Abstract
Purpose
Primary spinal cord and appendage tumors (PSCAT) originating from the spinal cord, spinal meninges, and cauda equina are uncommon. Worldwide, population-based cancer registry data are mostly based on malignant tumors only, which means few data are available on PSCATs, including non-malignant tumors. Therefore, the objective of this study was to provide information regarding the incidence of both non-malignant and malignant PSCATs in Korea on a national level.
Materials and Methods
Incidence of PSCATs was estimated from cases diagnosed between 2006 and 2010 using the National Cancer Incidence Database in Korea. Age-adjusted rates were calculated using the world standard population, and male-to-female rate ratios were calculated by histology type.
Results
Of all PSCATs registered (n=3,312), 86.6% were non-malignant. The overall age-adjusted incidence of PSCATs was 1.08 per 100,000 person-years, with an incidence of 0.99 per 100,000 in females and 1.15 in males. The most common site of PSCATs was the spinal cord (83.4%), followed by spinal meninges (16.1%) and cauda equina (0.5%). The most common histological type was neurilemmoma (41.3%), followed by meningiomas (20.1%) and ependymomas (7.6%). Men had significantly higher rates than women for ependymomas and lymphomas but had lower rates for meningiomas.
Conclusion
This study provides the first population-based analysis of PSCATs in Korea.
Keywords: Primary spinal tumors, Epidemiology, Incidence, Population-based, Korea
Introduction
Primary spinal cord and appendage tumors (PSCATs), including tumors of the spinal cord, spinal meninges, and cauda equina are one of the rarest types of tumors, comprising 4%-8% of tumors arising from the central nervous system (CNS) [1-6]. It is important to accurately determine the epidemiology of PSCATs for decision-making regarding treatment as well as research and health care planning [4,5,7-10]. Only a small number of populationbased data concerning PSCATs are available, and there are no population-based data from Asian countries.
The Korea Central Cancer Registry (KCCR) constructed the Korea National Cancer Incidence Database (KNCIDB), which publishes an annual report of the national cancer incidence rate. In 2005, the first national cancer incidence statistics for the years between 1999 and 2001 were reported by the KCCR [11]. The KCCR collected data only on malignant tumors prior to 2005. This exclusion of non-malignant cases restricted the ability to accurately estimate the incidence of PSCATs in Korea. In 2004, the KCCR revised its criteria for cancer registration to include non-malignant primary brain and CNS tumors (benign, uncertain, and unknown behaviors). In January 2005, the KCCR began collecting data on non-malignant primary brain and CNS tumors, including PSCATs [12]. Consequently, we were able to more accurate determine incidences of PSCATs.
The objective of this study was to provide more detailed estimates of population-based incidences of all primary malignant and non-malignant PSCATs diagnosed between 2006 and 2010 in Korea.
Materials and Methods
The Korean Ministry of Health and Welfare initiated the nationwide cancer registry (KCCR) in 1980 [11]. The KCCR expanded cancer registration to cover the entire Korean population since 2003. KCCR data from 1999 to 2002 were published as the ‘Cancer Incidence in Five Continents,' which reflects the completeness and validity of incidence data in Korea [13]. The completeness of the KCCR data has been estimated to be over 96% for malignant tumors [14].
Data on PSCATs from 2006 to 2010, including malignant and non-malignant cases, were identified in the KNCIDB. The basic information available included the demographic characteristics of each patient, date of diagnosis, primary site, and histological type of the tumor according to the International Classification of Diseases for Oncology, 3rd edition (ICDO- 3) [15]. The ICD-O-3, which contains topography codes and morphology codes, was developed by the World Health Organization (WHO) and International Agency for Research on Cancer (IARC) for use in cancer registries, pathology, and other departments specializing in cancer [15].
Primary tumors with the following ICD-O-3 site codes were included in the analysis: C70.1 (spinal meninges), C72.0 (spinal cord), and C72.1 (cauda equina). For histological type, we used histology categories used in Duong et al.’s report (Appendix 1) [5].
1. Statistical analysis
Frequencies according to demographic and tumor characteristics for all PSCATs were calculated. Age-standardized incidence rates with 95% confidence intervals for all PSCATs were calculated overall as well as by tumor behavior, gender, histology, and year of diagnosis. Rates were expressed per 100,000 persons and were age-standardized according to the world standard population [16]. Male-to-female rate ratios were calculated by dividing the age-standardized incidence rates for males by those for females.
Results
Table 1 shows the characteristics of PSCATs diagnosed from 2006 to 2010. Of 3,312 PSCATs cases, 443 (13.4%) were malignant and 2,869 (86.6%) were non-malignant.
Table 1.
Characteristics of primary spinal cord and appendage tumors in Korea between 2006 and 2010
| Characteristic | Total |
Malignant |
Non-malignant |
|||
|---|---|---|---|---|---|---|
| No. (%) | Ratea) (95% CI) | No. (%) | Ratea) (95% CI) | No. (%) | Ratea) (95% CI) | |
| Total | 3,312 (100) | 1.08 (1.04-1.12) | 443 (100) | 0.16 (0.14-0.18) | 2,869 (100) | 0.92 (0.89-0.96) |
| Age at diagnosis (yr) | ||||||
| 0-9 | 53 (1.6) | 0.20 | 25 (5.6) | 0.10 | 28 (1.0) | 0.11 |
| 10-19 | 125 (3.8) | 0.37 | 32 (7.2) | 0.09 | 93 (3.2) | 0.27 |
| 20-29 | 243 (7.3) | 0.67 | 50 (11.3) | 0.14 | 193 (6.7) | 0.53 |
| 30-39 | 461 (13.9) | 1.08 | 82 (18.5) | 0.19 | 379 (13.2) | 0.89 |
| 40-49 | 721 (21.8) | 1.68 | 78 (17.6) | 0.18 | 643 (22.4) | 1.5 |
| 50-59 | 741 (22.4) | 2.46 | 84 (19.0) | 0.28 | 657 (22.9) | 2.18 |
| 60-69 | 591 (17.8) | 3.03 | 52 (11.7) | 0.27 | 539 (18.8) | 2.76 |
| 70-79 | 314 (9.5) | 2.76 | 26 (5.9) | 0.23 | 288 (10.0) | 2.53 |
| ≥ 80 | 63 (1.9) | 1.59 | 14 (3.2) | 0.35 | 49 (1.7) | 1.24 |
| Gender | ||||||
| Male | 1,477 (44.6) | 0.99 (0.94-1.04) | 265 (59.8) | 0.19 (0.17-0.22) | 1,212 (42.2) | 0.80 (0.75-0.85) |
| Female | 1,835 (55.4) | 1.15 (1.10-1.21) | 178 (40.2) | 0.13 (0.11-0.15) | 1,657 (57.8) | 1.02 (0.97-1.08) |
| Primary site (ICD-O-3 site code) | ||||||
| Spinal meninges (C70.1) | 532 (16.1) | 0.16 (0.15-0.18) | 12 (2.7) | 0.00 (0.00-0.01) | 520 (18.1) | 0.16 (0.15-0.17) |
| Spinal cord (C72.0) | 2,763 (83.4) | 0.91 (0.88- 0.95) | 430 (97.1) | 0.15 (0.14-0.17) | 2,333 (81.3) | 0.76 (0.72-0.79) |
| Cauda equina (C72.1) | 17 (0.5) | 0.01 (0.00-0.01) | 1 (0.2) | 0.00 (0.00-0.00) | 16 (0.6) | 0.01 (0.00-0.01) |
| Histology | ||||||
| Ependymoma | 253 (7.6) | 0.09 (0.07-0.10) | 183 (41.3) | 0.06 (0.05-0.07) | 70 (2.4) | 0.03 (0.02-0.03) |
| Pilocytic astrocytic tumors | 21 (0.6) | 0.01 (0.01-0.02) | 2 (0.5) | 0.00 (0.00-0.00) | 19 (0.7) | 0.01 (0.00-0.01) |
| Other astrocytoma | 59 (1.8) | 0.02 (0.02-0.03) | 52 (11.7) | 0.02 (0.02-0.03) | 7 (0.2) | 0.00 (0.00-0.00) |
| Tumors of the spinal nerves | 1,486 (44.9) | 0.47 (0.45-0.50) | 21 (4.7) | 0.01 (0.00-0.01) | 1,465 (51.1) | 0.47 (0.44-0.49) |
| Neurofibroma, NOS | 69 (2.1) | 0.03 (0.02-0.03) | - | - | 69 (2.4) | 0.03 (0.02-0.03) |
| Neurofibromatosis, NOS | 14 (0.4) | 0.01 (0.00-0.01) | - | - | 14 (0.5) | 0.01 (0.00-0.01) |
| Malignant peripheral nerve sheath tumor | 6 (0.2) | 0.00 (0.00-0.00) | 6 (1.4) | 0.00 (0.00-0.00) | - | - |
| Plexiform neurofibroma | 7 (0.2) | 0.00 (0.00-0.01) | - | - | 7 (0.2) | 0.00 (0.00-0.01) |
| Neurilemoma, NOS | 1,369 (41.3) | 0.43 (0.41-0.45) | - | - | 1,369 (47.7) | 0.43 (0.41-0.45) |
| Neurilemoma malignant | 15 (0.5) | 0.00 (0.00-0.01) | 15 (3.4) | 0.00 (0.00-0.01) | - | - |
| Others | 6 (0.2) | 0.00 (0.00-0.00) | - | - | 6 (0.2) | 0.00 (0.00-0.00) |
| Meningioma | 665 (20.1) | 0.20 (0.19-0.22) | 4 (0.9) | 0.00 (0.00-0.00) | 661 (23.0) | 0.20 (0.19-0.22) |
| Hemangioblastoma | 75 (2.3) | 0.03 (0.02-0.03) | 0 | - | 75 (2.6) | 0.03 (0.02-0.03) |
| Other mesenchymal tumors | 56 (1.7) | 0.02 (0.01-0.02) | 5 (1.1) | 0.00 (0.00-0.01) | 51 (1.8) | 0.02 (0.01-0.02) |
| Lymphomas | 26 (0.8) | 0.01 (0.01-0.01) | 26 (5.9) | 0.01 (0.01-0.01) | - | - |
| Other tumors | 92 (2.8) | 0.04 (0.03-0.05) | 45 (10.2) | 0.02 (0.01-0.03) | 47 (1.6) | 0.02 (0.01-0.03) |
| Unclassified tumors | 579 (17.5) | 0.19 (0.17-0.21) | 105 (23.7) | 0.04 (0.03-0.04) | 474 (16.5) | 0.15 (0.14-0.17) |
| Year of diagnosis | ||||||
| 2006 | 540 (16.3) | 0.92 (0.84-1.00) | 87 (19.6) | 0.16 (0.13-0.20) | 453 (15.8) | 0.76 (0.68-0.83) |
| 2007 | 584 (17.6) | 0.97 (0.89-1.05) | 95 (21.4) | 0.17 (0.13-0.20) | 489 (17.0) | 0.81 (0.73-0.88) |
| 2008 | 679 (20.5) | 1.11 (1.02-1.19) | 89 (20.1) | 0.16 (0.12-0.19) | 590 (20.6) | 0.95 (0.87-1.03) |
| 2009 | 688 (20.8) | 1.10 (1.02-1.19) | 83 (18.7) | 0.15 (0.12-0.19) | 605 (21.1) | 0.95 (0.88-1.03) |
| 2010 | 821 (24.8) | 1.28 (1.19-1.38) | 89 (20.1) | 0.16 (0.12-0.20) | 732 (25.5) | 1.13 (1.04-1.21) |
CI, confidence interval; ICD-O-3, International Classification of Diseases for Oncology, third edition; NOS, not otherwise specified.
Rates are per 100,000 persons and age-adjusted to the world standard population, except age-specific rates, which were not age-adjusted.
The age-standardized incidence rate for non-malignant primary spinal tumors was 0.92 per 100,000 and 0.16 per 100,000 for malignant tumors. Age-specific incidence rate for all PSCATs was lowest in the age range from 0 to 9 years (0.20 per 100,000) and was highest in adults aged 60 to 69 years (3.03 per 100,000). Age-specific rates gradually increased with advancing age, peaked from 60 to 69 years, and declined thereafter among non-malignant PSCATs. However, for malignant PSCATs, rates peaked in patients over 80 years of age. Childhood tumors were more likely to be malignant. Malignant tumors were more frequent in men (59.8%), whereas non-malignant tumors were more frequently found in women (57.8%). The spinal cord was the most frequent site (83.4%), followed by the spinal meninges (16.1%) and cauda equina (0.5%).
The most common histological type was neurilemomas (41.3%), followed by meningiomas (20.1%), and ependymomas (7.6%). Ependymomas were the most common histological type among malignant tumors (41.3%). Neurilemomas accounted for 47.7% of non-malignant tumors.
Table 2 shows incidence rates of PSCATs by primary site and histology. Meningioma had the highest incidence among the spinal meninges (91.2%). Among tumors in the spinal cord, neurilemomas were the most common (49.3%, 0.43 per 100,000), followed by ependymomas and meningiomas.
Table 2.
Incidence rates of primary spinal cord and appendage tumors by primary site and histology in Korea, 2006-2010
| Characteristic | Spinal meninges (C70.1) |
Spinal cord (C72.0) |
Cauda equina (C72.1) |
|||
|---|---|---|---|---|---|---|
| No. (%) | Ratea) | No. (%) | Ratea) | No. (%) | Ratea) | |
| Ependymoma | 2 (0.4) | 0.00 | 250 (9.0) | 0.08 | 1 (5.9) | 0.00 |
| Pilocytic astrocytic tumors | - | - | 21 (0.8) | 0.01 | - | - |
| Other astrocytoma | 1 (0.2) | 0.00 | 58 (2.1) | 0.02 | - | - |
| Tumors of spinal nerves | - | - | 1,480 (53.6) | 0.47 | 6 (35.3) | 0.00 |
| Neurofibroma, NOS | - | - | 69 (2.5) | 0.03 | - | - |
| Neurofibromatosis, NOS | - | - | 14 (0.5) | 0.01 | - | - |
| Malignant peripheral nerve sheath tumor | - | - | 6 (0.2) | 0.00 | - | - |
| Plexiform neurofibroma | - | - | 7 (0.3) | 0.00 | - | - |
| Neurilemoma, NOS | - | - | 1,363 (49.3) | 0.43 | 6 (35.3) | 0.00 |
| Neurilemoma malignant | - | - | 15 (0.5) | 0.00 | - | - |
| Others | - | - | 6 (0.2) | 0.00 | - | - |
| Meningioma | 485 (91.2) | 0.15 | 177 (6.4) | 0.05 | 3 (17.6) | 0.00 |
| Hemangioblastoma | 1 (0.2) | 0.00 | 73 (2.6) | 0.02 | 1 (5.9) | 0.00 |
| Other mesenchymal tumors | 6 (1.1) | 0.00 | 49 (1.8) | 0.02 | 1 (5.9) | 0.00 |
| Lymphomas | 1 (0.2) | 0.00 | 25 (0.9) | 0.01 | - | - |
| Other tumors | 3 (0.6) | 0.00 | 89 (3.2) | 0.04 | - | - |
| Unclassified tumors | 33 (6.2) | 0.01 | 541 (19.6) | 0.18 | 5 (29.4) | 0.00 |
NOS, not otherwise specified.
Age-adjusted rate per 100,000 to the world standard population.
Table 3 shows age-adjusted rate by sex and histological type, along with male-to-female age-adjusted rate ratios. Men showed at least 3-fold higher incidence rate of lymphomas compared to women (male:female rate ratio, 3.20). For ependymomas, men showed statistically higher rates than women (male:female rate ratio, 1.35). Conversely, women showed at least 4-fold higher rates for meningiomas (male:female rate ratio, 0.27).
Table 3.
Malignant and non-malignant primary spinal cord and appendage tumor male-to-female rate ratios by histology type in Korea between 2006 and 2010
| Histology | Total |
Male |
Female |
Male-to-female rate ratio (95% CI) | |||
|---|---|---|---|---|---|---|---|
| No. (%) | Ratea) | No. (%) | Ratea) | No. (%) | Ratea) | ||
| Ependymoma | 253 (7.6) | 0.09 | 143 (9.7) | 0.10 | 110 (6.0) | 0.07 | 1.35 (1.04-1.75) |
| Pilocytic astrocytic tumors | 21 (0.6) | 0.01 | 11 (0.7) | 0.01 | 10 (0.5) | 0.01 | 1.26 (0.49-3.22) |
| Other astrocytoma | 59 (1.8) | 0.02 | 33 (2.2) | 0.02 | 26 (1.4) | 0.02 | 1.05 (0.61-1.81) |
| Tumors of spinal nerves | 1,486 (44.9) | 0.47 | 744 (50.4) | 0.48 | 742 (40.4) | 0.46 | 1.04 (0.94-1.16) |
| Neurofibroma, NOS | 69 (2.1) | 0.03 | 40 (2.7) | 0.03 | 29 (1.6) | 0.02 | 1.42 (0.87-2.34) |
| Neurofibromatosis, NOS | 14 (0.4) | 0.01 | 8 (0.5) | 0.01 | 6 (0.3) | 0.00 | 1.49 (0.50-4.46) |
| Malignant peripheral nerve sheath tumor | 6 (0.2) | 0.00 | 4 (0.3) | 0.00 | 2 (0.1) | 0.00 | 2.29 (0.42-12.57) |
| Plexiform neurofibroma | 7 (0.2) | 0.00 | 5 (0.3) | 0.01 | 2 (0.1) | 0.00 | 2.43 (0.44-13.45) |
| Neurilemoma, NOS | 1,369 (41.3) | 0.43 | 674 (45.6) | 0.43 | 695 (37.9) | 0.43 | 1.00 (0.90-1.11) |
| Neurilemoma malignant | 15 (0.5) | 0.00 | 9 (0.6) | 0.01 | 6 (0.3) | 0.00 | 1.65 (0.58-4.72) |
| Others | 6 (0.2) | 0.00 | 4 (0.3) | 0.00 | 2 (0.1) | 0.00 | 3.50 (0.54-22.59) |
| Meningioma | 665 (20.1) | 0.20 | 126 (8.5) | 0.08 | 539 (29.4) | 0.31 | 0.27 (0.23-0.32) |
| Hemangioblastoma | 75 (2.3) | 0.03 | 47 (3.2) | 0.03 | 28 (1.5) | 0.02 | 1.59 (0.99-2.56) |
| Other mesenchymal tumors | 56 (1.7) | 0.02 | 31 (2.1) | 0.02 | 25 (1.4) | 0.02 | 1.23 (0.69-2.18) |
| Lymphomas | 26 (0.8) | 0.01 | 18 (1.2) | 0.02 | 8 (0.4) | 0.00 | 3.20 (1.28-8.02) |
| Other tumors | 92 (2.8) | 0.04 | 46 (3.1) | 0.04 | 46 (2.5) | 0.05 | 0.78 (0.49-1.23) |
| Unclassified tumors | 579 (17.5) | 0.19 | 278 (18.8) | 0.19 | 301 (16.4) | 0.19 | 1.01 (0.85-1.19) |
CI, confidence interval; NOS, not otherwise specified.
Age-adjusted rate per 100,000 to the world standard population.
Fig. 1 shows incidence rates of PSCATs by primary site and sex. Women showed 3-fold higher incidence rates of tumors of the spinal meninges. For tumors of the spinal cord, men showed slightly higher incidence rates than women.
Fig. 1.
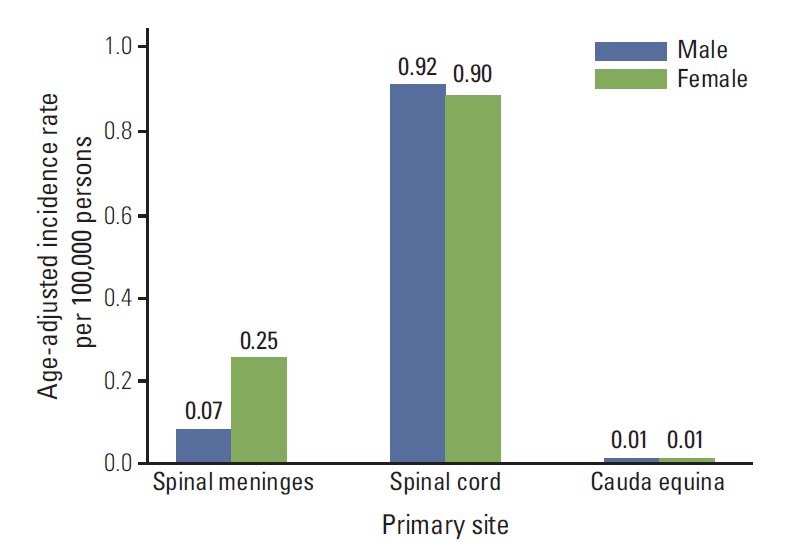
Primary spinal cord and appendage tumor incidence rates by primary site and gender in Korea between 2006 and 2010.
Discussion
To our knowledge, this is the first Asian epidemiologic report on PSCATs based on a nationwide population-based registry in Korea.
The incidence of PSCATs in our study (1.08 per 100,000 persons) was slightly higher than that observed in the United States (0.97 per 100,000 persons) [5] or Estonia (0.80 per 100,000 persons) [3], whereas it was slightly lower than that found in France (1.20 per 100,000 persons) [2] or Croatia (1.60 per 100,000 persons) [10].
In our study, the most common site of PSCATs was the spinal cord (83.4%), followed by spinal meninges (16.1%) and cauda equina (0.5%). The spinal cord was more frequently cited as a tumor location in our study compared with studies in Western countries [10]. Studies in the United States reported the same order, whereas frequency of tumors of the spinal cord was less than that in Korea (60%-70%) [4,5]. However, a study in Norway reported similar tumor rates in the spinal cord and spinal meninges, and a study in Croatia reported that the spinal meninges is the most common site with a rate of over 50% [3]. These differences may reflect population differences and small sample sizes.
We also found that the most common histological type of PSCATs was neurilemomas (41.3%), followed by meningiomas (20.1%) and ependymomas (7.6%). Schellinger et al. [4] reported that the most common histological types in the United States are meningiomas (29%), nerve sheath tumors (24%), and ependymomas (23%), which supports the results of Duong et al. [5]. With regard to sex differences, we found that the overall incidence rate among men was 0.99 per 100,000 persons while women had an incidence rate of 1.15 per 100,000 persons, which is similar to incidence rates in the United States [4,5], although the difference in incidence rates between men and women was greater in our study.
Age-specific incidence patterns differ between malignant and non-malignant PSCATs. For non-malignant PSCATs, rates peaked from 60 to 69 years of age and declined thereafter. However, for malignant PSCATs, rates gradually increased with age. These patterns also were found Estonia and the United States [3,5]. We found that 32% of tumors childhood (age, 0 to 19 years) PSCATs were malignant, whereas only 13.4% were malignant in adults. In the United States, more than half of all childhood tumors have been shown to be malignant [5].
However, we should interpret the results of the present study with caution. Firstly, there may be variability in completeness of the data on non-malignant tumors with time, as the accuracy of the data may have improved during study period. Especially, in January 2005, the KCCR began collecting data on non-malignant primary brain and CNS tumors, including PSCATs. When we analyzed trends in non-malignant primary brain and CNS tumors, we found that incidence rates in 2006 were relatively low compared to following years. Secondly, it should be noted that the frequency of unclassified tumors was found to be relatively high (17.5%) compared with that of the United States (4.6%) [5]. Therefore, the real incidence of each histological subtype would be higher than that reported in this study, particularly for malignant tumors (23.7%). This may be due to the fact that many PSCAT patients are diagnosed using imaging modalities without surgery or biopsy in non-operated or inoperable cases.
Conclusion
This is the first population-based study in Korea to present a descriptive epidemiology of PSCATs. Our study found that 86.6% of PSCATs were non-malignant, and the most common site was the spinal cord (83.4%). Childhood tumors were more likely to be malignant than adult tumors. The common histological types were neurilemomas, meningiomas, and ependymomas.
Acknowledgments
This work was supported by a research grant from the National Cancer Center (No. 1310220).
Appendix 1. Histology codes for primary spinal cord and appendage tumors
| Primary spinal cord and appendage tumors (histology definitions) | ICD-O-3 codes |
|---|---|
| Tumors of neuroepithelial tissue | |
| Ependymoma | 9391, 9392, 9393, 9394 |
| Pilocytic astrocytoma | 9421 |
| Other astrocytic tumors | 9410, 9420, 9401, 9411, 9383, 9384, 9424, 9400, 9440, 9441, 9442/3 |
| Tumors of spinal nerves | 9540, 9541, 9550, 9560, 9561, 9570, 9571, 9562 |
| Neurofibroma, NOS | 9540/0 |
| Neurofibromatosis, NOS | 9540/1 |
| Malignant peripheral nerve sheath tumor | 9540/3 |
| Plexiform neurofibroma | 9550/0 |
| Neurilemmoma, NOS | 9560/0 |
| Neurilemmoma malignant | 9560/3 |
| Others | 9541, 9560/1, 9562, 9570, 9571 |
| Tumors of meninges | |
| Meningioma | 9530, 9531, 9532, 9533, 9534, 9537, 9538, 9539 |
| Hemangioblastoma | 9161, 9535 |
| Other mesenchymal | 8324, 8728, 8800, 8801, 8802, 8803, 8804, 8805, 8806, 8810, 8815, 8824, 8830, 8831, 8850, 8851, 8852, 8854, 8857, 8861, 8870, 8890, 8897, 8900, 8910, 8920, 8990, 9040, 9150, 9170, 9180, 9210, 9241, 9260, 9480, 9536 |
| Lymphomas | 9590, 9591, 9596, 9650, 9651, 9652, 9653, 9654, 9655, 9659, 9661, 9662, 9663, 9664, 9665, 9667, 9670, 9671, 9673, 9675, 9680, 9684, 9687, 9690, 9691, 9695, 9698, 9699, 9701, 9702, 9705, 9714, 9719, 9727, 9728, 9729, 9731, 9733, 9734, 9740, 9741, 9750, 9755, 9756, 9757, 9758, 9766, 9826, 9827, 9860, 9861, 9930, 9970 |
| Othersa) | 8680, 8693, 8711, 8963, 9064, 9070, 9071, 9080, 9084, 9085, 9220, 9231, 9240, 9364, 9370, 9371, 9380, 9382, 9390, 9412, 9413, 9430, 9450, 9451, 9470, 9473, 9490, 9492, 9500, 9501, 9503, 9505, 9506, 9508 |
| Unclassified tumors | 9120, 9121, 9122, 9123, 9125, 9130, 9131, 9133, 9140, 8000, 8001, 8002, 8003, 8004, 8005, 8010, 8013, 8021, 8452, 8683, 8720, 8811, 8840, 8860, 8896, 8980, 9173, 9580, 9751, 9752, 9753, 9754, 9823, 9837, 9866 |
ICD-O-3, International Classification of Diseases for Oncology, 3rd ed.
Others includes neuronal/glial, nonmalignant and malignant, chordoma/chondrosarcoma, embryonal/primitive/medulloblastoma, germ cell tumors and cysts, glioma malignant, not otherwise specified (NOS), mixed glioma, choroid plexus, oligodendroglioma, and anaplastic oligodendroglioma.
Footnotes
Conflict of interest relevant to this article was not reported.
References
- 1.Engelhard HH, Villano JL, Porter KR, Stewart AK, Barua M, Barker FG, et al. Clinical presentation, histology, and treatment in 430 patients with primary tumors of the spinal cord, spinal meninges, or cauda equina. J Neurosurg Spine. 2010;13:67–77. doi: 10.3171/2010.3.SPINE09430. [DOI] [PubMed] [Google Scholar]
- 2.Elia-pasquet S, Provost D, Jaffre A, Loiseau H, Vital A, Kantor G, Et Al. Incidence Of Central Nervous System Tumors In Gironde, France. Neuroepidemiology. 2004;23:110–7. doi: 10.1159/000075953. [DOI] [PubMed] [Google Scholar]
- 3.Liigant A, Asser T, Kulla A, Kaasik AE. Epidemiology of primary central nervous system tumors in Estonia. Neuroepidemiology. 2000;19:300–11. doi: 10.1159/000026269. [DOI] [PubMed] [Google Scholar]
- 4.Schellinger KA, Propp JM, Villano JL, McCarthy BJ. Descriptive epidemiology of primary spinal cord tumors. J Neurooncol. 2008;87:173–9. doi: 10.1007/s11060-007-9507-z. [DOI] [PubMed] [Google Scholar]
- 5.Duong LM, McCarthy BJ, McLendon RE, Dolecek TA, Kruchko C, Douglas LL, et al. Descriptive epidemiology of malignant and nonmalignant primary spinal cord, spinal meninges, and cauda equina tumors, United States, 2004-2007. Cancer. 2012;118:4220–7. doi: 10.1002/cncr.27390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Central Brain Tumor Registry of the United States . CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2004-2007. Hinsdale: Central Brain Tumor Registry of the United States; 2011. [Google Scholar]
- 7.Davis FG, Freels S, Grutsch J, Barlas S, Brem S. Survival rates in patients with primary malignant brain tumors stratified by patient age and tumor histological type: an analysis based on Surveillance, Epidemiology, and End Results (SEER) data, 1973-1991. J Neurosurg. 1998;88:1–10. doi: 10.3171/jns.1998.88.1.0001. [DOI] [PubMed] [Google Scholar]
- 8.Surawicz TS, McCarthy BJ, Kupelian V, Jukich PJ, Bruner JM, Davis FG. Descriptive epidemiology of primary brain and CNS tumors: results from the Central Brain Tumor Registry of the United States, 1990-1994. Neuro Oncol. 1999;1:14–25. doi: 10.1093/neuonc/1.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johannesen TB, Angell-Andersen E, Tretli S, Langmark F, Lote K. Trends in incidence of brain and central nervous system tumors in Norway, 1970-1999. Neuroepidemiology. 2004;23:101–9. doi: 10.1159/000075952. [DOI] [PubMed] [Google Scholar]
- 10.Materljan E, Materljan B, Sepcic J, Tuskan-Mohar L, Zamolo G, Erman-Baldini I. Epidemiology of central nervous system tumors in Labin area, Croatia, 1974-2001. Croat Med J. 2004;45:206–12. [PubMed] [Google Scholar]
- 11.Shin HR, Won YJ, Jung KW, Kong HJ, Yim SH, Lee JK, et al. Nationwide cancer incidence in Korea, 1999~2001; first result using the national cancer incidence database. Cancer Res Treat. 2005;37:325–31. doi: 10.4143/crt.2005.37.6.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee CH, Jung KW, Yoo H, Park S, Lee SH. Epidemiology of primary brain and central nervous system tumors in Korea. J Korean Neurosurg Soc. 2010;48:145–52. doi: 10.3340/jkns.2010.48.2.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Curado MP, Edwards B, Shin HR, Storm H, Ferlay J, Heanue M, et al. Cancer incidence in five continents. Lyon: International Agency for Research on Cancer; 2008. [Google Scholar]
- 14.Jung KW, Park S, Kong HJ, Won YJ, Lee JY, Park EC, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2008. Cancer Res Treat. 2011;43:1–11. doi: 10.4143/crt.2011.43.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fritz A, Percy C, Jack A, Shanmugaratnam K, Sobin L, Parkin DM, et al. International classification of diseases for oncology. 3rd ed. Geneva: World Health Organization; 2000. [Google Scholar]
- 16.Segi M. Cancer mortality for selected sites in 24 countries (1950-1957) Sendai: Department of Public Health, Tohoku University School of Medicine; 1960. [Google Scholar]


