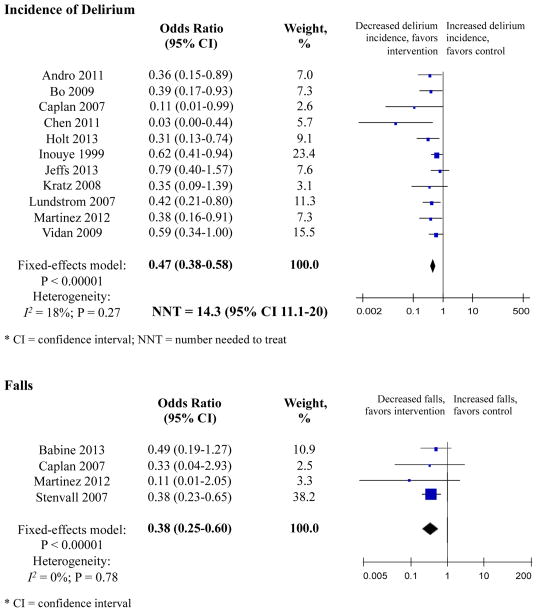
Figure 2. Primary Outcomes.
Incidence of Delirium
Eleven studies measured incidence of delirium. Three RMTs and five non-RMTs demonstrated significant reductions in the incidence of delirium. Overall, the meta-analysis involving 3751 patients showed that the odds of delirium were 53% lower in the intervention group compared with controls (OR 0.47, 95% CI 0.38–0.58). The number needed to treat in the combined sample was 14.3 (95% CI 11.1–20.0). There was low heterogeneity, I2 = 18% with p < 0.00001. Weighting was assigned according to the inverse of the variance. Odds ratios less than 1 indicate decreased delirium incidence. RMT indicates randomized or matched trials; CI indicates confidence interval.
Falls
Four studies examined the number of falls per patient-days. Individually, only Stenvall et al., an RMT, demonstrated significant reductions in the number of falls. Combined, the meta-analysis involving 1038 patients showed that the odds of falling were 62% lower among intervention subjects (OR 0.38, 95% CI 0.25–0.60). This represents the equivalent of 4.26 falls prevented per 1000 patient-days – or 2.79 falls per 1000 patient-days among intervention subjects compared to 7.05 falls per 1000 patient-days among control subjects. There was low heterogeneity, I2 = 0.00% with p < 0.0001. Weighting was assigned according to the inverse of the variance. Odds ratios less than 1 indicate decreased rate of falls. RMT indicates randomized or matched trials; CI indicates confidence interval.