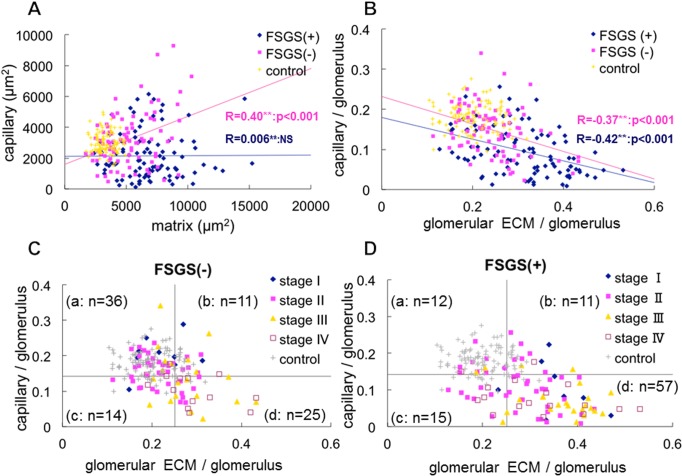
Fig 6. The relationship between the areas of glomerular capillaries and glomerular ECM in glomerular cross section in idiopathic membranous nephropathy (MN) by computer-assessed morphometric analysis.
(A) The areas (μm2) of glomerular capillaries (X-axis) and ECM (Y-axis) were measured in MN-FSGS(+) cases (blue rhombus), MN-FSGS(−) cases (red square), and minor glomerular abnormalities in control (yellow x). In MN cases with or without FSGS lesion, increase of glomerular capillary area and/or glomerular ECM area was evident, suggesting the development of glomerular hypertrophy. In MN-FSGS(−) cases, the area of capillaries was positively correlated with the area of ECM in glomeruli. In contrast, there was no correlation between the areas of capillaries and ECM in glomeruli in MN-FSGS(+), suggesting the development of decrease of glomerular capillary area with increase of ECM area in enlarged glomeruli. (B) To avoid the effects of the variation in the size of glomeruli, the areas of glomerular capillaries and ECM in glomeruli were adjusted by using the area of glomerular capillaries / the area of glomerular tuft, and the area of glomerular ECM / the area of glomerular tuft. Regardless of the presence or absence of FSGS lesion, the areas of glomerular capillaries and ECM were negatively correlated, indicating that the narrowing and decrease of glomerular capillaries was associated with the accumulation of ECM. (C, D) We examined the areas of glomerular capillaries and ECM in glomeruli in each stage of MN (stage I to IV) in cases without FSGS lesion (C, FSGS −) and with FSGS lesion (D, FSGS +). The horizontal boundary is set at the average of glomerular capillary area of all glomeruli in control and MN cases with and without FSGS lesion. The longitudinal boundary is set at the average of glomerular ECM area of all glomeruli in control and MN cases with and without FSGS lesion. In accordance with the setting the boundary for the average of the areas of glomerular capillaries and glomerular ECM, all glomeruli were divided into 4 categories; a: large capillary area with minimal accumulation of ECM, b: large capillary area with marked accumulation of ECM, c: decrease of glomerular capillary area with minimal accumulation of ECM, and d: decrease of glomerular capillary area with marked accumulation of ECM. (n = number) is the number of cases of MN with and without FSGS lesion in each category. In MN-FSGS(−) cases (C), many cases, especially stage I and stage II, were present in category a (36/86: 41.9%). In contrast, the most common category in MN-FSGS(+) cases (D), was d (57/95: 60.0%), and many cases of stage III (18/24: 75.0%) and IV (11/17:64.7%) fell into this category. These findings indicate that the decrease of glomerular capillaries with increase of glomerular ECM area was more prominent in MN-FSGS(+) than those in MN-FSGS(−) cases.