subfamily PTPs.47 Recent cancer genome studies identify mutations of PTPRM in colon and endometrium cancers as well as HNSCC (COSMIC database).8 Like many of the other phophatases, the PTPRM gene is also methylated in colon cancers.12 It has been shown that PTPRM regulates proliferation, migration and invasion of breast, prostate and brain cancer cells.47, 48 Further, the extracellular part of PTPRM mediates homophilic cell-cell adhesion.49–51 Specifically, PTPRM associates with E-cadherin and modulates E-cadherin-mediated cell-cell adhesion in a prostate cancer cell line.52 It was also reported that PTPRM associates with c-Met.53 Several intracellular substrates of PTPRM that regulate cell adhesion and migration including RACK1, PKCδ, IQGAP1 and p120, PLCγ and BCCIP, were also identified.54, 55, 56
Cleavage products of PTPRM also have cancer–related activities.57 PTPRM can be cleaved by a furin-like protease within the fourth FNIII repeat generating an extracellular E-subunit consisting of MAM, Ig and three FNIII repeats and a transmembrane P-subunit consisting a FNIII repeat, transmembrane and intracellular domains.58 The E-subunit still associates with the P subunit through non-covalent interaction in normal cells. In cancer cells, the P-subunit can be further processed by α- and γ-secretases to produce a membrane free catalytically active intracellular domain (ICD).58 Although full-length and E/P subunit of PTPRM can be detected in normal brain tissues, only the smaller proteolytic fragments are present in brain tumors.58, 59 The ICD fragment can translocate into the nucleus and regulates cell migration.58 However, the exact molecular function of the ICD fragment remains to be determined. Of possible clinical importance in the future, the E-subunit associates with brain tumor cells regardless of the fate of the P-subunit a property that was exploited to image brain tumors in animal models.60
PTPRJ
PTPRJ, also known as DEP1, belongs to the R3 sub-family RPTPs. The protein structures of this sub-family of RPTPs have an extracellular domains consisting of 15 FN III repeats and their intracellular segments harbor a single phosphatase domain (Figure 1). Loss of heterozygosity (LOH) of PTPRJ is common in human cancers including colon,61 breast62 and thyroid63 cancers as well as Meningioma64 and Non-Hodgkin’s Lymphoma.65 LOH of PTPRJ appears to be an early event for colon cancer as it occurs in human aberrant crypt foci, a pre-cancer lesion.66 Interestingly, PTPRJ is epigenetically silenced in Early-Onset Familial Colorectal Cancer.67 Somatic mutations of PTPRJ are observed in ~5% colon cancers and ~6% endometrium cancers (COSMIC database).
Consistent with the notion that PTPRJ may function as a tumor suppressor gene, overexpression of PTPRJ inhibits growth of breast, colon, pancreatic and thyroid cancer cell lines.68,69, 70,71 Interestingly, intratumor injection of adeno-associated viruses (AAVs) expressing PTPRJ suppresses growth of xenograft tumors established by a pancreatic cancer cell line.70 It has been shown that overexpression of PTPRJ causes G1 arrest through stabilization of p27Kip1 proteins.71 Mouse genetic studies mapped PTPRJ as a candidate colon tumor suppressor gene in mouse.72 However, PTPRJ knockout mice do not develop spontaneous tumors.73 It remains to be determined whether PTPRJ knockout mice are susceptible to carcinogen induced tumor development.
It has been shown that PTPRJ regulates multiple signaling pathways. PTPRJ interacts with and dephosphorylates numerous receptor tyrosine kinases (RTKs) including PDGFR, HGFR, EGFR and RET. PTPRJ interacts with and dephosphorylates RET oncogene at Y905 and Y1062 sites and antagonizes the transformation activity of RET.68 PTPRJ is also a negative modulator of the signaling mediated by cytosolic transducers, including phospholipase Cγ1 (PLCγ1), Akt,74 and PI3K.75 Moreover, PTPRJ associates with and dephosphorylates Src on tyrosine residues where phosphorylation inhibits Src kinase activity. Consistently, overexpression of PTPRJ activates Src and enhances cell-matrix adhesion.69 Further, knockdown of PTPRJ in myeloid cell lines results in hyper-phosphorylation of FLT3 and activation of FLT3 signaling to its downstream signaling molecules ERK and STAT5.76 Notably, reduction of PTPRJ enhances leukemogenesis.76 Lastly, PTPRJ itself is a transcriptional target of HIF-α77 and a target of miR-328.78
PTPRB
Protein tyrosine phosphatase receptor B (PTPRB) encodes a vascular endothelium specific phosphatase (VE-PTP). PTPRB mutations are extremely rare in epithelial tumors and leukemia. However, recent whole-exome sequencing identified PTPRB mutations in ~ 26% of angiosarcoma,79 an aggressive malignancy that arises spontaneously or secondarily to ionizing radiation or chronic lymphedema. Most of PTPRB mutations are nonsense mutations or insertions and deletions that cause frameshift mutations,79 suggesting that PTPRB functions as a tumor suppressor in angiosarcoma.
PTPRB plays an essential role in angiogenesis process, as the PTPRB knockout mice are embryonic lethal and show severe defects in vasculature formation.80,81 The primary targets of PTPRB/VE-PTP in endothelial cells are the endothelial cell receptor tyrosine kinase (Tie-2), VEGF receptor-2, VE-cadherin and plakoglobin82–84. Through de-phosphorylation of these substrates, PTPRB regulates endothelial cell polarity, lumen formation and vascular permeability.85, 84 Compared to normal blood vessels, tumor vasculature is abnormal and leaky. Interestingly, inhibition of PTPRB/VE-PTP by small molecule AKB-9778 normalizes the structure and function of tumor vessels.86
PTPN11
PTPN11 is also called Shp2, SH-PTP2, SH-PTP3, PTP1D, PTP2C, or Syp.87 It is one of the few known phosphatases that can function as an oncogene. Gain-of-function germline mutation of PTPN11 was first identified in a developmental disorder Noonan syndrome.88 Subsequently, oncogenic somatic mutations of PTPN11 were also found in over 30% of juvenile myelomonocytic leukemia (JMML) and a small fraction of patients exhibiting myelodysplastic syndrome and acute myeloid leukemia (AML).89 Interestingly, inactivation of PTPN11 leads to disease development as well. Loss-of-function germline mutations of PTPN11 were identified in a congenital heart disorder LEOPARD Syndrome.90 PTPN11/Shp2 protein consists of two SH2 domains (N-SH2 and C-SH2 domains), a central PTP catalytic domain and a C-terminal tail with a proline-rich motif.87 In the basal state, the backside loop of the N-SH2 domain folds into the PTP catalytic pocket, thereby keeping Shp2 in inactivate form. Upon stimulation by growth factors or cytokines, the N-SH2 domains of Shp2 bind to phosphorylated tyrosine residues on adapter proteins or receptor protein tyrosine kinases.87 This event induces a conformational change that leads to exposure of the PTP catalytic pocket to substrates. Most of PTPN11 mutations identified in Noonan syndrome and leukemia are located in the N-SH2 domains.87 These mutations perturb the binding of the N-SH2 domain to the PTP domain and activate its phosphatase activity without stimuli. In contrast, PTPN11 mutations in LEOPARD Syndrome are primarily located in the PTP domain and are enzymatically inactive.91 Intriguingly, recent studies suggest that PTPN11 may also function as a tumor suppressor gene in cancers. Bard-Chapeau et al showed that mice are susceptible to carcinogen-induced hepatocellular carcinoma when PTPN11 is conditionally ablated in liver.92 Moreover, loss-of-function mutation of PTPN11 was found in patients with metachondromatosis.93 A follow-up study demonstrated that mice with PTPN11 inactivated in osteoclasts developed features very similar to metachondromatosis.94
It appears that the primary signaling cascade regulated by PTPN11/Shp2 is the Ras/ERK MAP kinase pathway, as germline mutations of RAS, RAF, MEK1 and MEK2 are identified in Noonan and Noonan-like syndromes.87 Shp2 could activate the MAP kinase pathway through distinct mechanisms (Figure 3):87 (1) it dephosphorylates the inhibitory pY sites on Src family kinases, which in turn sustains activation of the MAP kinase; (2) It dephosphorylates binding sites of RasGAP on specific receptors and adaptor proteins; (3) It dephosphorylates Sprouty proteins, a family of RAS inhibitors. PTPN11/Shp2 also regulates several other intracellular pathways including Jak/Stat, PI3K/AKT, NF-κB and Calcineurin/NFAT signaling pathways.95 Interestingly, recent studies by Qu and colleagues demonstrated that Shp2 regulates the mitotic machinery to maintain chromosomal stability and that it may also regulate targets in mitochondria.96, 97
PTPN1
Protein tyrosine phosphatase non-receptor 1 (PTPN1), which encodes PTP1B, was the first PTP discovered.6 Although it has been speculated that PTPN1 could function as a tumor suppressor, strong genetic evidence has been lacking until a recent study showing that PTPN1 is frequently mutated in classical Hodgkin lymphoma and primary mediastinal B cell lymphoma (PMBCL).98 Using whole-genome and whole-transcriptome sequencing technology, Gunawardana et al found that PTPN1 is mutated somatically in over 20% of Hodgkin lymphoma and PMBCL cases.98 Those tumor-derived mutations appear to be loss-of-function mutations, as a fraction of them are nonsense mutations and some of the missense mutations diminish its phosphatase activity.98
It is well documented that PTP1B negatively regulates insulin and leptin signaling pathways. PTP1B dephosphorylates both insulin receptor (IR) and insulin receptor substrates (IRS), thereby turning off the PI3K/AKT signaling pathway.99 In the leptin and cytokine signaling pathways, PTP1B dephosphorylates the tyrosine kinase JAK2 and thus negatively regulates the JAK/STAT pathway.99 In contrast, PTP1B activates the Src family protein kinases by dephosphorylating inhibitory tyrosine phosphorylation of Src proteins.99 In fact, PTPN1 knockout delays ErbB2-induced mammary tumorigenesis in mice, suggesting that PTPN1 plays an oncogenic role in breast cancer.100 As discussed above, PTPN1 functions as a tumor suppressor in Hodgkin lymphoma and PMBCL, in which it primarily regulates the JAK/STAT pathway. Gunawardana et al showed that tumor-derived PTPN1 mutations result in activation of JAK/STAT signaling.98
PTPN13
Protein tyrosine phosphatase non-receptor 13 (PTPN13), also known as FAP1, was first identified as a Fas-associated protein that modulates Fas-induced apoptosis.101 Inactivation mutations of PTPN13 are found in colorectal, lung and endometrium cancers (COSMIC database).3 It is also epigenetically silenced in non-Hodgkin’s lymphoma, Hodgkin’s lymphoma, breast, gastric and hepatocellular carcinoma cell lines.102 In addition, loss of PTPN13 mRNA and protein expression frequently occurs in NSCLC.103 Consistent with its tumor suppressor functions, overexpression of PTPN13 causes resistance to Fas-induced apoptosis in HNSCC.104 Moreover, PTPN13 expression associates with poorer survival in oral squamous cell carcinoma (OSCC).105 Silencing PTPN13 sensitizes colon cancer cells to oxaliplatin.106 However, PTPN13 expression is associated with better survival of breast cancer patients.107
PTPN13 regulates phosphorylation of both cell surface receptors and intracellular substrates. PTPN13 negatively regulates Her2/Erbb2 phosphorylation, but it is not clear if Her2/Erbb2 is a direct substrate of PTPN13.108 It is also reported that EphrinB1 is a substrate of PTPN13.109 Loss of PTPN13 leads to increased phosphorylation of EphrinB1 and Erk.109 PTPN13 regulates multiple substrates in the PI3K-AKT signaling pathway and negatively impact the signaling of this pathway. It dephosphorylates both IRS1 and p85β. Dephosphorylation of p85β by PTPN13 leads to degradation of p110-free p85β.110 Consequently, negative regulation of the PI3K-AKT signaling by PTPN13 induces apoptosis in breast cancer cell lines110. PTPN13 also regulates APC/ β-catenin pathway. It interacts with APC, inactivates GSK3β kinase activity, results in β-catenin stabilization.111 Additionally, PTPN13 negatively regulates Ras/RAF/MEK/Erk signaling.112 Interestingly, PTPN13 also modulates cytokinesis. PTPN13 interacts with serologically defined colon cancer antigen-3 (SDCCAG3) and regulates cytokinesis.113 Another PTPN13 substrate involved in cytokinesis is Valosin Containing Protein (VCP/p97). Dephosphorylation of VCP/p97 by PTPN13 affects its midbody localization during cytokinesis.114 Lastly, PTPN13 is a target of viral oncoprotein, Bcr-abl and a microRNA.115,116,117 HPV 16 E6 oncoprotein physically associates with and degrades PTPN13 in HNSCC.115 It has been shown that PTPN13 is a target of miR-200 that regulates EMT in colon cancers,116 whereas the expression of Bcr-abl oncoprotein in myeloid progenitor cells up-regulates PTPN13 and causes resistance to Fas-induced apoptosis.117
PTPN14
PTPN14, also known as Pez, PTP36 and PTPD2, consists of an N-terminal FERM (four-point-one, ezrin, radixin, moesin) domain and a C-terminal phosphatase domain.118 PTPN14 is mutated in breast, colon and endometrium cancers.3, 28 Function of PTPN14 as a tumor suppressor gene is supported by the fact that hypomorphic PTPN14 where mutant mice were generated by gene-trapping, displayed lymphatic hyperplasia.119 Furthermore, in library screening with shRNAs against the PTP family genes, PTPN14 was identified as candidate tumor suppressor gene for breast cancer.120 Knocking down PTPN14 enhances anchorage-independent growth of normal immortalized mammary epithelial cells.120
It has been shown that PTPN14 may regulate cell–cell adhesion, cell–matrix adhesion, cell migration and cell growth.118 PTPN14 also regulates tyrosine phosphorylation of β-catenin and modulates cell-cell adhesion.121 Using a phospho-proteomic approach, we identified a list of putative substrates of PTPN14.122 We further validated that p130Cas is a PTPN14 substrate. PTPN14 dephosphorylates p130Cas at the Y128 residue.122 Regulation of p130Cas Y128 phosphorylation plays a role in colorectal tumorigenesis, as the genetically engineered p130Cas Y128F mutant knockin colorectal cancer cell lines display reduced migration and colony formation, impaired anchorage-independent growth, slower xenograft tumor growth in nude mice.122 Recently, several studies demonstrated that PTPN14 interacts with Yap and negatively regulates Yap oncogenic activity.120, 123–125 Overexpression of PTPN14 results in nuclear exclusion of YAP, thereby reducing its transcriptional activity. YAP is shown to be a direct substrate of PTPN14. However, whether the phosphatase activity of PTPN14 is required to regulate Yap activity is controversial. Lastly, PTPN14 also regulates TGF-β gene expression, thereby modulating epithelial–mesenchymal transition.118
Prospective
Recent cancer genomics studies reveal that PTPs are genetically altered in a variety of human cancers, providing compelling evidence that PTPs also play critical roles in tumorigenesis. Although the mutation frequency of individual PTPs is not extremely high, the PTP family genes in aggregate are mutated in a majority of human cancers. A recent analysis found that the mutational rate of PTP family genes ranges from 30% to 80% in various cancers.8 It is interesting that some of the PTPs are mutated in a tissue-specific manner. For example, PTPN1 is only mutated in lymphomas, suggesting that the PTPN1-regulated signal pathways play a particular important role in lymphocytes. Alternatively, differential expression of a PTP in different tissue types may also explain such a phenomenon. Unlike PTKs, functional studies of PTPs still lag behind. Modeling of PTPs functions in tumorigenesis using knockout mice should be fertile ground for future studies. Notably, most of the mutated PTPs are involved in cell adhesion and migration, suggesting that PTPs may play pivotal roles in tumor invasion and metastasis.
With the exception of PTPN11 that functions as an oncogene in leukemia, most PTPs function as tumor suppressor genes. It is challenge to target genetically altered tumor suppressive PTPs for cancer therapy. However, identification of the corresponding kinases and substrates of PTPs may identify novel targets for cancer treatment. In this regard, it is of key importance to develop systematic approaches to identify substrates of PTPs. Phosphatase substrate trapping methods have been very useful for validation of candidate substrates126, but have had limit success for systematic identification of PTP substrates. Recently, we have developed a phospho-proteomic approach to identify PTP substrates systematically, whereby lysates from cell line expressing a control, a WT PTP or a substrate-trapping PTP mutant are digested with trypsin and phosphopeptides are then enriched by an anti-pY antibody and profiled by mass- spectrometry.18, 122 In comparison with the control, pY peptides of candidate substrates are expected to increase in the cell line expressing the substrate-trapping mutant, but to decrease in the cell line expressing the WT PTP. We successfully applied this method to identify multiple substrates of PTPRT and PTPN14.18, 122 It will be interesting to see if this approach is generally applicable to identification of substrates of other PTPs.
Acknowledgement
We thank Dr. Susann Brady-Kalnay for critical reading of the manuscript. This work is supported by NIH grants R01CA127590, P50CA150964 and P30 CA043703.
Footnotes
Conflict of Interest
The authors declare no conflict of interest.
References
- 1.Brognard J, Hunter T. Protein kinase signaling networks in cancer. Curr Opin Genet Dev. 2011;21:4–11. doi: 10.1016/j.gde.2010.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Julien SG, Dubé N, Hardy S, Tremblay ML. Inside the human cancer tyrosine phosphatome. Nat Rev Cancer. 2011;11:35–49. doi: 10.1038/nrc2980. [DOI] [PubMed] [Google Scholar]
- 3.Wang Z, Shen D, Parsons DW, Bardelli A, Sager J, Szabo S, et al. Mutational analysis of the tyrosine phosphatome in colorectal cancers. Science. 2004;304:1164–1166. doi: 10.1126/science.1096096. [DOI] [PubMed] [Google Scholar]
- 4.Alonso A, Sasin J, Bottini N, Friedberg I, Friedberg I, Osterman A, et al. Protein tyrosine phosphatases in the human genome. Cell. 2004;117:699–711. doi: 10.1016/j.cell.2004.05.018. [DOI] [PubMed] [Google Scholar]
- 5.Barr AJ, Ugochukwu E, Lee WH, King ON, Filippakopoulos P, Alfano I, et al. Large-scale structural analysis of the classical human protein tyrosine phosphatome. Cell. 2009;136:352–363. doi: 10.1016/j.cell.2008.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tonks NK. Protein tyrosine phosphatases: from genes, to function, to disease. Nat Rev Mol Cell Biol. 2006;7:833–846. doi: 10.1038/nrm2039. [DOI] [PubMed] [Google Scholar]
- 7.Vogelstein B, Kinzler KW. Cancer genes and the pathways they control. Nat Med. 2004;10:789–799. doi: 10.1038/nm1087. [DOI] [PubMed] [Google Scholar]
- 8.Lui VW, Peyser ND, Ng PK, Hritz J, Zeng Y, Lu Y, et al. Frequent mutation of receptor protein tyrosine phosphatases provides a mechanism for STAT3 hyperactivation in head and neck cancer. Proceedings of the National Academy of Sciences of the United States of America. 2014;111:1114–1119. doi: 10.1073/pnas.1319551111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vogelstein B, Papadopoulos N, Velculescu VE, Zhou S, Diaz LA, Jr, Kinzler KW. Cancer genome landscapes. Science. 2013;339:1546–1558. doi: 10.1126/science.1235122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garraway LA, Lander ES. Lessons from the cancer genome. Cell. 2013;153:17–37. doi: 10.1016/j.cell.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 11.Zhao Y, Zhang X, Guda K, Lawrence E, Sun Q, Watanabe T, et al. Identification and functional characterization of paxillin as a target of protein tyrosine phosphatase receptor T. Proceedings of the National Academy of Sciences of the United States of America. 2010;107:2592–2597. doi: 10.1073/pnas.0914884107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laczmanska I, Karpinski P, Bebenek M, Sedziak T, Ramsey D, Szmida E, et al. Protein tyrosine phosphatase receptor-like genes are frequently hypermethylated in sporadic colorectal cancer. Journal of human genetics. 2013;58:11–15. doi: 10.1038/jhg.2012.119. [DOI] [PubMed] [Google Scholar]
- 13.Liu Z, Zhang J, Gao Y, Pei L, Zhou J, Gu L, et al. Large-Scale Characterization of DNA Methylation Changes in Human Gastric Carcinomas with and without Metastasis. Clinical cancer research : an official journal of the American Association for Cancer Research. 2014 doi: 10.1158/1078-0432.CCR-13-3380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Becka S, Zhang P, Craig SE, Lodowski DT, Wang Z, Brady-Kalnay SM. Characterization of the adhesive properties of the type IIb subfamily receptor protein tyrosine phosphatases. Cell Commun Adhes. 2010;17:34–47. doi: 10.3109/15419061.2010.487957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Besco JA, Hooft van Huijsduijnen R, Frostholm A, Rotter A. Intracellular substrates of brain-enriched receptor protein tyrosine phosphatase rho (RPTPrho/PTPRT) Brain Res. 2006;1116:50–57. doi: 10.1016/j.brainres.2006.07.122. [DOI] [PubMed] [Google Scholar]
- 16.Yu J, Becka S, Zhang P, Zhang X, Brady-Kalnay SM, Wang Z. Tumor-Derived Extracellular Mutations of PTPRT/PTP{rho} Are Defective in Cell Adhesion. Mol Cancer Res. 2008;6:1106–1113. doi: 10.1158/1541-7786.MCR-07-2123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang P, Becka S, Craig SE, Lodowski DT, Brady-Kalnay SM, Wang Z. Cancer-derived mutations in the fibronectin III repeats of PTPRT/PTPrho inhibit cell-cell aggregation. Cell Commun Adhes. 2009;16:146–153. doi: 10.3109/15419061003653771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang X, Guo A, Yu J, Possemato A, Chen Y, Zheng W, et al. Identification of STAT3 as a substrate of receptor protein tyrosine phosphatase T. PNAS. 2007;104:4060–4064. doi: 10.1073/pnas.0611665104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Darnell JE. Validating Stat3 in cancer therapy. Nat Med. 2005;11:595–596. doi: 10.1038/nm0605-595. [DOI] [PubMed] [Google Scholar]
- 20.Zhang P, Zhao Y, Zhu X, Sedwick D, Zhang X, Wang Z. Cross-talk between Phospho-STAT3 and PLC{gamma}1 Plays a Critical Role in Colorectal Tumorigenesis. Mol Cancer Res. 2011;9:1418–1428. doi: 10.1158/1541-7786.MCR-11-0147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Feng X, Scott A, Wang Y, Wang L, Zhao Y, Doerner S, et al. PTPRT Regulates High-Fat Diet-Induced Obesity and Insulin Resistance. PloS one. 2014;9:e100783. doi: 10.1371/journal.pone.0100783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park AR, Oh D, Lim SH, Choi J, Moon J, Yu DY, et al. Regulation of dendritic arborization by BCR Rac1 GTPase-activating protein, a substrate of PTPRT. Journal of cell science. 2012;125:4518–4531. doi: 10.1242/jcs.105502. [DOI] [PubMed] [Google Scholar]
- 23.Lim SH, Moon J, Lee M, Lee JR. PTPRT regulates the interaction of Syntaxin-binding protein 1 with Syntaxin 1 through dephosphorylation of specific tyrosine residue. Biochemical and biophysical research communications. 2013;439:40–46. doi: 10.1016/j.bbrc.2013.08.033. [DOI] [PubMed] [Google Scholar]
- 24.Cox C, Bignell G, Greenman C, Stabenau A, Warren W, Stephens P, et al. A survey of homozygous deletions in human cancer genomes. Proceedings of the National Academy of Sciences of the United States of America. 2005;102:4542–4547. doi: 10.1073/pnas.0408593102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Purdie KJ, Lambert SR, Teh MT, Chaplin T, Molloy G, Raghavan M, et al. Allelic imbalances and microdeletions affecting the PTPRD gene in cutaneous squamous cell carcinomas detected using single nucleotide polymorphism microarray analysis. Genes, chromosomes & cancer. 2007;46:661–669. doi: 10.1002/gcc.20447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kohno T, Otsuka A, Girard L, Sato M, Iwakawa R, Ogiwara H, et al. A catalog of genes homozygously deleted in human lung cancer and the candidacy of PTPRD as a tumor suppressor gene. Genes, chromosomes & cancer. 2010;49:342–352. doi: 10.1002/gcc.20746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Giefing M, Zemke N, Brauze D, Kostrzewska-Poczekaj M, Luczak M, Szaumkessel M, et al. High resolution ArrayCGH and expression profiling identifies PTPRD and PCDH17/PCH68 as tumor suppressor gene candidates in laryngeal squamous cell carcinoma. Genes, chromosomes & cancer. 2011;50:154–166. doi: 10.1002/gcc.20840. [DOI] [PubMed] [Google Scholar]
- 28.Sjoblom T, Jones S, Wood LD, Parsons DW, Lin J, Barber TD, et al. The consensus coding sequences of human breast and colorectal cancers. Science. 2006;314:268–274. doi: 10.1126/science.1133427. [DOI] [PubMed] [Google Scholar]
- 29.Weir BA, Woo MS, Getz G, Perner S, Ding L, Beroukhim R, et al. Characterizing the cancer genome in lung adenocarcinoma. Nature. 2007;450:893–898. doi: 10.1038/nature06358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Solomon DA, Kim J-S, Cronin JC, Sibenaller Z, Ryken T, Rosenberg SA, et al. Mutational Inactivation of PTPRD in Glioblastoma Multiforme and Malignant Melanoma. Cancer research. 2008;68:10300–10306. doi: 10.1158/0008-5472.CAN-08-3272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Veeriah S, Brennan C, Meng S, Singh B, Fagin JA, Solit DB, et al. The tyrosine phosphatase PTPRD is a tumor suppressor that is frequently inactivated and mutated in glioblastoma and other human cancers. Proceedings of the National Academy of Sciences of the United States of America. 2009;106:9435–9440. doi: 10.1073/pnas.0900571106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ortiz B, Fabius AW, Wu WH, Pedraza A, Brennan CW, Schultz N, et al. Loss of the tyrosine phosphatase PTPRD leads to aberrant STAT3 activation and promotes gliomagenesis. Proceedings of the National Academy of Sciences of the United States of America. 2014;111:8149–8154. doi: 10.1073/pnas.1401952111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jiang Y, Janku F, Subbiah V, Angelo LS, Naing A, Anderson PM, et al. Germline PTPRD mutations in Ewing sarcoma: biologic and clinical implications. Oncotarget. 2013;4:884–889. doi: 10.18632/oncotarget.1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Funato K, Yamazumi Y, Oda T, Akiyama T. Tyrosine phosphatase PTPRD suppresses colon cancer cell migration in coordination with CD44. Experimental and therapeutic medicine. 2011;2:457–463. doi: 10.3892/etm.2011.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Woodings JA, Sharp SJ, Machesky LM. MIM-B, a putative metastasis suppressor protein, binds to actin and to protein tyrosine phosphatase delta. The Biochemical journal. 2003;371:463–471. doi: 10.1042/BJ20021962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Meehan M, Parthasarathi L, Moran N, Jefferies CA, Foley N, Lazzari E, et al. Protein tyrosine phosphatase receptor delta acts as a neuroblastoma tumor suppressor by destabilizing the aurora kinase A oncogene. Molecular cancer. 2012;11:6. doi: 10.1186/1476-4598-11-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sap J, Jiang YP, Friedlander D, Grumet M, Schlessinger J. Receptor tyrosine phosphatase R-PTP-kappa mediates homophilic binding. Molecular and cellular biology. 1994;14:1–9. doi: 10.1128/mcb.14.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Seshagiri S, Stawiski EW, Durinck S, Modrusan Z, Storm EE, Conboy CB, et al. Recurrent R-spondin fusions in colon cancer. Nature. 2012;488:660–664. doi: 10.1038/nature11282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nakamura M, Kishi M, Sakaki T, Hashimoto H, Nakase H, Shimada K, et al. Novel tumor suppressor loci on 6q22–23 in primary central nervous system lymphomas. Cancer research. 2003;63:737–741. [PubMed] [Google Scholar]
- 40.Agarwal S, Al-Keilani MS, Alqudah MA, Sibenaller ZA, Ryken TC, Assem M. Tumor derived mutations of protein tyrosine phosphatase receptor type k affect its function and alter sensitivity to chemotherapeutics in glioma. PloS one. 2013;8:e62852. doi: 10.1371/journal.pone.0062852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xu Y, Tan LJ, Grachtchouk V, Voorhees JJ, Fisher GJ. Receptor-type protein-tyrosine phosphatase-kappa regulates epidermal growth factor receptor function. The Journal of biological chemistry. 2005;280:42694–42700. doi: 10.1074/jbc.M507722200. [DOI] [PubMed] [Google Scholar]
- 42.Lucci MA, Orlandi R, Triulzi T, Tagliabue E, Balsari A, Villa-Moruzzi E. Expression profile of tyrosine phosphatases in HER2 breast cancer cells and tumors. Cellular oncology : the official journal of the International Society for Cellular Oncology. 2010;32:361–372. doi: 10.3233/CLO-2010-0520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Novellino L, De Filippo A, Deho P, Perrone F, Pilotti S, Parmiani G, et al. PTPRK negatively regulates transcriptional activity of wild type and mutated oncogenic beta-catenin and affects membrane distribution of beta-catenin/E-cadherin complexes in cancer cells. Cellular signalling. 2008;20:872–883. doi: 10.1016/j.cellsig.2007.12.024. [DOI] [PubMed] [Google Scholar]
- 44.Wang SE, Wu FY, Shin I, Qu S, Arteaga CL. Transforming growth factor {beta} (TGF-{beta})-Smad target gene protein tyrosine phosphatase receptor type kappa is required for TGF-{beta} function. Molecular and cellular biology. 2005;25:4703–4715. doi: 10.1128/MCB.25.11.4703-4715.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Flavell JR, Baumforth KR, Wood VH, Davies GL, Wei W, Reynolds GM, et al. Down-regulation of the TGF-beta target gene, PTPRK, by the Epstein-Barr virus encoded EBNA1 contributes to the growth and survival of Hodgkin lymphoma cells. Blood. 2008;111:292–301. doi: 10.1182/blood-2006-11-059881. [DOI] [PubMed] [Google Scholar]
- 46.Kim YS, Jung JA, Kim HJ, Ahn YH, Yoo JS, Oh S, et al. Galectin-3 binding protein promotes cell motility in colon cancer by stimulating the shedding of protein tyrosine phosphatase kappa by proprotein convertase 5. Biochemical and biophysical research communications. 2011;404:96–102. doi: 10.1016/j.bbrc.2010.11.071. [DOI] [PubMed] [Google Scholar]
- 47.Brady-Kalnay SM. Protein tyrosine phosphatases. In: Beckerle M, editor. Cell Adhesion: Frontiers in Molecular Biology. Vol. 39. Oxford, UK: Oxford University Press; pp. 217–258. [Google Scholar]
- 48.Craig SE, Brady-Kalnay SM. Cancer cells cut homophilic cell adhesion molecules and run. Cancer research. 2011;71:303–309. doi: 10.1158/0008-5472.CAN-10-2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brady-Kalnay SM, Flint AJ, Tonks NK. Homophilic binding of PTP mu, a receptor-type protein tyrosine phosphatase, can mediate cell-cell aggregation. The Journal of cell biology. 1993;122:961–972. doi: 10.1083/jcb.122.4.961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Brady-Kalnay SM, Tonks NK. Identification of the homophilic binding site of the receptor protein tyrosine phosphatase PTP mu. The Journal of biological chemistry. 1994;269:28472–28477. [PubMed] [Google Scholar]
- 51.Gebbink MF, Zondag GC, Wubbolts RW, Beijersbergen RL, van Etten I, Moolenaar WH. Cell-cell adhesion mediated by a receptor-like protein tyrosine phosphatase. The Journal of biological chemistry. 1993;268:16101–16104. [PubMed] [Google Scholar]
- 52.Hellberg CB, Burden-Gulley SM, Pietz GE, Brady-Kalnay SM. Expression of the receptor protein-tyrosine phosphatase, PTPmu, restores E-cadherin-dependent adhesion in human prostate carcinoma cells. The Journal of biological chemistry. 2002;277:11165–11173. doi: 10.1074/jbc.M112157200. [DOI] [PubMed] [Google Scholar]
- 53.Hiscox S, Jiang WG. Association of the HGF/SF receptor, c-met, with the cell-surface adhesion molecule, E-cadherin, and catenins in human tumor cells. Biochemical and biophysical research communications. 1999;261:406–411. doi: 10.1006/bbrc.1999.1002. [DOI] [PubMed] [Google Scholar]
- 54.Mourton T, Hellberg CB, Burden-Gulley SM, Hinman J, Rhee A, Brady-Kalnay SM. The PTPmu protein-tyrosine phosphatase binds and recruits the scaffolding protein RACK1 to cell-cell contacts. The Journal of biological chemistry. 2001;276:14896–14901. doi: 10.1074/jbc.M010823200. [DOI] [PubMed] [Google Scholar]
- 55.Phillips-Mason PJ, Mourton T, Major DL, Brady-Kalnay SM. BCCIP associates with the receptor protein tyrosine phosphatase PTPmu. Journal of cellular biochemistry. 2008;105:1059–1072. doi: 10.1002/jcb.21907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Phillips-Mason PJ, Kaur H, Burden-Gulley SM, Craig SE, Brady-Kalnay SM. Identification of phospholipase C gamma1 as a protein tyrosine phosphatase mu substrate that regulates cell migration. Journal of cellular biochemistry. 2011;112:39–48. doi: 10.1002/jcb.22710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Phillips-Mason PJ, Craig SE, Brady-Kalnay SM. Should I stay or should I go? Shedding of RPTPs in cancer cells switches signals from stabilizing cell-cell adhesion to driving cell migration. Cell adhesion & migration. 2011;5:298–305. doi: 10.4161/cam.5.4.16970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Burgoyne AM, Phillips-Mason PJ, Burden-Gulley SM, Robinson S, Sloan AE, Miller RH, et al. Proteolytic Cleavage of Protein Tyrosine Phosphatase {micro} Regulates Glioblastoma Cell Migration. Cancer research. 2009;69:6960–6968. doi: 10.1158/0008-5472.CAN-09-0863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Phillips-Mason PJ, Craig SE, Brady-Kalnay SM. A Protease Storm Cleaves a Cell-Cell Adhesion Molecule in Cancer: Multiple Proteases Converge to Regulate PTPmu in Glioma Cells. Journal of cellular biochemistry. 2014 doi: 10.1002/jcb.24824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Burden-Gulley SM, Gates TJ, Burgoyne AM, Cutter JL, Lodowski DT, Robinson S, et al. A novel molecular diagnostic of glioblastomas: detection of an extracellular fragment of protein tyrosine phosphatase mu. Neoplasia. 2010;12:305–316. doi: 10.1593/neo.91940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ruivenkamp C, Hermsen M, Postma C, Klous A, Baak J, Meijer G, et al. LOH of PTPRJ occurs early in colorectal cancer and is associated with chromosomal loss of 18q12–21. Oncogene. 2003;22:3472–3474. doi: 10.1038/sj.onc.1206246. [DOI] [PubMed] [Google Scholar]
- 62.Lesueur F, Pharoah PD, Laing S, Ahmed S, Jordan C, Smith PL, et al. Allelic association of the human homologue of the mouse modifier Ptprj with breast cancer. Human molecular genetics. 2005;14:2349–2356. doi: 10.1093/hmg/ddi237. [DOI] [PubMed] [Google Scholar]
- 63.Iuliano R, Le Pera I, Cristofaro C, Baudi F, Arturi F, Pallante P, et al. The tyrosine phosphatase PTPRJ/DEP-1 genotype affects thyroid carcinogenesis. Oncogene. 2004;23:8432–8438. doi: 10.1038/sj.onc.1207766. [DOI] [PubMed] [Google Scholar]
- 64.Petermann A, Haase D, Wetzel A, Balavenkatraman KK, Tenev T, Guhrs KH, et al. Loss of the protein-tyrosine phosphatase DEP-1/PTPRJ drives meningioma cell motility. Brain pathology. 2011;21:405–418. doi: 10.1111/j.1750-3639.2010.00464.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Aya-Bonilla C, Green MR, Camilleri E, Benton M, Keane C, Marlton P, et al. High-resolution loss of heterozygosity screening implicates PTPRJ as a potential tumor suppressor gene that affects susceptibility to Non-Hodgkin's lymphoma. Genes, chromosomes & cancer. 2013;52:467–479. doi: 10.1002/gcc.22044. [DOI] [PubMed] [Google Scholar]
- 66.Luo L, Shen GQ, Stiffler KA, Wang QK, Pretlow TG, Pretlow TP. Loss of heterozygosity in human aberrant crypt foci (ACF), a putative precursor of colon cancer. Carcinogenesis. 2006;27:1153–1159. doi: 10.1093/carcin/bgi354. [DOI] [PubMed] [Google Scholar]
- 67.Venkatachalam R, Ligtenberg MJ, Hoogerbrugge N, Schackert HK, Gorgens H, Hahn MM, et al. Germline epigenetic silencing of the tumor suppressor gene PTPRJ in early-onset familial colorectal cancer. Gastroenterology. 2010;139:2221–2224. doi: 10.1053/j.gastro.2010.08.063. [DOI] [PubMed] [Google Scholar]
- 68.Keane MM, Lowrey GA, Ettenberg SA, Dayton MA, Lipkowitz S. The protein tyrosine phosphatase DEP-1 is induced during differentiation and inhibits growth of breast cancer cells. Cancer research. 1996;56:4236–4243. [PubMed] [Google Scholar]
- 69.Balavenkatraman KK, Jandt E, Friedrich K, Kautenburger T, Pool-Zobel BL, Ostman A, et al. DEP-1 protein tyrosine phosphatase inhibits proliferation and migration of colon carcinoma cells and is upregulated by protective nutrients. Oncogene. 2006;25:6319–6324. doi: 10.1038/sj.onc.1209647. [DOI] [PubMed] [Google Scholar]
- 70.Trapasso F, Yendamuri S, Dumon KR, Iuliano R, Cesari R, Feig B, et al. Restoration of receptor-type protein tyrosine phosphatase eta function inhibits human pancreatic carcinoma cell growth in vitro and in vivo. Carcinogenesis. 2004;25:2107–2114. doi: 10.1093/carcin/bgh224. [DOI] [PubMed] [Google Scholar]
- 71.Trapasso F, Iuliano R, Boccia A, Stella A, Visconti R, Bruni P, et al. Rat protein tyrosine phosphatase eta suppresses the neoplastic phenotype of retrovirally transformed thyroid cells through the stabilization of p27(Kip1) Molecular and cellular biology. 2000;20:9236–9246. doi: 10.1128/mcb.20.24.9236-9246.2000. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 72.Ruivenkamp CA, van Wezel T, Zanon C, Stassen AP, Vlcek C, Csikos T, et al. Ptprj is a candidate for the mouse colon-cancer susceptibility locus Scc1 and is frequently deleted in human cancers. Nature genetics. 2002;31:295–300. doi: 10.1038/ng903. [DOI] [PubMed] [Google Scholar]
- 73.Trapasso F, Drusco A, Costinean S, Alder H, Aqeilan RI, Iuliano R, et al. Genetic ablation of Ptprj, a mouse cancer susceptibility gene, results in normal growth and development and does not predispose to spontaneous tumorigenesis. DNA and cell biology. 2006;25:376–382. doi: 10.1089/dna.2006.25.376. [DOI] [PubMed] [Google Scholar]
- 74.Omerovic J, Clague MJ, Prior IA. Phosphatome profiling reveals PTPN2, PTPRJ and PTEN as potent negative regulators of PKB/Akt activation in Ras-mutated cancer cells. The Biochemical journal. 2010;426:65–72. doi: 10.1042/BJ20091413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Paduano F, Ortuso F, Campiglia P, Raso C, Iaccino E, Gaspari M, et al. Isolation and functional characterization of peptide agonists of PTPRJ, a tyrosine phosphatase receptor endowed with tumor suppressor activity. ACS chemical biology. 2012;7:1666–1676. doi: 10.1021/cb300281t. [DOI] [PubMed] [Google Scholar]
- 76.Arora D, Stopp S, Bohmer SA, Schons J, Godfrey R, Masson K, et al. Protein-tyrosine phosphatase DEP-1 controls receptor tyrosine kinase FLT3 signaling. The Journal of biological chemistry. 2011;286:10918–10929. doi: 10.1074/jbc.M110.205021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Casagrande S, Ruf M, Rechsteiner M, Morra L, Brun-Schmid S, von Teichman A, et al. The protein tyrosine phosphatase receptor type J is regulated by the pVHL-HIF axis in clear cell renal cell carcinoma. The Journal of pathology. 2013;229:525–534. doi: 10.1002/path.4107. [DOI] [PubMed] [Google Scholar]
- 78.Paduano F, Dattilo V, Narciso D, Bilotta A, Gaudio E, Menniti M, et al. Protein tyrosine phosphatase PTPRJ is negatively regulated by microRNA-328. The FEBS journal. 2013;280:401–412. doi: 10.1111/j.1742-4658.2012.08624.x. [DOI] [PubMed] [Google Scholar]
- 79.Behjati S, Tarpey PS, Sheldon H, Martincorena I, Van Loo P, Gundem G, et al. Recurrent PTPRB and PLCG1 mutations in angiosarcoma. Nature genetics. 2014;46:376–379. doi: 10.1038/ng.2921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Dominguez MG, Hughes VC, Pan L, Simmons M, Daly C, Anderson K, et al. Vascular endothelial tyrosine phosphatase (VE-PTP)-null mice undergo vasculogenesis but die embryonically because of defects in angiogenesis. Proceedings of the National Academy of Sciences of the United States of America. 2007;104:3243–3248. doi: 10.1073/pnas.0611510104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Baumer S, Keller L, Holtmann A, Funke R, August B, Gamp A, et al. Vascular endothelial cell-specific phosphotyrosine phosphatase (VE-PTP) activity is required for blood vessel development. Blood. 2006;107:4754–4762. doi: 10.1182/blood-2006-01-0141. [DOI] [PubMed] [Google Scholar]
- 82.Winderlich M, Keller L, Cagna G, Broermann A, Kamenyeva O, Kiefer F, et al. VE-PTP controls blood vessel development by balancing Tie-2 activity. The Journal of cell biology. 2009;185:657–671. doi: 10.1083/jcb.200811159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mellberg S, Dimberg A, Bahram F, Hayashi M, Rennel E, Ameur A, et al. Transcriptional profiling reveals a critical role for tyrosine phosphatase VE-PTP in regulation of VEGFR2 activity and endothelial cell morphogenesis. FASEB journal : official publication of the Federation of American Societies for Experimental Biology. 2009;23:1490–1502. doi: 10.1096/fj.08-123810. [DOI] [PubMed] [Google Scholar]
- 84.Broermann A, Winderlich M, Block H, Frye M, Rossaint J, Zarbock A, et al. Dissociation of VE-PTP from VE-cadherin is required for leukocyte extravasation and for VEGF-induced vascular permeability in vivo. The Journal of experimental medicine. 2011;208:2393–2401. doi: 10.1084/jem.20110525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hayashi M, Majumdar A, Li X, Adler J, Sun Z, Vertuani S, et al. VE-PTP regulates VEGFR2 activity in stalk cells to establish endothelial cell polarity and lumen formation. Nature communications. 2013;4:1672. doi: 10.1038/ncomms2683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Goel S, Gupta N, Walcott BP, Snuderl M, Kesler CT, Kirkpatrick ND, et al. Effects of vascular-endothelial protein tyrosine phosphatase inhibition on breast cancer vasculature and metastatic progression. Journal of the National Cancer Institute. 2013;105:1188–1201. doi: 10.1093/jnci/djt164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Liu X, Qu CK. Protein Tyrosine Phosphatase SHP-2 (PTPN11) in Hematopoiesis and Leukemogenesis. Journal of signal transduction. 2011;2011:195239. doi: 10.1155/2011/195239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Tartaglia M, Mehler EL, Goldberg R, Zampino G, Brunner HG, Kremer H, et al. Mutations in PTPN11, encoding the protein tyrosine phosphatase SHP-2, cause Noonan syndrome. Nature genetics. 2001;29:465–468. doi: 10.1038/ng772. [DOI] [PubMed] [Google Scholar]
- 89.Tartaglia M, Niemeyer CM, Fragale A, Song X, Buechner J, Jung A, et al. Somatic mutations in PTPN11 in juvenile myelomonocytic leukemia, myelodysplastic syndromes and acute myeloid leukemia. Nature genetics. 2003;34:148–150. doi: 10.1038/ng1156. [DOI] [PubMed] [Google Scholar]
- 90.Legius E, Schrander-Stumpel C, Schollen E, Pulles-Heintzberger C, Gewillig M, Fryns JP. PTPN11 mutations in LEOPARD syndrome. Journal of medical genetics. 2002;39:571–574. doi: 10.1136/jmg.39.8.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lauriol J, Kontaridis MI. PTPN11-associated mutations in the heart: has LEOPARD changed Its RASpots? Trends in cardiovascular medicine. 2011;21:97–104. doi: 10.1016/j.tcm.2012.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bard-Chapeau EA, Li S, Ding J, Zhang SS, Zhu HH, Princen F, et al. Ptpn11/Shp2 acts as a tumor suppressor in hepatocellular carcinogenesis. Cancer cell. 2011;19:629–639. doi: 10.1016/j.ccr.2011.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bowen ME, Boyden ED, Holm IA, Campos-Xavier B, Bonafe L, Superti-Furga A, et al. Loss-of-function mutations in PTPN11 cause metachondromatosis, but not Ollier disease or Maffucci syndrome. PLoS genetics. 2011;7:e1002050. doi: 10.1371/journal.pgen.1002050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Yang W, Wang J, Moore DC, Liang H, Dooner M, Wu Q, et al. Ptpn11 deletion in a novel progenitor causes metachondromatosis by inducing hedgehog signalling. Nature. 2013;499:491–495. doi: 10.1038/nature12396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Qu CK. Role of the SHP-2 tyrosine phosphatase in cytokine-induced signaling and cellular response. Biochimica et biophysica acta. 2002;1592:297–301. doi: 10.1016/s0167-4889(02)00322-1. [DOI] [PubMed] [Google Scholar]
- 96.Zheng H, Li S, Hsu P, Qu CK. Induction of a tumor-associated activating mutation in protein tyrosine phosphatase Ptpn11 (Shp2) enhances mitochondrial metabolism, leading to oxidative stress and senescence. The Journal of biological chemistry. 2013;288:25727–25738. doi: 10.1074/jbc.M113.462291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Liu X, Zheng H, Qu CK. Protein tyrosine phosphatase Shp2 (Ptpn11) plays an important role in maintenance of chromosome stability. Cancer research. 2012;72:5296–5306. doi: 10.1158/0008-5472.CAN-12-1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gunawardana J, Chan FC, Telenius A, Woolcock B, Kridel R, Tan KL, et al. Recurrent somatic mutations of PTPN1 in primary mediastinal B cell lymphoma and Hodgkin lymphoma. Nature genetics. 2014;46:329–335. doi: 10.1038/ng.2900. [DOI] [PubMed] [Google Scholar]
- 99.Yip SC, Saha S, Chernoff J. PTP1B: a double agent in metabolism and oncogenesis. Trends in biochemical sciences. 2010;35:442–449. doi: 10.1016/j.tibs.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bentires-Alj M, Neel BG. Protein-tyrosine phosphatase 1B is required for HER2/Neu-induced breast cancer. Cancer research. 2007;67:2420–2424. doi: 10.1158/0008-5472.CAN-06-4610. [DOI] [PubMed] [Google Scholar]
- 101.Freiss G, Chalbos D. PTPN13/PTPL1: an important regulator of tumor aggressiveness. Anti-cancer agents in medicinal chemistry. 2011;11:78–88. doi: 10.2174/187152011794941262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ying J, Li H, Cui Y, Wong AH, Langford C, Tao Q. Epigenetic disruption of two proapoptotic genes MAPK10/JNK3 and PTPN13/FAP-1 in multiple lymphomas and carcinomas through hypermethylation of a common bidirectional promoter. Leukemia. 2006;20:1173–1175. doi: 10.1038/sj.leu.2404193. [DOI] [PubMed] [Google Scholar]
- 103.Scrima M, De Marco C, De Vita F, Fabiani F, Franco R, Pirozzi G, et al. The nonreceptor-type tyrosine phosphatase PTPN13 is a tumor suppressor gene in non-small cell lung cancer. The American journal of pathology. 2012;180:1202–1214. doi: 10.1016/j.ajpath.2011.11.038. [DOI] [PubMed] [Google Scholar]
- 104.Wieckowski E, Atarashi Y, Stanson J, Sato TA, Whiteside TL. FAP-1-mediated activation of NF-kappaB induces resistance of head and neck cancer to Fas-induced apoptosis. Journal of cellular biochemistry. 2007;100:16–28. doi: 10.1002/jcb.20922. [DOI] [PubMed] [Google Scholar]
- 105.Nariai Y, Mishima K, Yoshimura Y, Sekine J. FAP-1 and NF-kappaB expressions in oral squamous cell carcinoma as potential markers for chemo-radio sensitivity and prognosis. International journal of oral and maxillofacial surgery. 2011;40:419–426. doi: 10.1016/j.ijom.2010.10.020. [DOI] [PubMed] [Google Scholar]
- 106.Xiao ZY, Wu W, Eagleton N, Chen HQ, Shao J, Teng H, et al. Silencing Fas-associated phosphatase 1 expression enhances efficiency of chemotherapy for colon carcinoma with oxaliplatin. World journal of gastroenterology : WJG. 2010;16:112–118. doi: 10.3748/wjg.v16.i1.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Revillion F, Puech C, Rabenoelina F, Chalbos D, Peyrat JP, Freiss G. Expression of the putative tumor suppressor gene PTPN13/PTPL1 is an independent prognostic marker for overall survival in breast cancer. International journal of cancer Journal international du cancer. 2009;124:638–643. doi: 10.1002/ijc.23989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Zhu JH, Chen R, Yi W, Cantin GT, Fearns C, Yang Y, et al. Protein tyrosine phosphatase PTPN13 negatively regulates Her2/ErbB2 malignant signaling. Oncogene. 2008;27:2525–2531. doi: 10.1038/sj.onc.1210922. [DOI] [PubMed] [Google Scholar]
- 109.Vermeer PD, Bell M, Lee K, Vermeer DW, Wieking BG, Bilal E, et al. ErbB2, EphrinB1, Src kinase and PTPN13 signaling complex regulates MAP kinase signaling in human cancers. PloS one. 2012;7:e30447. doi: 10.1371/journal.pone.0030447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kuchay S, Duan S, Schenkein E, Peschiaroli A, Saraf A, Florens L, et al. FBXL2- and PTPL1-mediated degradation of p110-free p85beta regulatory subunit controls the PI(3)K signalling cascade. Nature cell biology. 2013;15:472–480. doi: 10.1038/ncb2731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Huang W, Bei L, Eklund EA. Fas-associated phosphatase 1 (Fap1) influences betacatenin activity in myeloid progenitor cells expressing the Bcr-abl oncogene. The Journal of biological chemistry. 2013;288:12766–12776. doi: 10.1074/jbc.M112.429696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Hoover AC, Strand GL, Nowicki PN, Anderson ME, Vermeer PD, Klingelhutz AJ, et al. Impaired PTPN13 phosphatase activity in spontaneous or HPV-induced squamous cell carcinomas potentiates oncogene signaling through the MAP kinase pathway. Oncogene. 2009;28:3960–3970. doi: 10.1038/onc.2009.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Hagemann N, Ackermann N, Christmann J, Brier S, Yu F, Erdmann KS. The serologically defined colon cancer antigen-3 interacts with the protein tyrosine phosphatase PTPN13 and is involved in the regulation of cytokinesis. Oncogene. 2013;32:4602–4613. doi: 10.1038/onc.2012.485. [DOI] [PubMed] [Google Scholar]
- 114.Abaan OD, Hendriks W, Uren A, Toretsky JA, Erkizan HV. Valosin containing protein (VCP/p97) is a novel substrate for the protein tyrosine phosphatase PTPL1. Experimental cell research. 2013;319:1–11. doi: 10.1016/j.yexcr.2012.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Spanos WC, Hoover A, Harris GF, Wu S, Strand GL, Anderson ME, et al. The PDZ binding motif of human papillomavirus type 16 E6 induces PTPN13 loss, which allows anchorage-independent growth and synergizes with ras for invasive growth. Journal of virology. 2008;82:2493–2500. doi: 10.1128/JVI.02188-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Schickel R, Park SM, Murmann AE, Peter ME. miR-200c regulates induction of apoptosis through CD95 by targeting FAP-1. Molecular cell. 2010;38:908–915. doi: 10.1016/j.molcel.2010.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Huang W, Bei L, Eklund EA. Fas-associated phosphatase 1 mediates Fas resistance in myeloid progenitor cells expressing the Bcr-abl oncogene. Leukemia & lymphoma. 2013;54:619–630. doi: 10.3109/10428194.2012.720979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Wyatt L, Khew-Goodall Y. PTP-Pez: a novel regulator of TGFbeta signaling. Cell Cycle. 2008;7:2290–2295. doi: 10.4161/cc.6443. [DOI] [PubMed] [Google Scholar]
- 119.Au AC, Hernandez PA, Lieber E, Nadroo AM, Shen YM, Kelley KA, et al. Protein tyrosine phosphatase PTPN14 is a regulator of lymphatic function and choanal development in humans. American journal of human genetics. 2010;87:436–444. doi: 10.1016/j.ajhg.2010.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wang W, Huang J, Wang X, Yuan J, Li X, Feng L, et al. PTPN14 is required for the density-dependent control of YAP1. Genes & development. 2012;26:1959–1971. doi: 10.1101/gad.192955.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Wadham C, Gamble JR, Vadas MA, Khew-Goodall Y. The protein tyrosine phosphatase Pez is a major phosphatase of adherens junctions and dephosphorylates beta-catenin. Mol Biol Cell. 2003;14:2520–2529. doi: 10.1091/mbc.E02-09-0577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zhang P, Guo A, Possemato A, Wang C, Beard L, Carlin C, et al. Identification and functional characterization of p130Cas as a substrate of protein tyrosine phosphatase nonreceptor 14. Oncogene. 2012 doi: 10.1038/onc.2012.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Michaloglou C, Lehmann W, Martin T, Delaunay C, Hueber A, Barys L, et al. The tyrosine phosphatase PTPN14 is a negative regulator of YAP activity. PloS one. 2013;8:e61916. doi: 10.1371/journal.pone.0061916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Huang JM, Nagatomo I, Suzuki E, Mizuno T, Kumagai T, Berezov A, et al. YAP modifies cancer cell sensitivity to EGFR and survivin inhibitors and is negatively regulated by the non-receptor type protein tyrosine phosphatase 14. Oncogene. 2013;32:2220–2229. doi: 10.1038/onc.2012.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Liu X, Yang N, Figel SA, Wilson KE, Morrison CD, Gelman IH, et al. PTPN14 interacts with and negatively regulates the oncogenic function of YAP. Oncogene. 2013;32:1266–1273. doi: 10.1038/onc.2012.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Flint AJ, Tiganis T, Barford D, Tonks NK. Development of "substrate-trapping" mutants to identify physiological substrates of protein tyrosine phosphatases. Proceedings of the National Academy of Sciences of the United States of America. 1997;94:1680–1685. doi: 10.1073/pnas.94.5.1680. [DOI] [PMC free article] [PubMed] [Google Scholar]