Abstract
Background:
Every pregnancy is a joyful moment for all mothers who dream of a safe pregnancy and a healthy baby. However, every pregnant woman faces the risk of sudden, unpredictable complications that could end in death or injury to herself or to her infant. Birth preparedness and complication readiness (BPACR) is a strategy that encourages pregnant women, their families, and communities to effectively plan for births and deal with emergencies, if they occur. It is a key component of globally accepted safe motherhood programs.
Objectives:
The objective of our study was to assess the status of BPACR among pregnant women and to study the socio-demographic factors affecting BPACR.
Materials and Methods:
We conducted a facility-based cross-sectional study among 417 antenatal attendees at a primary health center, Palam, New Delhi from January to April 2012. Knowledge about danger signs, planning for transport, place, and delivery by skilled birth attendant, financial management, and outcome were assessed. BPACR index was calculated.
Results:
Our study revealed that the BPACR index was very low (41%) although the preparedness level was high. Majority (81.1%) had identified a skilled attendant at birth for delivery. Nearly half of the women (48.9%) had saved money for delivery and 44.1% women had also identified a mode of transportation for the delivery. However, only 179 (42.9%) women were aware about early registration of pregnancy. Only one-third (33.1%) of women knew about four or more antenatal visits during pregnancy. Overall, only 27.8% women knew about any one danger sign of pregnancy.
Conclusion:
The level of awareness regarding BPACR was very low (41%). Efforts should be targeted to increase the awareness regarding components of BPACR among pregnant women and their families at the Primary Health Center (PHC) as well as at the community level. This will indeed go a long way in reducing morbidity as well as mortality in pregnant women, thus enabling us to reach the millennium development goal.
Keywords: Birth preparedness and complication readiness, danger signs, India, pregnancy
Introduction
Maternal mortality is a substantial burden in many developing countries. Globally, more than 40% of pregnant women may experience acute obstetric problems. The World Health Organization (WHO) estimates that 300 million women in the developing world suffer from short-term or long-term morbidities brought about by pregnancy and childbirth. Most of maternal deaths occur in the developing world.(1) With 214 maternal deaths per 100,000 live births, it remains a major public-health challenge in India (SRS)(2)
Majority of maternal deaths occur during labor, delivery, and within 24 hours post-partum. Apart from medical causes, there are numerous interrelated socio cultural factors which delay care-seeking and contribute to these deaths. Care-seeking is delayed because of the delay in
-
(a)
Identifying the complication,
-
(b)
Deciding to seek care,
-
(c)
Identifying and reaching a health facility, and
-
(d)
Receiving adequate and appropriate treatment at the health facility.(3)
Reduction of maternal mortality has been recognized as a priority concern across the globe. The International Conference on Population and Development in 1994 had recommended reduction in maternal mortality by at least 50% of the 1990 levels by the year 2000 and further one-half by the year 2015. The Millennium Development Goals (MDG) of the United Nations has set the target of achieving 200 maternal deaths per lakh of live births by 2007 and 109 per lakh of live births by 2015.
Every pregnant woman faces the risk of sudden, unpredictable complications that could end in death or injury to herself or to her infant. Pregnancy-related complications cannot be reliably predicted. Hence, it is necessary to employ strategies to overcome such problems as they arise.
Birth preparedness and complication readiness (BPACR) is one intervention that addresses these delays by encouraging pregnant women, their families, and communities to effectively plan for births and deal with emergencies, if they occur. It is a key component of globally accepted safe motherhood programs, which helps ensure women to reach professional care when labor begins and to reduce delays that occur when mothers in labor experience obstetric complications.
BPACR include many elements, including:
-
(a)
Registration of pregnancy,
-
(b)
Knowledge of danger signs,
-
(c)
Plan for where to give birth,
-
(d)
Plan for a skilled birth attendant,
-
(e)
Plan for transportation,
-
(f)
A birth companion, and
-
(g)
Identification of compatible blood donors in case of emergency.(3)
There is evidence from studies conducted in different parts of the world that promoting BPACR improves preventive behaviors, improves knowledge of mothers about danger-signs, and leads to improvement in care-seeking during obstetric emergency. We did not find any study reporting BPACR status of antenatal women in Delhi. Hence, this study was done with the objective to assess the status of BPACR among pregnant women attending a primary health center and to study the socio demographic factors affecting BPACR among the study subjects
Materials and Methods
We conducted a facility based cross-sectional study among antenatal women attendees from January-April 2012 at a Primary Health Center (PHC), Palam, Delhi. Palam, the field practice area of one of the premier tertiary level hospital at New Delhi has a total population of nearly 120,000 (Demographic survey, 2010).It has been considered an urban area since census 2001. Both government and private health agencies cater to the healthcare needs of the residents. This PHC provides primary healthcare services like immunization, antenatal care, family planning, and treatment of minor ailments to the community. Specialist services in Gynecology and Obstetrics are provided here by the senior residents from the Department of Obstetrics and Gynecology through a weekly clinic. There are a multitude of hospitals and networks of dispensaries of public health services. In addition, private practitioners of allopathy as well as of alternate systems of medicine are present in the area.
A total of 417 pregnant women who attended antenatal clinic of PHC Palam were serially included in the study. On an average, 100 new cases attend the antenatal clinic every month. It was intended to carry out the study for a period of 4 months (a quarter). Hence all pregnant women who attended the antenatal clinic for the first time during the study period were included and therefore no sampling was done. A pre-tested, semi-structured, interview schedule was prepared. The schedule included questions regarding identification data, socio-demographic profile, details about antenatal care practices, preferred place of delivery, knowledge of danger signs during pregnancy, labor and puerperium, identification of place or personnel for delivery, and arrangement for money and transport.
Socio-economic status was classified into two categories:
-
(a)
Those above poverty line (APL) and
-
(b)
Those below poverty line (BPL).
The cut-off for APL for Delhi state has been defined as those whose per capita income is more than 1,134 rupees per capita per month and the rest under BPL.(4) The study was approved by institutional ethical review board. After taking an informed consent, the women were interviewed. BPACR was measured using a series of questions including knowledge about danger signs, planning for transport, place, and delivery by skilled birth attendant, financial management, and outcome. BPACR index was calculated by a set of indicators. These indicators are quantifiable and expressed in percentage of women having specific characteristics. BPACR index has been developed by the Johns Hopkin Bloomberg School of Public Health and has been used in many studies conducted worldwide including India.
BPACR index was calculated from the following indicators:
Percentage of the women who knew about > 8 danger signs of pregnancy.
Percentage of the women who knew about financial assistance provided by government in Janani Suraksh Yojana (JSY).
Percentage of the women who knew about transportation provided by government in JSY.
Percentage of the women who availed Antenatal Care (ANC ) in 1st trimester by skilled provider.
Percentage of the women who identified skilled birth attendant for delivery.
Percentage of the women who identified mode of transportation.
Percentage of the women who saved money to pay for expenses.
BPACR index was calculated as ∑Indicator/7
BPACR index which includes indicators like knowledge about danger signs of pregnancy, financial assistance, and transportation provided by government in JSY, ANC services in 1st trimester by skilled provider, registration of pregnancy, identification of a skilled birth attendant for delivery and mode of transportation, saving money to pay for expenses were the dependent variables while respondents age,education and occupation, husband's age, education and occupation, socio-economic status, parity, type of family were considered as independent variables. Data were entered and analyzed in Statistical Package for the Social Sciences (SPSS) version 12. Descriptive statistics were used to describe the distribution of all variables. Bi variate analysis using Chi-square was used to examine the association between each independent variable and BPACR indicators.
Results
Respondent characteristics
A total of 417 women participated in our study with no refusals. The mean age of the respondents was 24.2 years (standard deviation, SD 3.64) with nearly equal numbers (37.2% and 37.4 %) in 20-24 years and 25-29 years age-group, respectively and 7.7 % in 30-34 years. Only one subject was less than 18 years and only 5 (1.2%) were above 35 years. On the contrary, majority of their husbands (71.9%) belonged to the age-group 25-34 years. The mean age at marriage was 20.1 (range 9-31yrs) and mean age at 1st childbirth was 21.56 range (15-33 yrs).
Almost 1/5th (20.4%) subjects were illiterate as compared to only (9.6%) of their husbands. Nearly one-fourth (24.0%) had completed primary and middle school. One hundred and fifty-eight (37.9%) had completed high school and intermediate level as against 43.7 % in husbands. Only 74 (17.7%) were graduates or professionals as compared to one-fourth (25.4%) of their husbands. Majority of the subjects were homemakers (90.6%). Only 3.8 % of their husbands were unemployed. Only 8 (1.9%) women were involved in unskilled and semi-skilled work. Similar numbers of women were engaged in semi-professional or professional work as against 10.1% of their husbands. More than half (57.6 %) of their husbands were involved in semi-skilled and skilled work. Sixty-two (14.9) were shop owners/clerks. Only 30 (7.2%) subjects belonged to below poverty line socio-economic status and the rest (92.8%) were above poverty line. Majority of the subjects (92.8%) were Hindus followed by (4.8%) Muslims and Sikhs (1.9%). More than half (56.6%) the subjects stayed in joint families, whereas 181 (43.4%) belonged to nuclear families. Almost half of the women were primigravida (47.5%), 39.8% were para one, and 9 women (2.2%) were para 3 and above.
Almost half of the women (54.2%) registered themselves in the second trimester, whereas only 179 women (42.9%) registered themselves in the first trimester of pregnancy. There were 12 (92.9%) women who registered even in the third trimester.
Majority (90.2%) of the women were registered at government health facilities and the rest (9.8%) in private health facilities. Women under study were in different periods of gestation. Therefore, only those women (33.1%) who were nearing term or in the third trimester had completed four or more antenatal visits and the remaining 2/3rds had less than four visits.
Awareness regarding antenatal care and danger signals during pregnancy and labor
Table 1 shows the awareness of study subjects regarding various aspects of antenatal care. Only 179 (42.9%) women were aware about early registration of pregnancy. Only one-third (33.1%) of women knew about four or more antenatal visits during pregnancy. More than three-fourths (83.2%) of the women were aware about tetanus (TT) immunization. About one-third (32.6%) women knew about consumption of iron folic acid (IFA) tablets during pregnancy and were aware about transportation (32.7%) and financial assistance provided by government in JSY scheme (37.2%).
Table 1.
Awareness regarding antenatal care and danger signals during pregnancy and labor
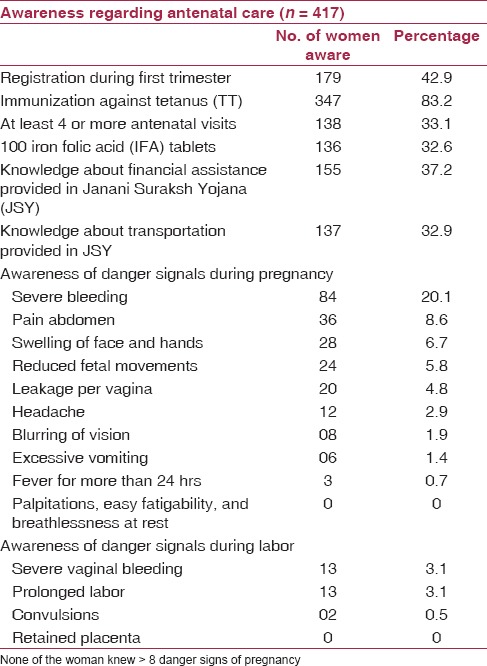
Table 1 also depicts the awareness of antenatal women regarding various danger signs of pregnancy. Overall, one-fifth (27.8%) women knew about anyone danger sign of pregnancy The most common danger signs known were severe bleeding (20.1%) followed by pain abdomen (8.6%), swelling of face and hands (6.7%), and reduced fetal movement (5.8%).
Only 28 (6.7%) knew about danger signs in labor [Table 1] and only 3 (0.7%) knew about danger sign during puerperium (not shown in the Table).
The various sources from where this knowledge regarding danger signs was acquired was elders/mother-in-law in 50 (45.8%), doctor in 29 (26.6) %), friends in 11 (10.0%), and other sources in 18 (16.6%).
BPACR status
Table 2 shows the status of BPACR among antenatal women. Majority (81.1%) had identified a skilled attendant at birth for delivery. Nearly half of the women (48.9%) had saved money for delivery and 44.1% women had also identified a mode of transportation for the delivery. One hundred and seventy-nine (42.9%) women had registered themselves in the first trimester and availed antenatal care also.
Table 2.
Status of birth preparedness among the pregnant women
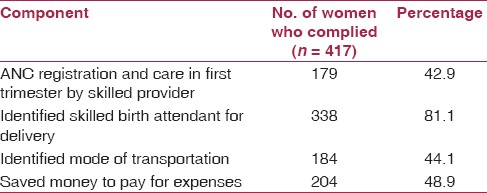
BPACR index was calculated as ∑Indicator/7 which was observed to be 41%.
Association between some independent variables and BPACR Components
The results of the test of association between the independent variables and various components of BPACR are shown in Table 3. We found that age and education of women were highly statistically significantly associated with their knowledge of danger signs of pregnancy (P = 0.000). Education of women (P = 0.001) and parity (P = 0.000) were also statistically significantly associated with their knowledge about early registration of pregnancy.
Table 3.
Factors associated with birth preparedness and complication readiness
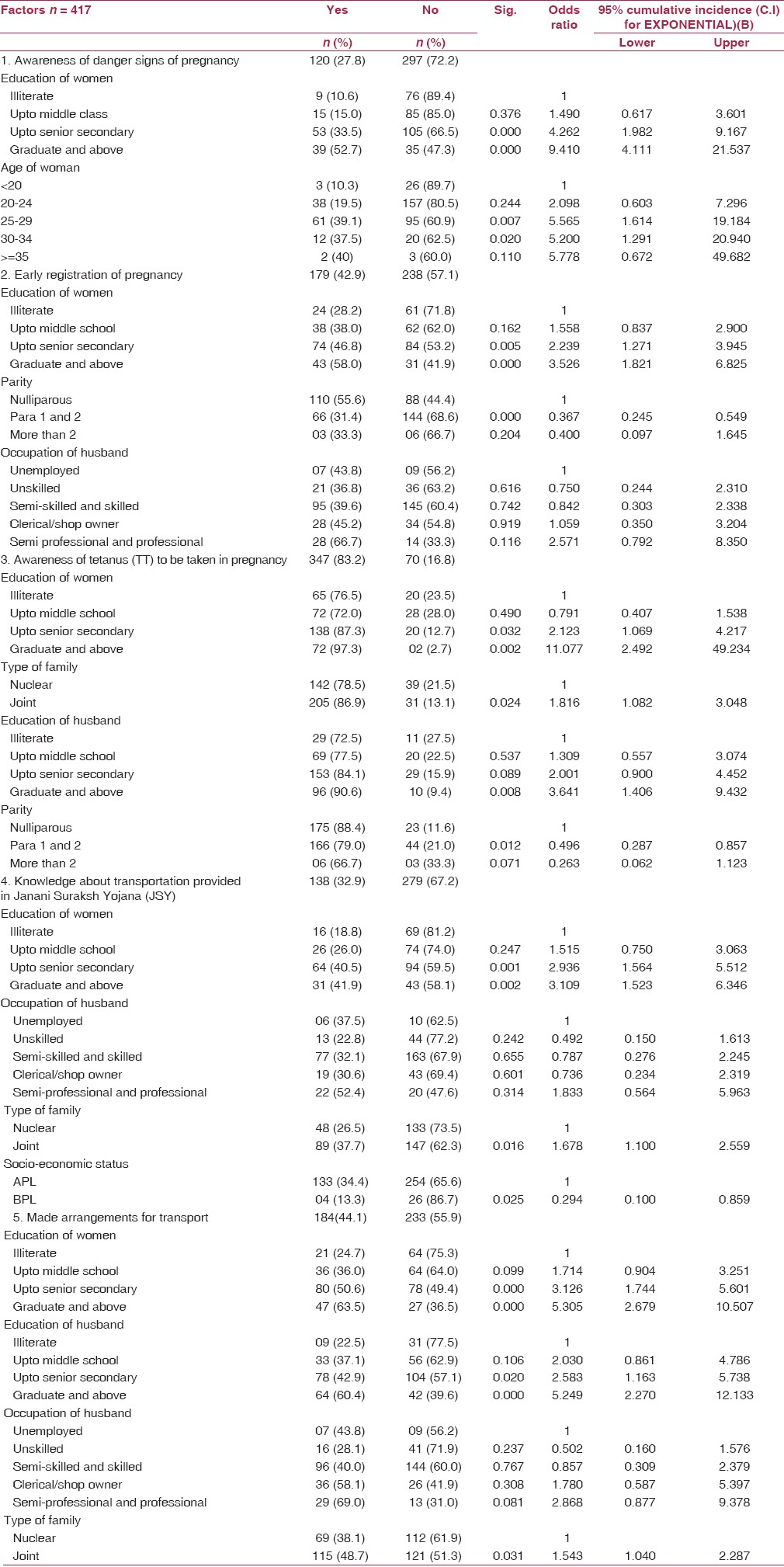
Education of women (P = 0.00) and her husband (P = 0.02), parity (P = 0.01), and type of family (P = 0.02) were also statistically significantly associated with their awareness about TT immunizations in pregnancy.
Similarly, education of women (P = 0.001), type of family (joint) (P = 0.01) and Socio-economic Status (SES) (P = 0.01) were statistically significantly associated with their awareness about transportation provided by JSY scheme.
Education of women (P = 0.000) and their husbands (P = 0.000), occupation of husband (P = 0.000), and type of family (0.03) were also statistically significantly associated with the women who had made arrangements for transport before delivery.
On statistical analysis, it was seen that among multiparous women awareness regarding danger signals was significantly higher (P = 0.002). Awareness for transport provided (P = 0.016) and financial assistance under JSY was also significantly higher among multiparous women (P = 008). For other components of BPACR, the difference was not found to be statistically significant.
It was seen that women who were educated up to middle school and above were more aware about early danger signs of pregnancy, early registration of pregnancy, awareness of TT immunization, knowledge about transportation provided by JSY, identification of a place/person for delivery, and arrangements for transport during delivery.
Discussion
BPACR is the process of planning for normal birth and anticipating the actions needed in case of an emergency.
In many societies in the world, cultural beliefs, and lack of awareness inhibit preparation in advance for delivery and expected baby. The majority of pregnant women and their families do not know how to recognize the danger signs of complications. When complications occur, the unprepared family wastes a great deal of time in recognizing the problem, getting organized, getting money, finding transport, and reaching the appropriate referral facility.
Birth preparedness is a strategy to promote the timely use of skilled maternal and neonatal care, especially during childbirth, based on the theory that preparing for childbirth reduces delays in obtaining this care. Despite the great potential of BPACR in reducing the maternal and newborn deaths its status is not well-known.
In our study, overall level of awareness regarding danger signs of pregnancy was very low (27.8%), followed by poor knowledge of danger signs of labor (6.7%), whereas only three women (0.7%) knew about danger signs during puerperium. And, 81.1% of women had identified a skilled provider for birth which is similar to a multicentric study conducted in Nigeria, where it was reported that awareness of the concept of birth preparedness was high (70.6%) but knowledge of specific danger signs was poor. Education and parity were reported to be the best predictors of awareness of birth preparedness.(5) In another study done in Nigeria,(6) similar results regarding poor awareness of danger signs (28.3%) were reported.
In a study conducted in Ethiopia, poor comprehensive knowledge and practices of birth preparation and complication readiness were reported. Out of 534 women included in the study, only 22% of the respondents were prepared for birth and its complications. In multivariate analysis, preparation for birth and its complication was higher among literate mothers, women with parity range of 2 to 4, women with history of still birth and those who were advised about birth preparedness during their antenatal care follow-up.(7)
In another study conducted in Southern Ethiopia among 743 pregnant women, it was highlighted that only a quarter (20.5%) of pregnant women identified skilled provider. Only 8.1% identified health facility for delivery and/or for obstetric emergencies. Preparedness for transportation was also found to be very low (7.7%). Overall, only 17% of pregnant women were well prepared.(8)
In a United Nations International Children's Education Fund (UNICEF) collaborative study in Burkina Faso, it was reported that although knowledge for danger signs was poor, majority of women reported planning for birth. And, 43.4% planned for a birth provider, 46.1% planned for transportation, and 83.3% planned to save money in the case of an emergency.(9) In a similar study done in Kenya,(10) 84.3% had saved money for labor; and in study conducted done in Nigeria,(6) 87.5% had decided the place of delivery, 64.8% had saved money for delivery, and 62.3% had made arrangements for transport which is similar to the present study where though the knowledge of danger signs was poor, women had planned for their birth, planned for transportation, and saved money also .
A field trial conducted in the neighboring country of Nepal concluded that birth preparedness programs can positively influence knowledge and intermediate health outcomes, such as household practices and use of some health services. It was recommended that such programs can be implemented by government health services with minimal outside assistance but should be comprehensively integrated into the safe motherhood program rather than implemented as a separate intervention.(11) Studies conducted in India have highlighted poor levels of preparedness among women. In a study conducted among 312 recently delivered women in 11 slums of Indore, it was reported that less than half of the mothers (47.8%) were well-prepared. Although awareness of the mothers about at least one danger-sign of pregnancy and delivery was not low, being 79.2% and 78.5%, respectively; however, nearly three-fourths of the deliveries took place in the home. Overall, only 32% of the deliveries (home and health facility combined) were attended by skilled birth attendants. Skilled attendance during delivery was three times higher in well-prepared mothers as compared to less-prepared.(12)
A study conducted among pregnant and recently delivered mothers in Rewa district of Madhya Pradesh also highlighted similar findings. Overall BP and CR index was found to be 47.5%. Index did not differ significantly between pregnant and recently delivered mothers. This study revealed poor level of knowledge about key danger signs and transportation services among mothers. The BPACR index was similar to the present study (41%). Knowledge about financial assistance was high. The study showed that majority of the women had planned for skilled provider and transport but less than half (44.2%) of the mothers planned for saving money. Husband and in-laws play dominant role in decision-making. This finding can be utilized for targeting men in Information, Education and Communication (IEC) activities.(13)
Our study showed that parity, younger age, education, joint family system, and husband's education and occupation were associated with having a birth plan.
Woman's education (P = 0.001) and her spouse's education (P = 0.02) up to middle school and above were strong predictors of BPACR which is similar to a study done in rural Uganda where women's education and her spouse's education are significantly associated with BPACR(14) and a study done in Kenya(10) also reported women's education having positive influence on birth preparedness.
The low level of BPACR in present study is largely attributed to low level of awareness regarding danger signals during pregnancy and labor. Although 81% of women had identified a birth attendant for delivery, less than half had identified a mode of transport (44%) or saved money to pay for the expenses (48%). The role of health workers becomes pertinent in such scenario to improve BPACR. There is a need to involve other family members, especially the decision makers so that BPACR can be improved.
There is enough evidence to suggest that the level of BPACR is low in many societies. Antenatal care provides a golden opportunity to all the pregnant women to provide information, education and communication so that they along with their families can make the correct choices especially in event of any complications arising during delivery, childbirth or post-partum. This opportunity is missed many a times due to a number of reasons which should be addressed at the individual, family, community and the health provider's level.
Conclusion
The BPACR index in the present study was 41 %. Our study showed that though there was poor awareness of danger signs during pregnancy, labor as well as puerperium, the level of birth preparedness was high. And, 81.1% women had identified a skilled birth attendant for delivery. Education of women beyond middle school was the most important factor associated with awareness regarding various components of BPACR. Repeated IEC awareness programs may be initiated at the PHC towards community participation so that BPACR status improves for these women. This will be a positive step toward achieving the millennium development goal 5 of safe motherhood and reduction in maternal mortality.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.WHO; UNICEF; UNFPA. Maternal Mortality in 2005: Estimates Developed by WHO, UNICEF, UNFPA. Geneva: WHO; 2007. [Last accessed on 2013 Oct 30]. Available from: http://www.who.int/whosis/mme_2005.pdf . [Google Scholar]
- 2.SRS. Special Bulletin on Maternal Mortality in India 2007-09. Office of Registrar General of India. 2011. [Last accessed on 2013 Oct 30]. Available from: http://www.censusindia.gov.in/vital_statistics/SRS_Bulletins/Final-MMR%20Bulletin-2007-09_070711.pdf .
- 3.Monitoring birth preparedness and complication readiness. Tools and indicators for maternal and newborn health. Baltimore: JHPIEGO; 2004. [Last accessed on 2013 Nov 1]. Maternal and Neonatal Health Programme. Available from: http://www.jhpiego.org/files/BPACRtoolkit.pdf . [Google Scholar]
- 4.Poverty Estimates for 2011-12 - of Planning Commission. [Last accessed on 2013 Oct 30]. Available from: http://planningcommission.nic.in/news/pre_pov2307.pdf .
- 5.Ekabua JE, Ekabua KJ, Odusolu P, Agan TU, Iklaki CU, Etokidem AJ. Awareness of birth preparedness and complication readiness in southeastern Nigeria. ISRN Obstet Gynecol. 2011;2011:560641. doi: 10.5402/2011/560641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Onayade AA, Akanbi OO, Okunola HA, Oyeniyi CF, Togun OO, Sule SS. Birth preparedness and emergency readiness plans of antenatal clinic attendees in Ile-Ife, Nigeria. Niger Postgrad Med J. 2010;17:30–9. [PubMed] [Google Scholar]
- 7.Hiluf M, Fantahun M. Birth Preparedness and Complication Readiness among women in Adigrat town, north Ethiopia. [Last accessed on 2013 Oct 30];Ethiop J Health Dev. 2007 22:14–20. Available from: http://www.ajol.info/index.php/ejhd/article/download/10057/31331 . [Google Scholar]
- 8.Hailu M, Gebremariam A, Alemseged F, Deribe K. Birth preparedness and complication readiness among pregnant women in Southern Ethiopia. PLoS One. 2011;6:e21432. doi: 10.1371/journal.pone.0021432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moran AC, Sangli G, Dineen R, Rawlins B, Yameogo M, Baya B. Birth-preparedness for maternal health: Findings from Koupéla District, Burkina Faso. J Health Popul Nutr. 2006;24:489–97. [PMC free article] [PubMed] [Google Scholar]
- 10.Mutiso SM, Qureshi Z, Kinuthia J. Birth preparedness among antenatal clients. East Afr Med J. 2008;85:275–83. doi: 10.4314/eamj.v85i6.9625. [DOI] [PubMed] [Google Scholar]
- 11.McPherson RA, Khadka N, Moore JM, Sharma M. Are birth-preparedness programmes effective. Results from a field trial in Siraha district, Nepal? J Health Popul Nutr. 2006;24:479–88. [PMC free article] [PubMed] [Google Scholar]
- 12.Agarwal S, Sethi V, Srivastava K, Jha PK, Baqui A. Birth preparedness and complication readiness among slum women in Indore city, India. J Health Popul Nutr. 2010;28:383–91. doi: 10.3329/jhpn.v28i4.6045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.NIHFW, UNFPA, SS Medical College, Rewa. A study for assessing birth preparedness and complication readiness intervention in Rewa district of Madhya Pradesh. 2008-9. [Last accessed on 2013 Oct 30]. Available from: http://nihfw.org/pdf/RAHI-II%20Reports/REWA.pdf .
- 14.Kakaire O, Kaye DK, Osinde MO. Male involvement in birth preparedness and complication readiness for emergency obstetric referrals in rural Uganda. Reprod Health. 2011;8:12. doi: 10.1186/1742-4755-8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]


