Abstract
Objectives: The objective of this study was to radiographically quantify bone height and bone density in patients with periodontitis after fixed orthodontic treatment using cone beam computed tomography (CBCT). Materials and methods: A total of 81 patients including 40 patients with chronic periodontitis (group 1) and 41 patients with normal periodontal tissues (group 2) were selected. CBCT scanning for anterior teeth were taken before and after orthodontic treatment. Measurements of bone height and bone density were performed using CBCT software. Results: The group 1 presented a statistically lesser bone density and bone height when compared to group 2 before treatment. There was a significant loss of bone density for both groups after orthodontic treatment, but bone density loss was significantly greater in the group 1. There was no statistically significant bone height change in two groups after treatment. Conclusions: This study demonstrated that orthodontic treatment can preserve bone height but not capable of maintaining bone density, especially for patients with periodontitis. It is indicated that the change of bone density may be more susceptible than that of bone height when radiographically evaluating bone status under this combined periodontal and orthodontic therapy.
Keywords: CBCT, alveolar bone density, alveolar height, periodontal disease, tooth movement
Introduction
Periodontitis is characterized by inflammation of the supporting tissues of the teeth, resulting in resorption of the alveolar bone as well as loss of the soft tissue attachment to the tooth. It has been reported that over 30% of the adult population suffer from chronic periodontitis in a Chinese population [1]. In adult periodontal patients, pathologic tooth migration can create serious functional and aesthetic problems. Periodontitis-related patients often suffer a lot of complications, including tipping, drifting or extrusion of one or several incisors, the occurrence of gaps between anterior teeth and occlusal interference that may lead to destructive periodontal disease [2,3]. A traumatic occlusion and pathologic dentition could not always be improved by periodontal treatment alone. Orthodontic treatment can achieve satisfactory outcomes from esthetic, occlusal, and functional standpoints when periodontal inflammation is well controlled [4]. A combined periodontal-orthodontic therapy has been considered one of the most ideal treatment options at present [5].
Nevertheless, clinicians are often faced with the challenge of moving periodontally compromised teeth. Bone loss alters the position of the center of resistance to teeth [6] and consequently traditional orthodontic treatment may be at high risk, especially for intrusion and tipping. It is necessary to pay special attention to alveolar bone status of patients who are more likely to be susceptible to periodontal disease, and to control existing disease, before starting overall orthodontic treatment.
For patients with periodontitis, it has been observed clinically that tooth mobility remarkably increases once treatment begins, even if the inflammation and orthodontic forces are strictly controlled. It is known that orthodontic movement require healthy and adequate bone. Bone density and height are two of the most useful parameters in the evaluation of bone status [7,8]. It is likely that the quantitative measurement of bone density and bone height may have a clearer understanding of the combination of periodontal-orthodontic therapy. However, the relationship of bone density and periodontal disease has been reported in a limited number of studies. The use of CBCT has been shown the advantage of undistorted visualization of the alveolar crest on a life-size scale and high geometric measurements for assessing bone volume [9,10]. The aim of this study was to radiographically quantify bone density and bone height in periodontally compromised patients, as compared with patients of normal periodontal support, who all underwent fixed orthodontic treatment.
Patients and methods
Patients
A total of 81 cases were selected in the department of Craniofacial Orthodontics or Periodontology of Shanghai’s Ninth People’s Hospital. Patients suffering from apical cysts, supernumerary teeth, root resorption or crown-root angulation by CBCT, and systemic risk factors for periodontal diseases like diabetes, osteoporosis, and immunological disorders were excluded from the study. This study was approved by the ethics committee of the Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine. All participants signed an informed consent agreement. Two different groups were included in our study.
Group 1
The group 1 as the test group consisted of 40 subjects with chronic periodontitis. There were 11 men and 29 women, mean age 34.4 years (range 18-39 years). All patients had integral dentition with deep overjet, severe anterior extrusion, a class II molar relationship. Inflammation was controlled before orthodontic treatment. Follow up consisted of maintenance periodontal therapy every 3 months and routine orthodontic appointments with a one-month interval.
Group 2
The group 2 included 41 subjects (13 males, 28 females) with a class II malocclusion as the control group, which had healthy periodontal tissue. The mean age was 29.3 years (range 20-37 years). Subjects in this group were matched with the group 1 for the degree of malocclusion and age.
Oral hygiene was emphasized during the active orthodontic treatment. An MBT pre-adjusted bracket system with a slot size of 0.022 (3M Unitek, Calif) was applied.
CBCT examinations
Before and after orthodontic treatment, CBCT images (3D, Multi-Image Morita Micro CT) were obtained from the upper and lower anterior region to evaluate bone density and height bone. CBCT scan was carried out by a single technician and operated at 80 kV and 5 mA with a height of 30 mm, width of 40 mm. When the CBCT was used for imaging, the mean skin dose was 0.026 mSv per examination. Multiplanar reconstructions from the DICOM (Digital Imaging and Communications in Medicine) data were made. Image slices were oriented through axial, coronal, and sagittal views of the 3D head rendering in any direction. Using cephalometric projection, the developed technique for calculating bone density and bone height are shown and described as follows:
Step 1: Sagittal section: Adjusting the long axis of the middle incisor to the vertical line (Figure 1A, 1B); Step 2: Transverse section: Positioning the cemento-enamel junction in the axial view. Locating the line connected with pulp cavity centers of adjacent incisors to the horizon level (Figure 1C). Step 3: Coronal section: Consequently, the longest and repeated images of the interalveolar septum could be obtained and repeating steps for other interalveolar septums (Figure 1D).
Figure 1.
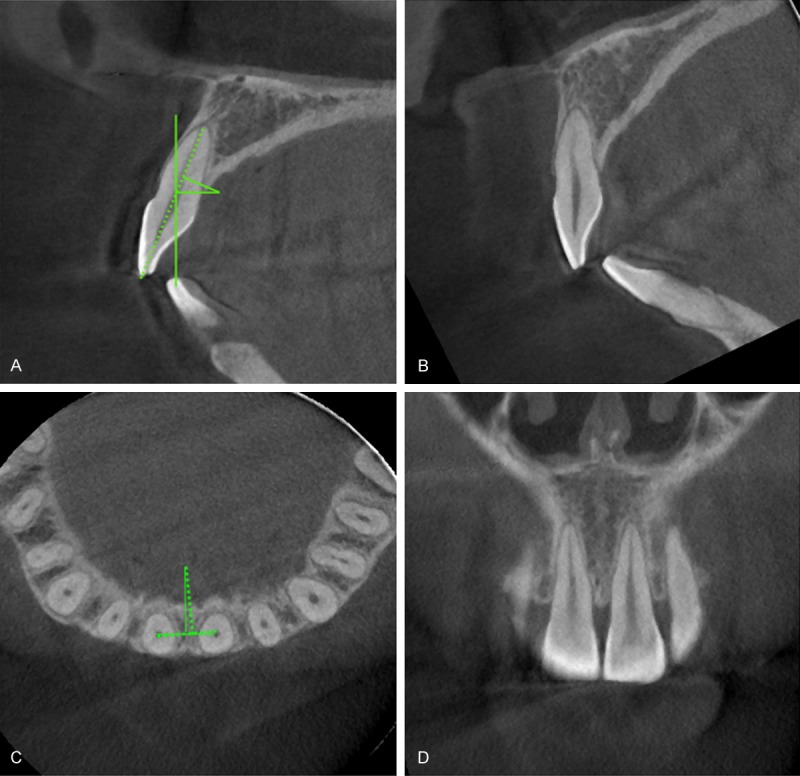
The process for landmark location in the 3D images is as follows: A. Adjusting the long axis of the middle incisor to the vertical line. B. Locating the CEJ of the incisor in a sagittal slice. C. Rotating a line connected with adjacent incisors to the horizon level in an axial view. D. The largest selected image of the incisors in the coronal view.
The coronal, middle, and apical area of the interalveolar septum were selected to measure bone density (Figure 2A). Bone density of the anterior area was evaluated through densitometry variations of grayscale, which varied from 0 to 255 (transparent to opaque) (Figure 2B). Alveolar bone height extending from the apex to the alveolar crest was measured in millimeters (Figure 3).
Figure 2.
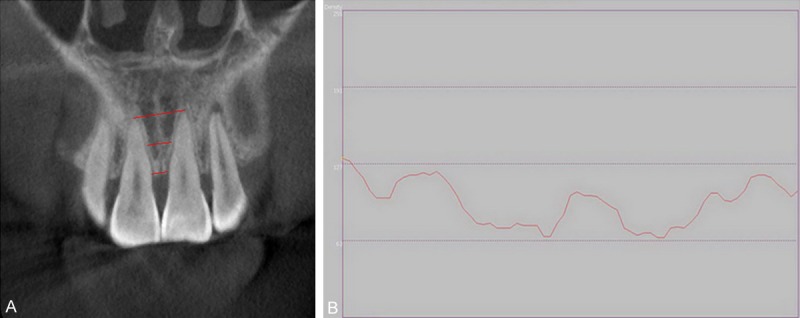
Bone density measurement. A. Evaluations of alveolar bone density at the coronal, midroot and root apex levels of the interalveolar septum are performed. B. A curve of density value which is expressed as gray scale is obtained in the computer.
Figure 3.
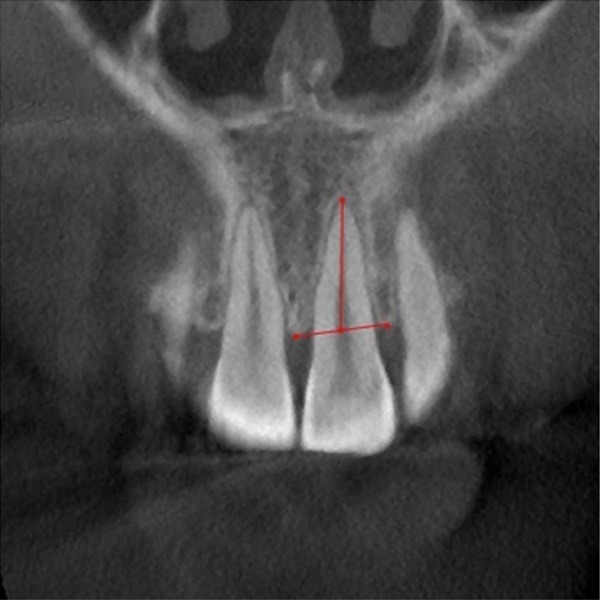
The alveolar height is the distance between the root apex and the middle point of the line connecting the mesial and distal alveolar crest.
Statistical analysis
Consistency of morphometric measurements was evaluated in a 20% (16 of 81) random sample of imaging by blindly repeating measures twice. To assess measurement accuracy, intraclass correlation coefficient (ICC) was used. The level of reliability was ICC value > 0.75, and it was found between 0.93 and 0.97 in our study. The Paired-T-Test was used for self-control comparisons and the Independent-Samples T Test for inter-group assessment. All statistical analyses were performed using statistical Package for the Social Sciences, version 16 (SPSS, Chicago, IL) and a P-value less than 0.05 was considered statistically significant.
Results
Clinical characteristics of the subjects
The descriptive statistics was shown in Table 1 and there were no significant differences in sex, age, and treatment duration between the two groups at baseline (P > 0.05). The mean treatment duration was 26.3 months (range 20-33 months) and 22.6 months (range 18-27 months) for the group 1 and group 2, respectively.
Table 1.
Descriptive statistics and comparisons for the differences between the two groups (mean ± SD)
| Group 1 | Group 2 | P | |
|---|---|---|---|
| Case | 40 | 41 | 1.00 |
| Sex (M/F) | 11/29 | 13/28 | 1.00 |
| Mean age (Y) | 34.4 ± 12.1 | 29.3 ± 10.8 | 0.68 |
| Duration (M) | 26.3 ± 3.4 | 22.6 ± 4.7 | 0.54 |
Change of bone density
In group 1, the alveolar density decreased significantly from 129.62 to 99.53, while in group 2, the density decreased from 148.93 to 135.97. The group 1 presented a statistically smaller bone density before treatment. There was a significant loss of bone density for both groups after orthodontic treatment and the group 1 showed a greater bone density loss when compared to group 2 (Table 2).
Table 2.
Statistical comparisons for the difference between the beginning (T0) and the end of the treatment (T1) in two group
| Group 1 | Group 2 | Comparison P | |
|---|---|---|---|
|
|
|||
| Mean ± SD | Mean ± SD | ||
| D1 | 129.62 ± 25.51 | 148.93 ± 30.07 | 0.02* |
| D2 | 99.53 ± 14.34 | 135.97 ± 18.79 | < 0.001** |
| D2-D1 | -29.09 ± 17.56** | -12.96 ± 27.5* | 0.02* |
| H1 | 9.78 ± 1.39 | 11.38 ± 1.86 | < 0.001** |
| H2 | 9.62 ± 1.74 | 11.27 ± 1.09 | < 0.001** |
| H2-H1 | -0.16 ± 1.69 | -0.11 ± 0.75 | 0.51 |
D1, alveolar bone density of pre-treatment; D2, alveolar bone density of post-treatment; H1, alveolar bone height of pre-treatment; H2, alveolar bone height of post-treatment;
Significant for P < 0.05;
Significant for P < 0.01.
Change of bone height
Before treatment, the group 1 presented a statistically smaller bone height than group 2. The average alveolar height was 9.78 mm in group 1 and 11.38 mm in group 2 pre-treatment, respectively. The average difference between pre-treatment and post treatment was 0.16 mm in group 1, and 0.11 mm in group 2. However, there was no significant bone height loss in each group after treatment (Table 2).
Discussion
This study performed a 3D study on the alveolar bone change after fixed orthodontic treatment in patients affected with periodontitis using CBCT. CBCT as the newest CT apparatus has already demonstrated outstanding 3D performance in the area of high quality imaging concerning measurements of the nearby alveolar crest [11,12]. Clinical analysis demonstrated no difference between cadaver measurements and measurements from CBCT [13]. Images from CBCT are anatomically true (1 to 1 in size) 3D representations, providing excellent linear measurements of alveolar bone height.
CT scan has been common for measuring bone density and the Hounsfield Unit (HU) is routinely used to determine the bone density objectively [14]. The lower radiation dose and reduced costs of CBCT make this a useful substitute for CT. But unlike CT, the gray density values of the CBCT images are relative, which are based on densitometry variation of gray scale [15]. A conversion ratio is found between the CBCT gray values and HU values of CT, and to accurately define the bone density with CBCT, it is necessary to multiply CBCT values by 0.7 [16]. However, in the current study, we pay more attention to changes in bone density through treatment and calibration of density values recorded by CBCT may be not required.
A set of customized 3D landmarks and measurements were defined to estimate alveolar bone density and height on CBCT. The depth of the alveolar socket was chosen as the bone height, which reflected effective periodontal bone support around the tooth. Each tooth was adjusted to the reference plan in the coronal view individually, in which the root is the longest. Apical root resorption of anterior incisors during orthodontic treatment has been reported in the literature [17]. Therefore, root resorption had been excluded in this study judging by CBCT. All these were to ensure that the measurements were of reproducibility and reliability.
In our quantitative radiographic study by CBCT, there was a statistically smaller bone density in periodontitis patients than in the controls before treatment. The relationship between periodontitis and generalized bone density has been widely evaluated [18,19]. However, the literature on the relationship between periodontitis and alveolar bone density is limited. The results of this study may suggest that an association of periodontitis with alveolar bone density decrease.
There was a significant bone density loss in both groups after orthodontic treatment. According to the histological findings, bone resorption and deposition is not synchronous, and bone resorption in areas of pressure might precede the formation seen in areas of tension during tooth movement [20]. Therefore, the observable density loss in two groups may due to the less mineralized new bone. However, a particularly noteworthy discovery was that bone density loss for the test group was significantly greater than that of the control group. It was demonstrated that with the same stimulation, bone loss in patients with periodontitis was greater than those with normal periodontal support. Periodontitis patients may display bone metabolism disturbance and we hypothesized that there would be unconventional bone remodeling during tooth movement in patients with periodontitis.
Stress related bone loss is a well-known phenomenon [21,22] and alveolar bone may be demonstrated to be stress-susceptible in patients with periodontitis. A net reduction of alveolar bone density occurred as a consequence of hyperactivity of regional bone absorption. It is recommended that the light force be applied for patients treated with combined periodontal and orthodontic therapies. The lack of definite biomechanics in our study may be a limitation, and future study including more clinical trials in this area could give an explanation. In addition, treated patients must be followed and studied longitudinally.
In the present study, there was not a statistically significant bone height loss in each group. A tooth could be orthodontically moved into an area of reduced bone height with maintenance of height of alveolar bone support [23]. In a prospective study, intrusive force of 12.5 g per tooth was used in patients with a reduced periodontium, and it was found that 25 of the 30 patients exhibited an increase for the area of the alveolus [24]. A histomorphometric study indicated that once periodontal infection had been controlled, application of orthodontic forces contributed to increasing alveolar bone volume, consequently improving bone quality in the periodontitis experiment [25]. Nevertheless, these studies were limited by the fact that no control groups and no 3D images were included. With CBCT, our data confirm previous results that periodontal bone height would not be lost significantly through this combined treatment in periodontitis patients compared to controls [26].
Conclusion
It is concluded that fixed orthodontic treatment would preserve bone height, but not be capable of maintaining bone density for patients with periodontitis. This study indicates that the change of bone density may be more susceptible than that of bone height and perhaps more concern should be focused on bone density loss for patients with combined orthodontic-periodontal treatments.
Acknowledgements
This project was supported by Shanghai Municipal Education Commission Research Fund for Young College and University Teachers (jdy11027), Research Fund of Shanghai Municipal Health Bureau (20134Y061) and College scientific research fund (2012-12) and the National Natural Science Foundation of China (10972142).
Disclosure of conflict of interest
None.
References
- 1.Cao Z, Li C, Zhu G. MMP-1 promoter gene polymorphism and susceptibility to chronic periodontitis in a Chinese population. Tissue Antigens. 2006;68:38–43. doi: 10.1111/j.1399-0039.2006.00615.x. [DOI] [PubMed] [Google Scholar]
- 2.Wagenberg BD, Eskow RN, Langer B. Orthodontic procedures that improve the periodontal prognosis. J Am Dent Assoc. 1980;100:370–373. doi: 10.14219/jada.archive.1980.0099. [DOI] [PubMed] [Google Scholar]
- 3.Zachrisson BU. Clinical implications of recent orthodontic-periodontic research findings. Semin Orthod. 1996;2:4–12. doi: 10.1016/s1073-8746(96)80034-x. [DOI] [PubMed] [Google Scholar]
- 4.Tavares CA, Allgayer S, Calvete Eda S, Polido WD. Orthodontic treatment for a patient with advanced periodontal disease: 11-year follow-up. Am J Orthod Dentofacial Orthop. 2013;144:455–465. doi: 10.1016/j.ajodo.2012.09.025. [DOI] [PubMed] [Google Scholar]
- 5.Corrente G, Abundo R, Re S, Cardaropoli D, Cardaropoli G. Orthodontic movement into infrabony defects in patients with advanced periodontal disease: a clinical and radiological study. J Periodontol. 2003;74:1104–1109. doi: 10.1902/jop.2003.74.8.1104. [DOI] [PubMed] [Google Scholar]
- 6.Southard KA, Liu WJ, Behrents RG. Extraction versus periodontal-orthodontic treatment: a case report. Quintessence Int. 1991;22:605–608. [PubMed] [Google Scholar]
- 7.Parakkal PF. Proceedings of the workshop on quantitative evaluation of periodontal diseases by physical measurement techniques. J Dent Res. 1979;58:547–553. doi: 10.1177/00220345790580020101. [DOI] [PubMed] [Google Scholar]
- 8.Oltramari PV, Navarro Rde L, Henriques JF, Taga R, Cestari TM, Janson G, Granjeiro JM. Evaluation of bone height and bone density after tooth extraction: an experimental study in minipigs. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:9–16. doi: 10.1016/j.tripleo.2007.06.015. [DOI] [PubMed] [Google Scholar]
- 9.Agbaje JO, Jacobs R, Maes F, Michiels K, van Steenberghe D. Volumetric analysis of extraction sockets using cone beam computed tomography: a pilot study on ex vivo jaw bone. J Clin Periodontol. 2007;34:985–990. doi: 10.1111/j.1600-051X.2007.01134.x. [DOI] [PubMed] [Google Scholar]
- 10.Kumar V, Ludlow J, Soares Cevidanes LH, Mol A. In vivo comparison of conventional and cone beam CT synthesized cephalograms. Angle Orthodontis. 2008;78:873–879. doi: 10.2319/082907-399.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morin O, Gillis A, Chen J, Aubin M, Bucci MK, Roach M 3rd, Pouliot J. Megavoltage cone-bine CT: system description and clinical applications. Medical Dosimetry. 2006;31:51–61. doi: 10.1016/j.meddos.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 12.de Oliveira AE, Cevidanes LH, Phillips C, Motta A, Burke B, Tyndall D. Observer reliability of three-dimensional cephalometric landmark identifi cation on cone-beam computerized tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:256–265. doi: 10.1016/j.tripleo.2008.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Veyre Goulet S, Fortin T, Thierry A. Accuracy of linear measurement provided by cone beam computed tomography to assess bone quantity in the posterior maxilla: a human cadaver study. Clin Implant Dent Relat Res. 2008;10:226–230. doi: 10.1111/j.1708-8208.2008.00083.x. [DOI] [PubMed] [Google Scholar]
- 14.Turkyilmaz I, Ozan O, Yilmaz B, Ersoy AE. Determination of bone quality of 372 implant recipient sites using Hounsfield unit from computerized tomography: a clinical study. Clin Implant Dent Relat Res. 2008;10:238–244. doi: 10.1111/j.1708-8208.2008.00085.x. [DOI] [PubMed] [Google Scholar]
- 15.Cassetta M, Sofan AA, Altieri F, Barbato E. Evaluation of alveolar cortical bone thickness and density for orthodontic mini-implant placement. J Clin Exp Dent. 2013;5:e245–252. doi: 10.4317/jced.51228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cassetta M, Stefanelli LV, Pacifici A, Pacifici L, Barbato E. How accurate is CBCT in measuring bone density? A comparative CBCT-CT in vitro study. Clin Implant Dent Relat Res. 2014;16:471–478. doi: 10.1111/cid.12027. [DOI] [PubMed] [Google Scholar]
- 17.Field C, Ichim I, Swain MV, Chan E, Darendeliler MA, Li W, Li Q. Mechanical responses to orthodontic loading: a 3-dimensional finite element multi-tooth model. Am J Orthod Dentofacial Orthop. 2009;135:174–181. doi: 10.1016/j.ajodo.2007.03.032. [DOI] [PubMed] [Google Scholar]
- 18.Hattatoglu-Sönmez E, Ozcakar L, Gökce-Kutsal Y, Karaagaoglu E, Demiralp B, Nazliel-Erverdi H. No alteration in bone mineral density in patients with periodontitis. J Dent Res. 2008;87:79–83. doi: 10.1177/154405910808700114. [DOI] [PubMed] [Google Scholar]
- 19.Phipps KR, Chan BK, Madden TE, Geurs NC, Reddy MS, Lewis CE, Orwoll ES. Longitudinal study of bone density and periodontal disease in men. J Dent Res. 2007;86:1110–1114. doi: 10.1177/154405910708601117. [DOI] [PubMed] [Google Scholar]
- 20.Bridges T, King G, Mohammed A. The effect of age on tooth movement and mineral density in the alveolar tissues of the rat. Am J Orthod Dentofacial Orthop. 1988;93:245–250. doi: 10.1016/s0889-5406(88)80010-6. [DOI] [PubMed] [Google Scholar]
- 21.Frost HM. Skeletal structural adaptation to mechanical usage: 1. Redefining Wolff’s law: the bone modeling problem. Anat Rec. 1990;226:403–413. doi: 10.1002/ar.1092260402. [DOI] [PubMed] [Google Scholar]
- 22.Frost HM. Why do marathon runners have less bone than weight lifters? A vital-biomechanical view and explanation. Bone. 1997;20:183–189. doi: 10.1016/s8756-3282(96)00311-0. [DOI] [PubMed] [Google Scholar]
- 23.Thilander B. Infrabony pockets and reduced alveolar bone height in relation to orthodontic therapy. Semin Orthod. 1996;2:55–61. doi: 10.1016/s1073-8746(96)80040-5. [DOI] [PubMed] [Google Scholar]
- 24.Melsen B. Tissue reaction to orthodontic tooth movement-a new paradigm. Eur J Orthod. 2001;23:671–681. doi: 10.1093/ejo/23.6.671. [DOI] [PubMed] [Google Scholar]
- 25.Garat JA, Gordillo ME, Ubios AM. Bone response to different strength orthodontic forces in animals with periodontitis. J Periodontal Res. 2005;40:441–444. doi: 10.1111/j.1600-0765.2005.00809.x. [DOI] [PubMed] [Google Scholar]
- 26.Artun J, Urbye KS. The effect of orthodontic treatment on periodontal bone support in patients with advanced loss of marginal periodontium. Am J Orthod Dentofacial Orthod. 1988;93:143–148. doi: 10.1016/0889-5406(88)90292-2. [DOI] [PubMed] [Google Scholar]


