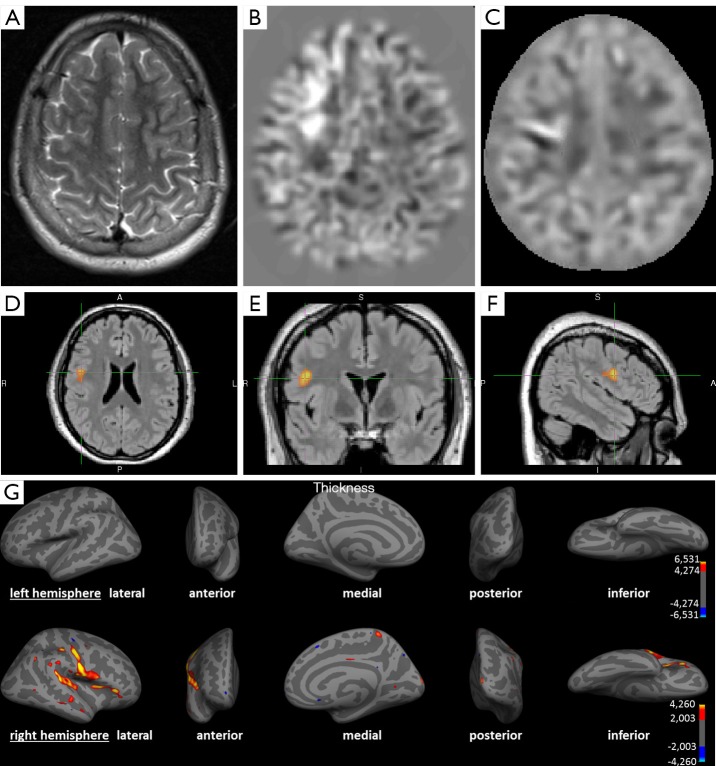
Figure 2.
A 14-year-old child with partial (clonuses of the left hand and leg) and secondary generalized seizures since the age of 4. (A) Axial T2-weighted image; (B) axial calculated junction map (window setting −4 to +4 z-score) based on a T1 MPRAGE sequence; (C) axial calculated extension map (window setting −7 to +7 z-score) based on a T1 MPRAGE sequence; (D-F) voxel-based morphometry of FLAIR, using SPM in axial, coronal and sagittal view; (G) SBM using Freesurfer representing left (upper row) and right (lower row) hemisphere. (A) No detectable structural lesion in conventional visual analysis; (B) brighter clusters in the junction map indicating blurring of the grey-white matter junction e.g., due to a focal cortical dysplasia; (C) brighter clusters in the extension map indicating abnormal extension of grey matter into white matter e.g., abnormal gyration; (D-F) colored clusters represent regions with significantly increased FLAIR intensities (P<0.05 FWE corrected); (G) colored vertices show significant increased cortical thickness (P<0.05 FDR corrected) compatible to an MCD. All post-processing methods indicate converging the presence of a lesion in the right frontal and insular cortex. The findings in post-processing methods were congruent with EEG findings. Based on these results the patient was operated, histopathology showed a focal cortical dysplasia type IIa. The patient benefited from the operation in form of a reduction of seizure frequency and intensity. SPM, statistical parametric mapping; SBM, surface-based morphometry; FWE, family wise error correction; FDR, false discovery rate correction; MCD, malformations of cortical development.