Abstract
Hemodialysis is associated with significant circulatory stress that could produce recurrent and cumulative ischemic insults to multiple organs, such as the brain. We aimed to characterize hemodialysis-induced brain injury by longitudinally studying the effects of hemodialysis on brain white matter microstructure and further examine if the use of cooled dialysate could provide protection against hemodialysis-associated brain injury. In total, 73 patients on incident hemodialysis starting within 6 months were randomized to dialyze with a dialysate temperature of either 37°C or 0.5°C below the core body temperature and followed up for 1 year. Brain white matter microstructure was studied by diffusion tensor magnetic resonance imaging at baseline and follow-up (38 patients available for paired analysis). Intradialytic hemodynamic stress was quantified using the extrema points analysis model. Patients on hemodialysis exhibited a pattern of ischemic brain injury (increased fractional anisotropy and reduced radial diffusivity). Cooled dialysate improved hemodynamic tolerability, and changes in brain white matter were associated with hemodynamic instability (higher mean arterial pressure extrema points frequencies were associated with higher fractional anisotropy [peak r=0.443, P<0.03] and lower radial diffusivity [peak r=−0.439, P<0.02]). Patients who dialyzed at 0.5°C below core body temperature exhibited complete protection against white matter changes at 1 year. Our data suggest that hemodialysis results in significant brain injury and that improvement in hemodynamic tolerability achieved by using cooled dialysate is effective at abrogating these effects. This intervention can be delivered without additional cost and is universally applicable.
Keywords: hemodialysis, cardiovascular, BP
Cognitive, psychologic, and functional abnormalities are well recognized in patients on hemodialysis (HD). Deficiencies in memory, executive function, and language are described in this population.1,2 Psychiatric disorders, such as depression, are far more prevalent in patients on HD compared with a population of the same age.3,4 The 1-year risk of developing multi-infarct dementia in patients on HD is 7.4 times higher than that of the general population.4,5 More importantly, the initiation of HD was found to be associated with a sharp decline in cognitive and functional status.6
There is now strong emerging evidence that the procedure of HD itself triggers significant recurrent circulatory stress.7 This circulatory stress is the result of interaction between complex hemodynamic factors, leading to perfusion anomalies in vulnerable vascular beds.8 Myocardial hypoperfusion and myocardial stunning manifested as regional wall motion abnormalities during HD have both been described.9,10 The effects of HD on the brain remain largely unexamined. We hypothesized that the same process occurs in other vulnerable vascular beds, such as the brain. Using a novel hemodynamic model (extrema points analysis),11 we showed that the frequencies of mean arterial BP extrema points increase during HD to peak during the third quarter of HD12 and that higher frequencies were found to be associated with neurocognitively significant established white matter (WM) damage in patients on HD.13
One of the most important interventions to improve hemodynamic performance during HD is the reduction of the dialysate temperature. Systematic review confirmed that reducing the dialysate temperature improves hemodynamic stability and reduces symptomatic intradialytic hypotension (IDH).14 This evidence was later supported by studies that showed reduction in myocardial stunning expressed as regional wall motion abnormalities and improvements in cardiovascular performance when reducing the dialysate temperature.15,16 These beneficial effects of using a lower dialysate temperature are thought to be mainly driven by improved systemic vascular resistance; one study suggested higher production of nitric oxide when using a dialysate temperature of 37.5°C compared with a cooled dialysate.17 However, the long-term effects of cooling the dialysate on vulnerable vascular beds are still unknown. Optimal temperature for the dialysate is also not known. Dialysis at 35°C was reported to have poor tolerability15; however, dialyzing at 0.5°C below core body temperature removes cold symptoms but provides a similar degree of protection against cardiac stunning.18
Diffusion tensor imaging (DTI) is a molecular magnetic resonance imaging (MRI) technique that allows the study of brain WM structural integrity. The random motion of water molecules within biologic tissues is restricted by cell membrane, cytoskeleton, and macromolecules. Therefore, it is possible to obtain information about tissue microstructure simply by observing the motion of water molecules. The tensor of water molecules diffusion can be decomposed into three orthogonal eigenvectors and three eigenvalues. The diffusion of water molecules in a highly organized tissue, such as the brain, can be represented in each voxel by anisotropy and diffusivity. Fractional anisotropy (FA) is a measure of diffusion directionality, and therefore, it represents the integrity of WM tracts. Diffusivity represents the degree of random water motion and is also sensitive to WM structural damage.19 Diffusivity along the direction of maximal diffusion is called axial diffusivity (AD), which is equal to the first eigenvalue ʎ1. Diffusion along the two orthogonal directions perpendicular to the main diffusion direction is called radial diffusivity (RD) and expressed as the average of the second and third eigenvalues [RD=(ʎ2+ʎ3)/2]. DTI has been shown to be sensitive in detecting subtle (but functionally significant) ultrastructural abnormalities in WM (in cerebral small vessel disease but also, multiple sclerosis, bipolar disorder, and schizotypal personality disorder20–23).
In this randomized clinical trial, we aimed to test the hypothesis that HD is associated with progressive WM ultrastructural injury and that it is amenable to protection by reducing HD-induced circulatory stress by cooling the dialysate.
Results
Enrolment and Follow-Up
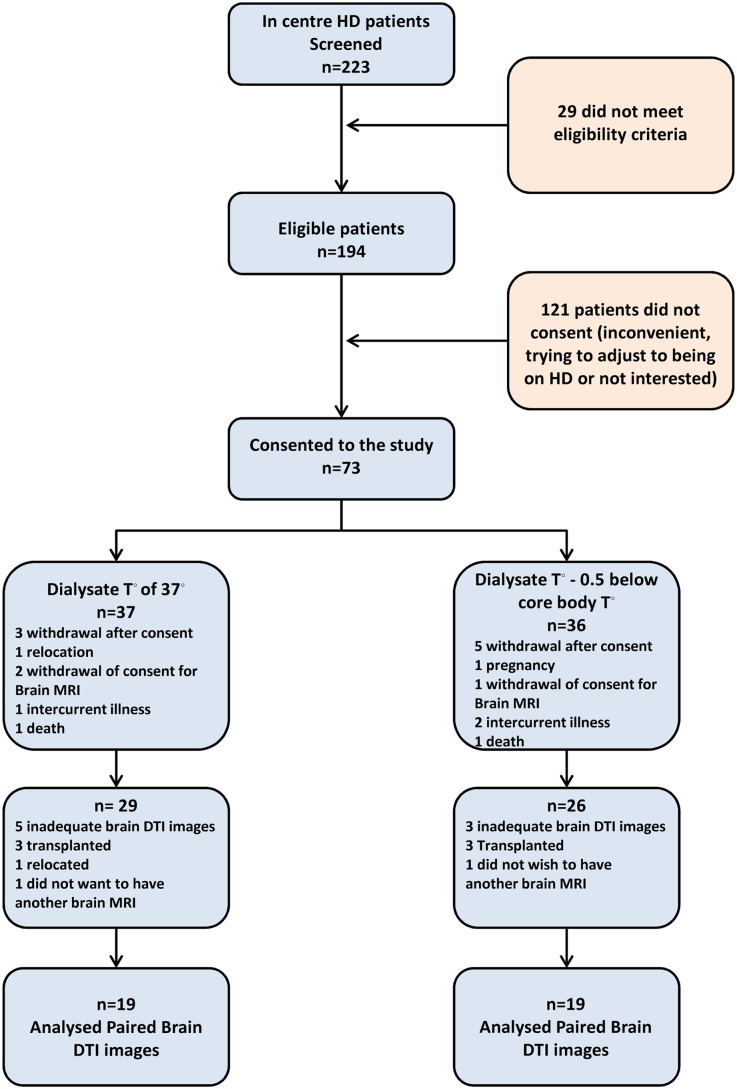
Of 223 patients on incident HD screened, 29 patients did not meet the eligibility criteria. Of 194 eligible patients, 121 patients did not consent for the study. The main reason given was inconvenience, because many patients felt that they wanted to adjust to being on HD. There were no statistically significant differences in age and sex between those who consented and those who did not (57.5±14.9 versus 61.5±22.3 years, P=0.26) and women (35.1% versus 41.3%, P=0.59). The remaining 73 patients entered the study and were randomized accordingly. At the end of the study, there were 38 patients who completed the brain part of the trial and had paired DTI images at baseline and 12 months. Of 73 patients who consented, 8 patients withdrew from the trial after consenting, 2 patients relocated to difference regions, 1 patient became pregnant, 3 patients withdrew their consent to have MRI at baseline, 3 patients had intercurrent illness that prevented imaging, and 2 patients had unexpected deaths. During the follow-up period, eight patients had inadequate brain DTI images, six patients received transplants, and two patients did not want to have a second brain MRI, which was in the trial flow chart (Figure 1). The characteristics of the trial cohort are summarized in Table 1, which shows that both groups were well matched. There were no differences in the characteristics of those who completed the study and those who dropped out, which is shown in Supplemental Table 1. Finally, we compared the FA, RD, and AD of brain WM between the two randomized groups at baseline using tract-based spatial statistics (TBSS) and found no differences between the two groups.
Figure 1.
Trial flow chart. Consolidated Standards of Reporting Trials (CONSORT) flow diagram demonstrating the phases of the trial starting from screening through to enrolment, randomization, follow up and data analysis.
Table 1.
Characteristics of the trial cohort
| Characteristics | Group Dialyzed at 37°C (n=19) | Group Dialyzed at 0.5°C below Body Temperature (n=19) | P Value |
|---|---|---|---|
| Age, yr | 61.37±12.31 | 54±16.46 | 0.14 |
| Sex (women) | 31.6% (6) | 36.8% (7) | >0.99 |
| Body mass index (kg/m2) | 28.6±5.6 | 26.7±5.3 | 0.32 |
| Diabetes mellitus | 26.3% (5) | 15.8% (3) | 0.35 |
| Ischemic heart disease | 31.6% (6) | 15.8% (3) | 0.45 |
| History of stroke | 5.3% (1) | 5.3% (1) | >0.99 |
| Smoking | 31.6% (6) | 21.1% (4) | 0.36 |
| Systolic BP (mmHg) | 136.8±25.12 | 143.12±24.5 | 0.49 |
| Diastolic BP (mmHg) | 71±10.87 | 79.6±12.6 | 0.05 |
| Ultrafiltration volume (ml) | 2067.53±579.34 | 2075.08±853.15 | 0.98 |
| Dialysis access line | 26.3% (5) | 26.3%(5) | |
| Dialysis access fistula/graft | 73.7% (14) | 73.7% (14) | |
| Hemoglobin | 11.29±1.86 | 10.63±1.35 | 0.31 |
| Calcium | 2.31±0.13 | 2.34±0.19 | 0.63 |
| Phosphate | 1.67±0.60 | 1.50±0.33 | 0.38 |
| Albumin | 34.86±3.34 | 36.08±3.84 | 0.40 |
| Erythropoietin-stimulating agent | 68.4% (13) | 63.2% (12) | 0.81 |
| Renin-angiotensin system blockade | 15.8% (3) | 10.5% (2) | >0.99 |
| β-Blockers | 26.3% (5) | 31.6% (6) | 0.71 |
| Statins | 47.4% (9) | 36.8% (7) | 0.72 |
| Vitamin D analogs | 42.1% (8) | 42.1% (8) | >0.99 |
| Kt/V | 1.20 (0.99–1.30) | 1.28 (1.14–1.38) | 0.17 |
Normally distributed data are presented as means±SDs. Non-normally distributed data are presented as medians (interquartile ranges). Categorical data are presented as percentages (numbers).
The Longitudinal Effect of HD on Brain WM Microstructure
The effect of HD on brain WM microstructure was studied by comparing all brain images paired at baseline and follow-up. Age, sex, and presence of ischemic heart disease and diabetes mellitus were incorporated into the design matrix to account for these factors. Aggregating both groups, we found an increase in FA at follow-up compared with baseline images, which is shown in Figure 2 (P<0.05 corrected for family-wise error [FWE]). Mean FA of the highlighted statistically significant voxels increased from 0.398±0.036 at baseline to 0.413±0.042 at 12 months. However, RD decreased at follow-up compared with baseline (P<0.05 corrected for FWE) (Figure 2). Mean RD of the highlighted statistically significant voxels decreased from 0.00063±0.0000692 10−3mm2⋅s−1) at baseline to 0.00061±0.000073 10−3mm2⋅s−1 at 12 months. There was no change in AD between baseline and follow-up. Changes in regional FA and the statistically significant voxels with both groups aggregated over 1 year are shown in Supplemental Table 2.
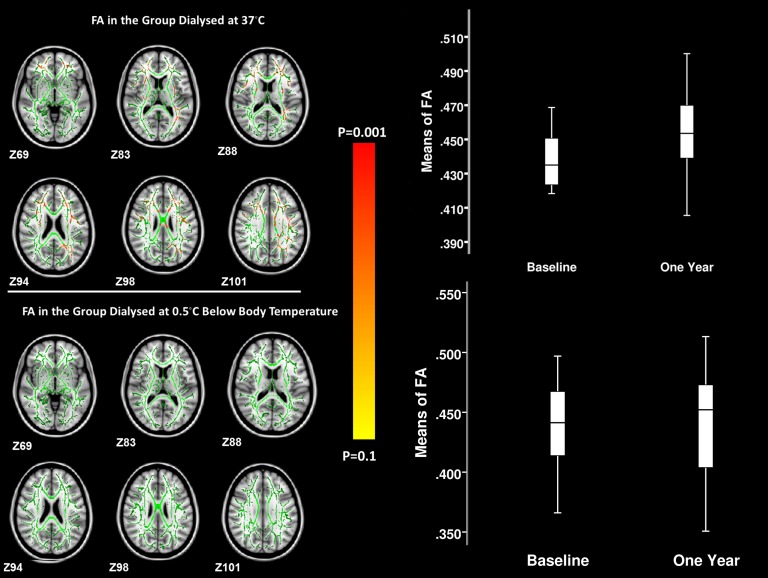
Figure 2.
Statistical image representing the results of the tract-based spatial statistical test comparing FA with RD at baseline and 1 year by aggregating the control and intervention groups. The statistically significant voxels with P values<0.05 corrected for multiple comparisons (red-yellow) are presented on a mean skeleton (green) on standardized T1 axial brain slices (of z scores). The color bar represents the degree of significance. The box plots represent FA and RD values in the statistically significant voxels at baseline and 1 year with the two groups aggregated.
The Effects of Cooling the Dialysate on Brain WM Microstructure
In the group that dialyzed with a dialysate temperature of 0.5°C below their core body temperature, there were no statistically significant changes in FA, RD, or AD between baseline and 12 months (mean FA at baseline=0.271±0.023; mean FWE at 1 year=0.269±0.031, P>0.05 corrected for FWE). However, the group that dialyzed at 37°C had increased FA at 12 months compared with baseline (P<0.05 corrected for FWE), which is shown in the statistical image (Figure 3). In this group, mean FA of the highlighted statistically significant voxels increased from 0.432±0.0298 at baseline to 0.452±0.0318 at 12 months. Moreover, using the John Hopkins University atlas for WM tracts, we found statistically significant voxels in 18 of 20 regions represented by this atlas; the FA means of the statistically significant voxels in each region and their percentages are presented in Table 2.
Figure 3.
Statistical image representing the results of the voxel-wise statistical model for the change in FA in each group over 1 year. The statistically significant voxels with P values<0.05 corrected for multiple comparisons (red-yellow) are overlaid on a mean skeleton (green) on standardized T1 axial brain slices (of z scores). The color bar represents the degree of significance. The box plots represent FA values of the statistically significant voxels in the group that dialyzed at 37°C at baseline and 1 year. No statistically significant voxels were found in the group that dialyzed at 0.5°C below their body temperature. In this group, FA values of the voxels with the same location as the significant ones in the control group are represented by the box plots at the bottom.
Table 2.
Region-of-interest analysis of FA
| Regional WM Tracts According to John Hopkins University Atlas | Group Dialyzed at 0.5°C below Body Temperature (n=19) | Group Dialyzed at 37°C (n=19) | ||||
|---|---|---|---|---|---|---|
| Mean FA at Baseline | Mean FA at 1 yr | Significant Voxels (%) | Mean FA at Baseline | Mean FA at 1 yr | Significant Voxels (%) | |
| Anterior thalamic radiation-L | 0.336±0.032 | 0.344±0.043 | 0 | 0.335±0.029 | 0.345±0.029 | 11.1 |
| Anterior thalamic radiation-R | 0.334±0.032 | 0.331±0.043 | 0 | 0.334±0.029 | 0.343±0.030 | 10.2 |
| Corticospinal tract-L | 0.428±0.022 | 0.428±0.033 | 0 | 0.432±0.024 | 0.439±0.022 | 4.4 |
| Corticospinal tract-R | 0.418±0.022 | 0.416±0.031 | 0 | 0.417±0.023 | 0.428±0.018 | 3.8 |
| Cingulate gyrus-L | 0.302±0.022 | 0.301±0.035 | 0 | 0.306±0.025 | 0.314±0.023 | 24.3 |
| Cingulate gyrus-R | 0.299±0.023 | 0.297±0.034 | 0 | 0.305±0.024 | 0.312±0.022 | 1.8 |
| Hippocamups-L | 0.265±0.035 | 0.263±0.038 | 0 | 0.261±0.033 | 0.275±0.032 | 1.8 |
| Hippocamups-R | 0.280±0.037 | 0.279±0.043 | 0 | 0.280±0.033 | 0.292±0.033 | 0 |
| Forceps major | 0.338±0.026 | 0.335±0.036 | 0 | 0.337±0.025 | 0.344±0.022 | 3.9 |
| Forceps minor | 0.316±0.027 | 0.316±0.037 | 0 | 0.315±0.030 | 0.324±0.030 | 25 |
| Inferior fronto-ocipital fasciculus-L | 0.314±0.028 | 0.314±0.038 | 0 | 0.310±0.025 | 0.320±0.024 | 9.5 |
| Inferior fronto-ocipital fasciculus-R | 0.320±0.027 | 0.319±0.038 | 0 | 0.321±0.025 | 0.328±0.024 | 9.7 |
| Inferior longitudinal fasciculus-L | 0.298±0.025 | 0.297±0.032 | 0 | 0.298±0.020 | 0.306±0.021 | 13.2 |
| Inferior longitudinal fasciculus-R | 0.289±0.021 | 0.287±0.031 | 0 | 0.292±0.020 | 0.299±0.020 | 0 |
| Superior longitudinal fasciculus-L | 0.286±0.022 | 0.284±0.031 | 0 | 0.288±0.018 | 0.297±0.018 | 26.6 |
| Superior longitudinal fasciculus-R | 0.272±0.019 | 0.270±0.027 | 0 | 0.273±0.017 | 0.282±0.013 | 6.9 |
| Ucinate fasciculus-L | 0.306±0.029 | 0.307±0.040 | 0 | 0.301±0.025 | 0.309±0.026 | 3.2 |
| Ucinate fasciculus-R | 0.303±0.026 | 0.305±0.039 | 0 | 0.305±0.025 | 0.314±0.027 | 5.1 |
| Superior longitudinal fasciculus-L (temporal part) | 0.314±0.031 | 0.312±0.037 | 0 | 0.318±0.022 | 0.321±0.024 | 21.6 |
| Superior longitudinal fasciculus-R (temporal part) | 0.357±0.028 | 0.354±0.037 | 0 | 0.350±0.024 | 0.354±0.021 | 0.9 |
Region-of-interest analysis using John Hopkins University WM labels atlas showing the changes in means of FA at baseline and 1 year of each region stratified by treatment group; percentages of the statistically significant voxels in each region are also presented. L, left; R, right.
A voxel-wise analysis using a general linear model (GLM) approach was used to compare the two groups at baseline and 1 year. At baseline, there was no difference in FA between the two groups (mean FA=0.273±0.022 in the control group versus 0.271±0.023 in the intervention group, P>0.05 corrected for FWE). However, at 1 year, mean FA was higher in the control group that dialyzed at 37°C compared with the group that dialyzed at 0.5°C below their body temperature (mean FA=0.282±0.021 versus 0.269±0.031, respectively, P<0.05 corrected for FWE). In the statistically significant voxels between the two groups at 1 year, the control group had a mean FA of 0.474±0.030 compared with 0.449±0.040 in the intervention group (P<0.05 corrected for FEW), which is shown in Supplemental Figure 1.
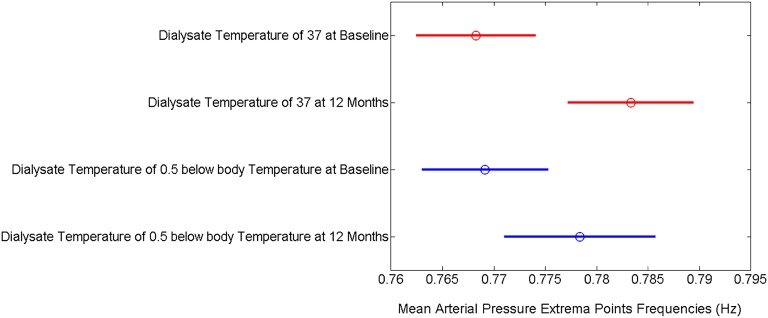
Hemodynamic Performance and Brain WM Integrity
Repeated measures ANOVA showed that the group that dialyzed at 37°C had a significant increase in mean arterial pressure (MAP) extrema points frequencies at 1 year, whereas the intervention group did not [F(3,89984)=4.72, P=0.003] (Figure 4). Furthermore, in a voxel-based analysis, the correlation between MAP extrema points frequency during HD on one hand and FA and RD on the other hand was examined using TBSS. Higher MAP extrema points frequencies were associated with higher FA (peak r=0.443, P<0.03) and lower RD (peak r=−0.439, P<0.02). The voxels with statistically significant correlations are presented in Supplemental Figure 2. The number of IDH episodes did not correlate with any changes in FA, RD, or AD.
Figure 4.
A graphical representation of repeated measures ANOVA of the frequencies of the mean arterial BP extrema points across all groups at baseline and follow-up. The circles represent the means of the frequencies of the extrema points for mean arterial BP. The lines represent confidence intervals.
Discussion
Few previous studies examined brain WM microstructure in patients on HD using DTI compared with normal controls.24,25 These studies reported decreased FA and increased mean diffusivity and RD in patients on HD compared with age-matched controls, indicating established WM damage. However, the lack of a longitudinal design in these studies does not allow any causality inference linking HD as a process to WM damage. Furthermore, these studies did not have any hemodynamic measurements to examine the mechanisms involved. This study is the first with an appropriate design to longitudinally examine the specific effects of HD on brain WM integrity and the capacity to reduce injury with a dialysis-based intervention by reducing circulatory stress.
The temporal evolution of diffusion of water molecules in ischemic stroke is well described in experimental animal models and humans. In the acute and subacute phases of brain ischemia, diffusivity of water molecules decreases, whereas diffusion anisotropy has been described in many studies to increase. In experimental animal stroke models, a decrease in diffusivity measures (mean diffusivity, RD, and AD) has been described in the hyperacute and acute phases, with an increase in FA in the first few hours after inducing an ischemic stroke.26,27 In humans, a similar pattern of increased FA has been described in the first 7 hours after an ischemic stroke, which starts to reduce within 21–29 hours.28,29 Similar to the findings in animal models, reductions in all diffusion eigenvalues have been described in humans during the acute phase of an ischemic stroke.28–31 These changes are thought to be related to the cytotoxic edema that results from ischemia.
We found similar WM changes to the ones described above comparing scans from all patients at baseline with their scans at 12 months. In our study, FA increased, whereas RD decreased, and there was no change in AD. These changes seem to correlate with a higher frequency of change in peaks and troughs of MAP (extrema points). We have previously shown that, in patients on HD, higher MAP extrema points frequencies (indicative of greater hemodynamic instability) correlated with established brain WM damage.13 The degree of brain injury was directly correlated to the degree of reduction in both neurocognitive testing scores. We also showed that, during HD, MAP extrema points frequencies increase gradually to peak during the third quarter of the dialysis session and remain at that level in the fourth quarter12 (previous studies identify this finding as the period of peak hemodynamic stress). The pattern that we found in this study of increased FA and reduced RD is rather unexpected, because these changes have been described in acute ischemic stroke within <24 hours. The MRI imaging at baseline and follow-up was performed on a nondialysis day within <24 hours from the dialysis session, and therefore, it is plausible that our findings—indicating acute ischemia—are related to the previous dialysis session, which then was exacerbated over 1 year of HD treatment. This finding supports the hypothesis that patients on HD are susceptible to recurrent acute ischemic brain insults that result from HD-induced circulatory stress, which is analogous to that observed previously in the myocardium.9,10 Furthermore, it is also plausible that higher extrema points frequencies are implicated in end organ damage, possibly by inducing acute injury at first that then develops into established damage.
In the group that dialyzed at 0.5°C below their core body temperature, there were no changes in brain WM FA, AD, or RD, and the MAP extrema points frequencies for this group did not significantly change at 12 months. The opposite was observed in the group that dialyzed at 37°C, where FA and MAP extrema points frequencies increased significantly at 1 year. Reducing the dialysate temperature is a very simple intervention with no cost that seems to have a significant effect on hemodynamic stability, organ perfusion, and end organ damage in this population, which is burdened with impaired hemodynamic regulatory functions. The hemodynamic stress of HD seems to induce changes in brain WM consistent with acute ischemia. HD at an individualized temperature of 0.5°C below core body temperature leads to better hemodynamic stability during HD and preservation of WM microstructure.
Our study has limitations. The sample size is small, which is a result of difficulties in recruiting patients on incident HD. Starting dialysis is a critical period in this population as they try to adjust to this major change, which was the reason that restricted many patients from participating in the study. The study has a high dropout percentage of 47.9%. This result was not related to the intervention, because it was tolerated very well; reasons for this dropout are summarized in Figure 1. The small sample size and the high dropout rate might limit the generalizability of the trial.
This patient group seems to be resistant to the application of interventions derived from the study of the non-CKD population designed to target improved cardiovascular outcomes. This study provides the first evidence that application of dialysis-based intervention improves HD tolerability (derived from an emerging understanding of the interaction of HD treatment in the pathophysiology of accelerated end organ injury) and directly abrogates critical organ injury. This study justifies additional larger-scale testing of dialysis-based interventions to reduce the burden of morbidity and mortality in HD.
Concise Methods
Study Design
The study was a randomized clinical trial, where patients were randomized to dialyze with a dialysate temperature of either 37°C or 0.5°C below the core body temperature determined from the mean of six prior treatment sessions with a tympanic thermometer. The follow-up period of the trial was 12 months. The study involved four dialysis centers, and ethical approval for the trial was obtained from the Nottingham Ethics Committee for all participating centers before study initiation and patient enrolment. The study was performed in accordance with the Research Governance Framework, International Conference on Harmonization Good Clinical Practice Guideline, and the 2000 Scotland Revision of the Declaration of Helsinki. The protocol of the study has been previously published in full.32
Participants
Recruitment for the trial commenced in September of 2009; the study completed recruiting 73 patients on dialysis in January of 2012, and the follow-up of the last patient was completed in January of 2013. Inclusion criteria for the trial were (1) patients having HD treatment at least three times per week, (2) patients willing and able to provide consent, and (3) men and women age≥16 years old. Exclusion criteria were (1) exposure to HD for >180 days, (2) contraindications for using MRI (e.g., patients with pacemakers and metal implants), (3) inability to tolerate MRI because of claustrophobia, (4) New York Heart Association grade IV heart failure, (5) pregnancy or lactating, and (6) mental incapacity to consent. All participants provided written informed consent before any trial-related procedure occurred. Adverse effects and safety of the intervention were monitored during the trial. The intervention was very well tolerated by the participants, and there were no adverse events related to the intervention.
Randomization and Blinding
Randomization was done in a single block by sealed envelopes generated by an independent statistician. The study was unblinded as appropriate; the dialysate temperature needed to be iteratively entered by the dialysis machine operator, and images were analyzed, anonymized, and blinded to treatment allocation.
Sample Size Estimation
To our knowledge, there have not been any trials that used DTI in patients on HD and analyzed the data using threshold-free cluster enhancement. Although such data are not available to enable an estimation of the treatment effect, this vanguard trial will provide an estimate from which to decide if future studies are warranted.
Hemodynamic Assessment during HD
Noninvasive continuous beat-to-beat hemodynamic monitoring was performed during HD using the Finometer (Finapres Medical Systems, Arnhem, The Netherlands). The Finometer works by continuous pulse-wave analysis at the digital artery and uses the finger-clamp method, in which changes in digital arterial diameter are detected by means of an infrared photoplethysmograph33 and opposed by an ultrafast pressure servo controller that changes pressure in an inflatable air bladder, both of which are mounted in a finger cuff. Arterial waveforms are generated and measured on a beat-to-beat basis and used to reconstruct a central aortic waveform by a validated transfer function.34
Extrema Points Analysis Model
We used a novel mathematical treatment of beat-to-beat hemodynamic parameters obtained by continuous monitoring during HD. We have previously described this model in detail.11 In brief, BPs generated by each heart beat constantly vary between local peaks and troughs (local extrema), the frequency and amplitude of which are regulated to maintain optimal organ perfusion. We have shown that patients on HD display higher MAP extrema frequencies, potentially resulting in higher variation in organ perfusion and detrimentally challenging perfusion to vulnerable vascular beds. Using Matlab and Simulink (R2011a; MathWorks, Natik, MA), the frequency of MAP extrema points was computed for each subject on HD and used in image statistical analysis using GLM.
IDH
IDH was defined as a reduction of 10% in systolic BP from the predialysis level. Using a Matlab (R2011a; MathWorks) script, systolic BP data obtained from the finometer were averaged every 5 minutes and compared with the predialysis level. A drop of 10% was identified as an IDH episode, and the number of IDH episodes during HD was computed.
Brain DTI
DTI imaging was performed on a nondialysis day on enrolment and then repeated 1 year later. Imaging was performed in a 1.5T MRI scanner (GE SignaHDxt 1.5T; GE Healthcare, Milwaukee, WI). A standard quadrature head coil was used. DTI sequences used a single-shot echoplanar imaging in 12 diffusion-sensitized directions, each with a b factor of 1,000 s mm\−2, field of view of 24 cm, two interleaved series of four repeats, each containing 25 2.8-mm slices with no gap, and repetition time/echo time of 12,000/80 with matrix=96×96.
Image Processing and Image Statistical Analyses
All images were analyzed using FSL5 software package, a comprehensive library of tools for the analysis of MRI and DTI brain imaging data created by Analysis Group (Oxford, United Kingdom; http://fsl.fmrib.ox.ac.uk/fsl).
All images were realigned to remove eddy current distortions.35,36 Diffusion tensor elements were computed at each voxel using the FMRIB Diffusion Toolbox program by creating a brain mask using Brain Extraction Tool software37 and then fitting the diffusion tensor model to obtain FA, AD, and RD maps.38
TBSS
Voxel-wise statistical analysis was performed using TBSS. Nonlinear registration aligning all FA data to a 1×1×1-mm standard space image (FMRIB58_FA image) was performed. The mean FA image was then created and thinned to create a mean FA skeleton, which represents the centers of all tracts common to the cohort. Each subject's aligned FA data were then projected onto this skeleton.
Image Voxel-Wise Statistical Analyses
Image voxel-wise statistical analysis randomize software was used to perform voxel-based statistical analysis of the skeletonized data. Paired t test was used to compare baseline and follow-up images. The effect of the intervention was examined using a repeated measures ANOVA model, and the model was constructed with images of each individual at baseline paired with those at 12 months according to group allocation. Because age, sex, and presence of diabetes mellitus and ischemic heart disease are important predictors of WM structural integrity, they were included in the design matrix and defined in the design contrast as covariates to correct for variation related to these factors. Time between the MRI scans at baseline and follow-up was also included as a covariate in the model. The number of permutations for all statistical analyses was set at 10,000, and correction for multiple comparisons was achieved using threshold-free cluster enhancement. Voxels were deemed significant at P<0.05, and all reported P values in the paired t test and ANOVA model were corrected for FWE.
A GLM was used to assess the difference between the two groups at 1 year. The model included age, sex, presence of ischemic heart disease and diabetes mellitus, and time elapsed between the baseline and follow-up MRI scans as covariates. GLM was also used to examine the correlation between brain WM FA, RD, and AD on one hand and the frequency of MAP extrema points during HD and the number of IDH episodes on the other hand. Baseline and 1-year follow-up images were paired in the design matrix. The design contrast was set to examine both positive and negative correlations. Peak correlation coefficient (peak r) was calculated from the t-map using the fslmaths program.
WM tracts were divided into 20 areas according to the John Hopkins University WM labels atlas by creating masks for each area. All averages and SDs were extracted from images using fslmaths and fslstats programs.
Statistical analysis was performed using SPSS, version 19 (IBM SPSS Statistics, Inc.). An α-error at 0.05 was judged to be significant. Normality was assessed using the Kolmogorov–Smirnov test, histograms, and normal Q-Q plot. Normally distributed data were presented as means±SDs; non-normally distributed data were presented as medians (interquartile ranges). Categorical data were expressed as counts and percentages. Unadjusted data were analyzed using independent sample t tests for normally distributed variables, Mann–Whitney U tests for nonparametric variables, and chi-squared or Fisher exact tests for categorical variables. Repeated measures ANOVA was used to compare MAP extrema points frequencies during HD across all subjects at baseline and follow-up. This comparison was done in Matlab (R2011a; MathWorks) using the N-way ANOVA and the multiple comparison test functions.
Disclosures
None.
Supplementary Material
Acknowledgments
The authors acknowledge Prof. Hugh Markus for input into the image acquisition protocol. The authors thank Prof. Simon Davies, Dr. Indranil Dasgupta, and Dr. Veena Reddy from the participating dialysis centers. The authors also acknowledge the radiographers from the Nuffield Hospital in Derby and Sheffield Teaching Hospital.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2013101086/-/DCSupplemental.
References
- 1.Oaksford K, Oaksford M, Ashraf M, Fitzgibbon G: Comparing neuropsychological function before and during haemodialysis: A habituating selective deficit for prose recall. Br J Health Psychol 13: 273–289, 2008 [DOI] [PubMed] [Google Scholar]
- 2.Murray AM, Tupper DE, Knopman DS, Gilbertson DT, Pederson SL, Li S, Smith GE, Hochhalter AK, Collins AJ, Kane RL: Cognitive impairment in hemodialysis patients is common. Neurology 67: 216–223, 2006 [DOI] [PubMed] [Google Scholar]
- 3.Fukunishi I, Koyama K, Iyoda S, Ogawa H, Ota Y, Nagaya K, Okayama M, Ushizaki R, Fujita E, Ezaki M, Nishitani S, Miyashita Y: Depressive symptoms in hemodialysis patients with silent cerebral infarction. Psychosomatics 44: 352–353, 2003 [DOI] [PubMed] [Google Scholar]
- 4.Fukunishi I, Kitaoka T, Shirai T, Kino K, Kanematsu E, Sato Y: Psychiatric disorders among patients undergoing hemodialysis therapy. Nephron 91: 344–347, 2002 [DOI] [PubMed] [Google Scholar]
- 5.Fazekas G, Fazekas F, Schmidt R, Kapeller P, Offenbacher H, Krejs GJ: Brain MRI findings and cognitive impairment in patients undergoing chronic hemodialysis treatment. J Neurol Sci 134: 83–88, 1995 [DOI] [PubMed] [Google Scholar]
- 6.Kurella Tamura M, Covinsky KE, Chertow GM, Yaffe K, Landefeld CS, McCulloch CE: Functional status of elderly adults before and after initiation of dialysis. N Engl J Med 361: 1539–1547, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McIntyre CW: Recurrent circulatory stress: The dark side of dialysis. Semin Dial 23: 449–451, 2010 [DOI] [PubMed] [Google Scholar]
- 8.McIntyre CW: Haemodialysis-induced myocardial stunning in chronic kidney disease - a new aspect of cardiovascular disease. Blood Purif 29: 105–110, 2010 [DOI] [PubMed] [Google Scholar]
- 9.McIntyre CW, Burton JO, Selby NM, Leccisotti L, Korsheed S, Baker CS, Camici PG: Hemodialysis-induced cardiac dysfunction is associated with an acute reduction in global and segmental myocardial blood flow. Clin J Am Soc Nephrol 3: 19–26, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burton JO, Jefferies HJ, Selby NM, McIntyre CW: Hemodialysis-induced cardiac injury: Determinants and associated outcomes. Clin J Am Soc Nephrol 4: 914–920, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eldehni MT, Odudu A, McIntyre CW: Exploring haemodynamics of haemodialysis using extrema points analysis model. Theor Biol Med Model 10: 33, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eldehni MT, Odudu A, McIntyre CW: Characterising hemodynamic stress during hemodialysis using extrema points analysis model. Nephron Clin Pract 2013, in press [DOI] [PubMed] [Google Scholar]
- 13.Eldehni MT, Odudu A, McIntyre CW: Brain white matter microstructure using diffusion tensor imaging and cognitive impairment in haemodialysis patients [Abstract]. Nephrol Dial Transplant 28: i49, 2013 [Google Scholar]
- 14.Selby NM, McIntyre CW: A systematic review of the clinical effects of reducing dialysate fluid temperature. Nephrol Dial Transplant 21: 1883–1898, 2006 [DOI] [PubMed] [Google Scholar]
- 15.Selby NM, Burton JO, Chesterton LJ, McIntyre CW: Dialysis-induced regional left ventricular dysfunction is ameliorated by cooling the dialysate. Clin J Am Soc Nephrol 1: 1216–1225, 2006 [DOI] [PubMed] [Google Scholar]
- 16.Chesterton LJ, Selby NM, Burton JO, McIntyre CW: Cool dialysate reduces asymptomatic intradialytic hypotension and increases baroreflex variability. Hemodial Int 13: 189–196, 2009 [DOI] [PubMed] [Google Scholar]
- 17.Beerenhout CH, Noris M, Kooman JP, Porrati F, Binda E, Morigi M, Bekers O, van der Sande FM, Todeschini M, Macconi D, Leunissen KM, Remuzzi G: Nitric oxide synthetic capacity in relation to dialysate temperature. Blood Purif 22: 203–209, 2004 [DOI] [PubMed] [Google Scholar]
- 18.Jefferies HJ, Burton JO, McIntyre CW: Individualised dialysate temperature improves intradialytic haemodynamics and abrogates haemodialysis-induced myocardial stunning, without compromising tolerability. Blood Purif 32: 63–68, 2011 [DOI] [PubMed] [Google Scholar]
- 19.Patel B, Markus HS: Magnetic resonance imaging in cerebral small vessel disease and its use as a surrogate disease marker. Int J Stroke 6: 47–59, 2011 [DOI] [PubMed] [Google Scholar]
- 20.Nitkunan A, Barrick TR, Charlton RA, Clark CA, Markus HS: Multimodal MRI in cerebral small vessel disease: Its relationship with cognition and sensitivity to change over time. Stroke 39: 1999–2005, 2008 [DOI] [PubMed] [Google Scholar]
- 21.Klawiter EC, Schmidt RE, Trinkaus K, Liang HF, Budde MD, Naismith RT, Song SK, Cross AH, Benzinger TL: Radial diffusivity predicts demyelination in ex vivo multiple sclerosis spinal cords. Neuroimage 55: 1454–1460, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lin F, Weng S, Xie B, Wu G, Lei H: Abnormal frontal cortex white matter connections in bipolar disorder: A DTI tractography study. J Affect Disord 131: 299–306, 2011 [DOI] [PubMed] [Google Scholar]
- 23.Hazlett EA, Goldstein KE, Tajima-Pozo K, Speidel ER, Zelmanova Y, Entis JJ, Silverman JM, New AS, Koenigsberg HW, Haznedar MM, Byne W, Siever LJ: Cingulate and temporal lobe fractional anisotropy in schizotypal personality disorder. Neuroimage 55: 900–908, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hsieh TJ, Chang JM, Chuang HY, Ko CH, Hsieh ML, Liu GC, Hsu JS: End-stage renal disease: In vivo diffusion-tensor imaging of silent white matter damage. Radiology 252: 518–525, 2009 [DOI] [PubMed] [Google Scholar]
- 25.Chou MC, Hsieh TJ, Lin YL, Hsieh YT, Li WZ, Chang JM, Ko CH, Kao EF, Jaw TS, Liu GC: Widespread white matter alterations in patients with end-stage renal disease: A voxelwise diffusion tensor imaging study. AJNR Am J Neuroradiol 34: 1945–1951, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pitkonen M, Abo-Ramadan U, Marinkovic I, Pedrono E, Hasan KM, Strbian D, Durukan A, Tatlisumak T: Long-term evolution of diffusion tensor indices after temporary experimental ischemic stroke in rats. Brain Res 1445: 103–110, 2012 [DOI] [PubMed] [Google Scholar]
- 27.Hui ES, Du F, Huang S, Shen Q, Duong TQ: Spatiotemporal dynamics of diffusional kurtosis, mean diffusivity and perfusion changes in experimental stroke. Brain Res 1451: 100–109, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bhagat YA, Hussain MS, Stobbe RW, Butcher KS, Emery DJ, Shuaib A, Siddiqui MM, Maheshwari P, Al-Hussain F, Beaulieu C: Elevations of diffusion anisotropy are associated with hyper-acute stroke: A serial imaging study. Magn Reson Imaging 26: 683–693, 2008 [DOI] [PubMed] [Google Scholar]
- 29.Bhagat YA, Emery DJ, Shuaib A, Sher F, Rizvi NH, Akhtar N, Clare TL, Leatherdale T, Beaulieu C: The relationship between diffusion anisotropy and time of onset after stroke. J Cereb Blood Flow Metab 26: 1442–1450, 2006 [DOI] [PubMed] [Google Scholar]
- 30.Warach S, Gaa J, Siewert B, Wielopolski P, Edelman RR: Acute human stroke studied by whole brain echo planar diffusion-weighted magnetic resonance imaging. Ann Neurol 37: 231–241, 1995 [DOI] [PubMed] [Google Scholar]
- 31.Yang Q, Tress BM, Barber PA, Desmond PM, Darby DG, Gerraty RP, Li T, Davis SM: Serial study of apparent diffusion coefficient and anisotropy in patients with acute stroke. Stroke 30: 2382–2390, 1999 [DOI] [PubMed] [Google Scholar]
- 32.Odudu A, Eldehni MT, Fakis A, McIntyre CW: Rationale and design of a multi-centre randomised controlled trial of individualised cooled dialysate to prevent left ventricular systolic dysfunction in haemodialysis patients. BMC Nephrol 13: 45, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dorlas JC, Nijboer JA, Butijn WT, van der Hoeven GM, Settels JJ, Wesseling KH: Effects of peripheral vasoconstriction on the blood pressure in the finger, measured continuously by a new noninvasive method (the Finapres). Anesthesiology 62: 342–345, 1985 [DOI] [PubMed] [Google Scholar]
- 34.Wesseling KH, Jansen JR, Settels JJ, Schreuder JJ: Computation of aortic flow from pressure in humans using a nonlinear, three-element model. J Appl Physiol (1985) 74: 2566–2573, 1993 [DOI] [PubMed] [Google Scholar]
- 35.Woods RP, Grafton ST, Holmes CJ, Cherry SR, Mazziotta JC: Automated image registration: I. General methods and intrasubject, intramodality validation. J Comput Assist Tomogr 22: 139–152, 1998 [DOI] [PubMed] [Google Scholar]
- 36.Woods RP, Grafton ST, Watson JD, Sicotte NL, Mazziotta JC: Automated image registration: II. Intersubject validation of linear and nonlinear models. J Comput Assist Tomogr 22: 153–165, 1998 [DOI] [PubMed] [Google Scholar]
- 37.Smith SM: Fast robust automated brain extraction. Hum Brain Mapp 17: 143–155, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pierpaoli C, Basser PJ: Toward a quantitative assessment of diffusion anisotropy. Magn Reson Med 36: 893–906, 1996 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.