Abstract
Esophageal carcinoma arising within an epiphrenic diverticulum is rare. We describe a case of a carcinoma in a long-standing epiphrenic diverticulum in a 62-year-old patient. Fluorine-18-2-Fluoro-2-Deoxy-D-Glucose Positron Emission Tomography and Computed Tomography, and endoscopic ultrasound revealed a hypermetabolic mass within the diverticulum. A preoperative diagnosis was made via endoscopic biopsy. The patient underwent Ivor-Lewis esophagectomy. He remains well and free of recurrence 18 months after surgery.
Keywords: Fluorine-18-2-Fluoro-2-Deoxy-D-Glucose Positron Emission Tomography and Computed Tomography, FDG, PET/CT, Carcinoma, Hypermetabolic, Epiphrenic, Diverticulum
CASE REPORT
A 62-year-old male presented with an 8-week history of worsening dysphagia to liquids and solids, and a 15 lb unintentional weight loss. He had been diagnosed with an epiphrenic diverticulum 7 years prior, but previously was only minimally symptomatic with occasional reflux and discomfort. In light of his worsening symptoms, endoscopy was performed. Endoscopy revealed a large diverticulum at 35 cm from the incisors, within which there was a friable mass (Fig 1). The gastroesophageal junction was normal, at 40 cm from the incisors.
Figure 1.
62 year old male with carcinoma in esophageal diverticulum. A) Endoscopic view showing esophageal diverticulum (double asterix) and esophageal lumen (single asterix). B) Endoscopic view showing mass within the esophageal diverticulum (arrow).
Imaging findings
Endoscopic ultrasound (EUS) was done with 5 MHz radial echoendoscope. The EUS revealed hypoechoic mass in the diverticulum (Fig 2). The mass did not invade the mediastinum. Endoscopic biopsy showed squamous cell carcinoma. He subsequently underwent Fluorine-18-2-Fluoro-2-Deoxy-D-Glucose Positron Emission Tomography and Computed Tomography (FDG-PET/CT) which showed a hypermetabolic mass lesion measuring 3.6 × 3.1 × 3.4 cm within the diverticulum measuring 4.8 × 4.8 × 5.4 cm, arising from the distal esophagus (Fig 3); the average standardized uptake value (SUV) was 10.2 and maximal SUV was 14.8. PET/CT showed no evidence of regional lymphadenopathy or metastatic disease.
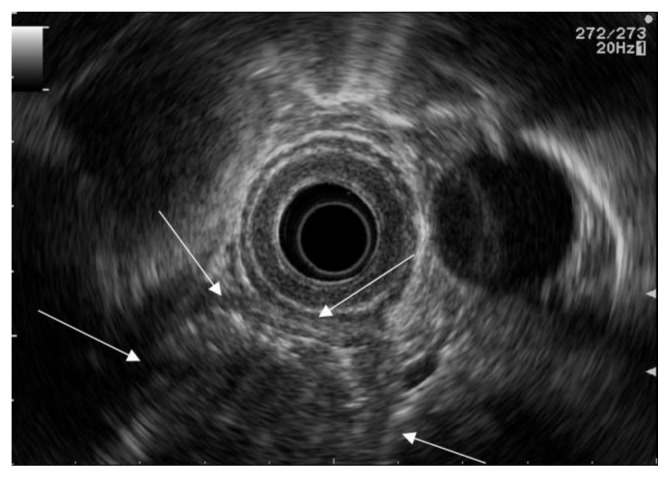
Figure 2.
62 year old male with carcinoma in esophageal diverticulum. Endoscopic ultrasound with 5 MHz radial echoendoscope (GF-UM140, Olympus America Inc., Melville, NY) advanced in to the esophagus, to the level of diverticulum, showing hypoechoic mass (arrows) measuring 3.6 × 3.1 × 3.4 cm in the esophageal diverticulum.
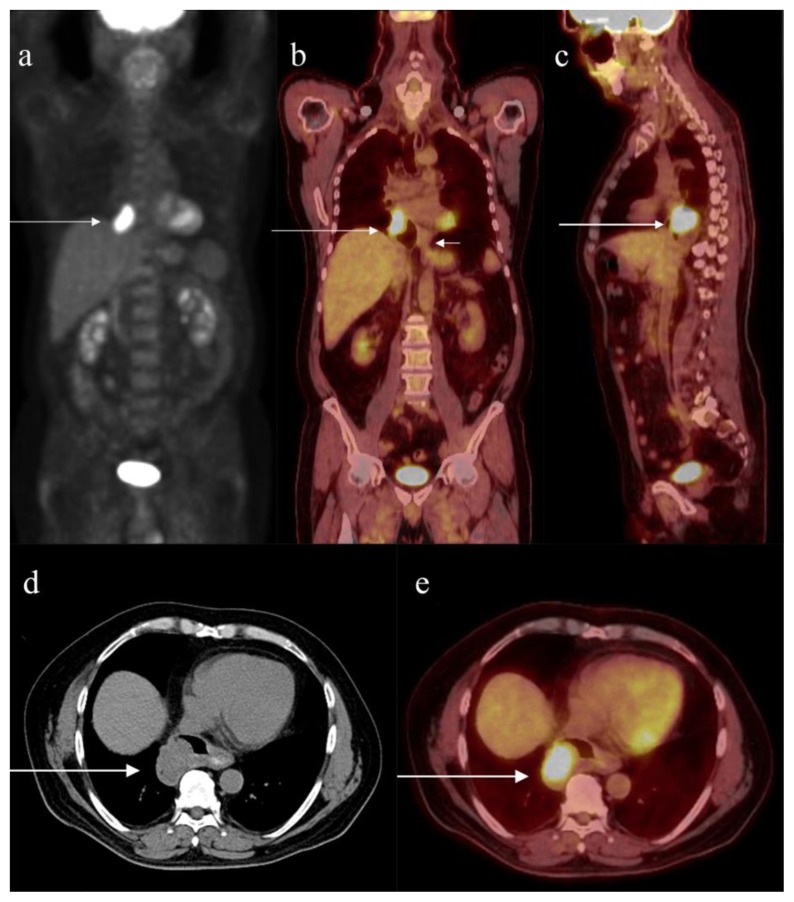
Figure 3.
62 year old male with carcinoma in esophageal diverticulum. A) Maximum intensity projection of FDG PET scan showing the hypermetabolic lesion with average SUV 10.2 and maximal SUV 14.8, in the region of right cardiophrenic angle (arrow). PET scanning of the body from the skull base to the upper thighs was performed 90 minutes after administration of 14.57 milli-Curie Ci of F18 FDG intravenously. Helical CT from the skull base to the upper thighs with 4 mm axial slices with dilute barium as oral contrast and without intravenous contrast was also performed and used for PET attenuation correction and localization. The PET images were reconstructed in axial, sagittal, and coronal planes and were fused with the reconstructed CT images in axial, sagittal, and coronal planes.
B) Coronal fused FDG-PET/CT showing the hypermetabolic lesion within the epiphrenic diverticulum (long arrow). Short arrow shows the esophago-gastric junction.
C) Sagittal fused FDG-PET/CT showing the hypermetabolic lesion within the epiphrenic diverticulum (arrow).
D) Axial image of CT portion of FDG-PET/CT showing the mass (arrow) measuring 3.6 × 3.1 × 3.4 cm within the epiphrenic diverticulum measuring 4.8 × 4.8 × 5.4 cm.
E) Axial fused FDG-PET/CT showing the hypermetabolic mass (arrow) measuring 3.6 × 3.1 × 3.4 cm, with average SUV 10.2 and maximal SUV 14.8, within the epiphrenic diverticulum.
Management
The patient underwent Ivor-Lewis esophagectomy and wedge resection of the lower lobe of right lung, as there were adhesions with the esophageal diverticulum. The patient also had mediastinal lymph node dissection, pyloromyotomy and insertion of feeding jejunostomy tube. The pathological specimen showed diverticulum containing a mass measuring 3.2 × 2.5 × 3.1 cm. The opening of the diverticulum measured 3.1cm from gastroesophageal junction. The esophagus was adherent to pleura by fibrosis, without evidence of tumor. Microscopic examination revealed moderately differentiated squamous cell carcinoma, invading through the muscularis propria into the periesophageal soft tissue. The proximal and distal margins were uninvolved by carcinoma. Distance of carcinoma from closest resection margin was 6.7 cm. There was no lymph-vascular invasion. None of the 26 lymph nodes (periesophageal and perigastric) examined showed any histopathologic abnormality. Final pathological staging was pT3N0M0.
Follow-up
The patient’s post-operative course was uneventful and patient was discharged home in stable condition on post-op day 7. There was no evidence of recurrence or metastases at 18 months follow up.
DISCUSSION
Etiology & demographics
Esophageal cancer is not uncommon; estimates for esophageal cancer in the United States are about 17,990 new cases diagnosed for 2013 [1]. Carcinoma in epiphrenic diverticula is rare. Herbella et al in a review of entire medical literature in 2011, found only 17 cases of squamous cell carcinoma arising in epiphrenic diverticula [2]. The majority (83%) of the patients were elderly male, with the mean age of 68 years. The mean time from the start of symptoms to diagnosis was 7 years and mean size of the diverticula was 5 cm. Our patient had similar characteristics in terms of age, gender, size of the diverticulum and time interval between the onset of the symptoms and cancer diagnosis. The pathophysiological mechanisms of carcinogenesis in esophageal diverticula are presumed to be chronic irritation by stasis of food, inflammation or repeated injury [3].
Clinical & imaging findings
Preoperative diagnosis of a carcinoma in an esophageal diverticulum may be difficult as symptoms associated with malignancy mimic those of the diverticulum alone or the underlying esophageal motor disorder. Progressive dysphagia and unintentional weight loss are key symptoms suggesting further evaluation to rule out associated malignancy [4]. Uncommon symptoms such as melena, hematemesis or hemoptysis are also concerning for malignancy [5]. In general, barium swallow may demonstrate esophageal lesions such as cancer or stricture associated with diverticulum [4]. However, barium esophagogram may be misleading as cancerous lesions may be masked by food residue within the diverticulum [6]. Progressive reduction in the apparent size of the epiphrenic diverticulum, filling defect in the diverticulum, or irregularity or apparent stenosis of the esophageal lumen near the diverticulum should be investigated to rule out malignant change instead of attributing the findings to retention of food [4]. Esophagoscopy allows inspection and biopsy of the esophageal mucosa and should be performed to exclude malignancy [6]. However, the tumor may be concealed by food materials within the diverticulum even in esophagoscopy [4]. Computed tomography is helpful in evaluating the mass lesion arising from the diverticulum and plays an important role in staging and surgical management of esophageal cancer [4]. Riddell et al developed criteria for local staging of esophageal cancer using high resolution T2 weighted imaging with external surface coil, and demonstrated the potential for using it as an alternative non-invasive staging technique [7]. Oberholzer et al found that tumor microcirculation in esophageal cancer differs with histological subtypes, and that tumor microcirculation can be quantitated by DCE MRI [8]. These studies show the potential of using MRI for evaluating suspected cases of carcinoma in esophageal diverticulum. FDG PET/CT, in which the FDG PET provides metabolic information and the CT provides anatomic details in a single procedure, has been shown to be useful for evaluation of numerous cancers, including esophageal carcinoma. It provides evaluation for distant metastases as well. Some reports suggest a limited role for FDG-PET/CT in the evaluation for regional nodal metastases [9]. However in the recent study by Tanabe et al, FDGPET/CT had a high diagnostic accuracy (87.3%) for detecting regional lymph nodal metastases [10]. Due to limitations in the technique for detection of small foci of cancer, FDG-PET/CT may not detect thin superficial primary lesions or microscopic nodal metastases [9]. In our case, FDG-PET/CT clearly demonstrated the malignant mass arising from the esophageal diverticulum as a hypermetabolic region within the diverticulum. FDG-PET/CT also showed the absence of lymph node or distant metastases. To the best of our knowledge, this is the first report in which FDG-PET/CT was used for evaluating carcinoma arising from an esophageal diverticulum.
A high degree of clinical suspicion and appropriate evaluation of patients with esophageal diverticula may enable early detection of malignancy. We suggest that FDG-PET/CT can be a complementary diagnostic tool for evaluating esophageal diverticulum for associated malignancy, especially when endoscopy and barium esophagography are equivocal due to food debris. FDG-PET/CT should also be considered in patients with known esophageal diverticula who have symptoms concerning for associated carcinoma when they are reluctant to undergo endoscopy, in order to avoid a delay in diagnosis and poor prognosis. FDG-PET/CT can be an effective diagnostic tool, and is complementary to endoscopy in evaluation of patients with esophageal diverticula.
Treatment & prognosis
Treatment of cancer in a diverticulum follows the same principles of the treatment for esophageal carcinoma. Different treatment approaches have been described, from radiotherapy alone to resection plus chemoradiotherapy, depending on the staging of the tumor. The outcomes are generally considered poor due to delayed diagnosis, except for superficial carcinomas [2].
Differential Diagnoses
Filling defect in the diverticulum in barium esophagogram and CT scan could be due to food residue/debris or malignancy within the diverticulum. Mass lesion which shows hypermetabolic activity represents malignancy, while food residue/debris does not show metabolic activity. Increased FDG uptake alone within a diverticulum without associated mass could be due to esophagitis.
TEACHING POINT
FDG-PET/CT can be used as a diagnostic tool for evaluating esophageal diverticulum for associated malignancy, especially when endoscopy or imaging modalities are equivocal due to food debris. FDG-PET/CT should also be considered in patients with known esophageal diverticula who have symptoms concerning for associated carcinoma when they are reluctant to undergo endoscopy, in order to avoid a delay in diagnosis and poor prognosis.
Table 1.
Summary table for squamous cell carcinoma arising from epiphrenic diverticulum.
| Etiology | Squamous cell carcinoma in epiphrenic diverticulum |
| Incidence | 17 cases as per review of entire medical literature by Herbella et al. |
| Gender ratio | Male:Female=4:1 |
| Age predilection | Elderly patients, Mean age 68 years |
| Risk factors | Diverticulum |
| Treatment | Depending on the staging of the tumor. Resection, radiotherapy, chemoradiation, resection plus chemoradiation. |
| Prognosis | Poor prognosis, unless diagnosed early |
| Findings on imaging |
Barium Swallow: Filling defect within the diverticulum CT: Soft tissue filling defect within the diverticulum MRI: Intermediate T2 signal intensity lesion. Contrast enhancement. Restricted diffusion. PET/CT: Hypermetabolic mass with increased FDG uptake within the diverticulum |
Table 2.
Differential diagnosis table for filling defects within an epiphrenic diverticulum
| Differential | Barium swallow | CT scan | PET/CT | MRI |
|---|---|---|---|---|
| Carcinoma within the epiphrenic diverticulum | Filling defect within the diverticulum | Soft tissue within the diverticulum may show enhancement. Sometimes difficult to differentiate from debris | Hypermetabolic soft tissue lesion within the diverticulum | Intermediate T2 signal intensity lesion. Contrast enhancement. Restricted diffusion. |
| Food particle and debris within the epiphrenic diverticulum | Filling defect within the diverticulum, may change position | Soft tissue filling defect within the diverticulum | Filling defect within the diverticulum without any metabolic activity. | Heterogeneous signal intensity. No contrast enhancement. |
| Esophagitis associated with diverticulum | May show mucosal changes of esophagitis | May show diffuse wall thickening | May show increased uptake of Fluorine-18–2-Fluoro-2-Deoxy-D-Glucose without associated mass. | Periesophageal edema. Contrast enhancement. No restricted diffusion. |
ABBREVIATIONS
- EUS
Endoscopic ultrasound
- FDG-PET/CT
Fluorine-18-2-Fluoro-2-Deoxy-D-Glucose Positron Emission Tomography and Computed Tomography
- SUV
Standardized uptake value
REFERENCES
- 1.What are the key statistics about cancer of the esophagus? [Accessed December 12, 2013]. Available at http://www.cancer.org/cancer/esophaguscancer/detailedguide/esophagus-cancer-key-statistics.
- 2.Herbella FAM, Dubecz A, Patti MG. Esophageal diverticula and cancer. Diseases of the Esophagus. 2012;25:153–158. doi: 10.1111/j.1442-2050.2011.01226.x. [DOI] [PubMed] [Google Scholar]
- 3.Kimura H, Konishi K, Tsukioka Y, et al. Superficial esophageal carcinoma arising from the diverticulum of the esophagus. Endoscopy. 1997;29:S53–54. doi: 10.1055/s-2007-1004331. [DOI] [PubMed] [Google Scholar]
- 4.Lai S, Hsu C. Carcinoma Arising from an Epiphrenic Diverticulum: A Frequently Misdiagnosed Disease. Ann Thorac Cardiovasc Surg. 2007;13:110–113. [PubMed] [Google Scholar]
- 5.Schultz SC, Byrne DM, De Cunzo P, et al. Carcinoma arising within epiphrenic diverticula. A report of two cases and review of the literature. J Cardiovasc Surg (Torino) 1996;37:649–651. 1996. [PubMed] [Google Scholar]
- 6.Turner MJ. Carcinoma as a complication of pharyngeal pouch. Br J Radiol. 1963;36:206–210. doi: 10.1259/0007-1285-36-423-206. [DOI] [PubMed] [Google Scholar]
- 7.Riddell AM, Allum WH, Thompson JN, et al. The appearances of oesophageal carcinoma demonstrated on high-resolution, T2-weighted MRI, with histopathological correlation. Eur Radiol. 2007;2:391–399. doi: 10.1007/s00330-006-0363-6. [DOI] [PubMed] [Google Scholar]
- 8.Oberholzer K, Pohlmann A, Schreiber W, et al. Assessment of tumor microcirculation with dynamic contrast-enhanced MRI in patients with esophageal cancer: initial experience. J Magn Reson Imaging. 2008;6:1296–1301. doi: 10.1002/jmri.21305. [DOI] [PubMed] [Google Scholar]
- 9.Erasmus JJ, Rohren EM, Hustinx R. PET and PET/CT in the Diagnosis and Staging of Esophageal and Gastric Cancers. PET Clinics. 2008;3:135–145. doi: 10.1016/j.cpet.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 10.Tanabe S, Naomoto Y, Shirakawa Y, et al. F-18 FDG PET/CT contributes to more accurate detection of lymph nodal metastasis from actively proliferating esophageal squamous cell carcinoma. Clin Nucl Med. 2011;36:854–859. doi: 10.1097/RLU.0b013e318217adc9. [DOI] [PubMed] [Google Scholar]