ABSTRACT
Purpose: To describe the perspectives of people with stroke and their physiotherapists on the use of biomechanics technology to assess balance and mobility. Methods: This qualitative study used semi-structured interviews with patients with stroke and a focus group with their physiotherapists. Coding of interview and focus-group data used a line-by-line inductive approach, with qualitative software to develop codes into themes. Results: The quantitative data from the assessment were seen as beneficial to providing patients with insight into balance and mobility problems. Physiotherapists found that the assessment confirmed clinical reasoning and aided in precise evaluation of progress but expressed mixed opinions as to whether treatment choice was influenced. Patients would have liked more communication regarding the purpose of the assessment. Patients also stated that trust in their physiotherapists helped them overcome anxieties and that confidence was gained through exposure to more challenging balance assessments. Physiotherapists advocated for the use of a harness system to safely incorporate reactive balance control assessment and training into practice. Conclusion: Both patients and therapists saw value in the quantitative data provided by the assessment. Regardless of the technology used, patients value a strong physiotherapist–patient relationship. Ongoing collaboration between clinicians and researchers should guide the evolution of technology into clinically useful tools.
Key Words: patient outcome assessment, technology, postural balance, stroke
RÉSUMÉ
Objectif : Décrire les vues des gens ayant subi une attaque et de leurs physiothérapeutes au sujet du recours à la biomécanique pour l'évaluation de l'équilibre et de la mobilité. Méthodes : Dans cette étude qualitative, on a mené des interviews semi-structurées auprès de patients ayant subi un accident vasculaire cérébral et organisé un groupe de discussion avec leurs physiothérapeutes. Pour coder les données de ces interviews et de ce groupe, on a procédé par induction ligne à ligne en se servant d'un logiciel qualitatif pour convertir les codes en thèmes. Résultats : On a jugé que les données quantitatives de cette évaluation pouvaient éclairer les patients sur les problèmes d'équilibre et de mobilité. Les physiothérapeutes ont constaté que l'évaluation confirmait le raisonnement clinique et contribuait à une appréciation précise des progrès, mais leurs opinions étaient partagées en matière d'incidence sur le choix de traitement. Les patients auraient voulu plus de communication sur le but de l'évaluation. Ils ont aussi dit que la confiance dans leurs physiothérapeutes les aidait à vaincre leurs anxiétés et que cette confiance s'acquérait par une exposition à des évaluations d'équilibre plus exigeantes. Les physiothérapeutes préconisaient l'emploi d'un système de harnais pour une intégration en toute sécurité à leur pratique de l'évaluation et de la formation en maîtrise réactive de l'équilibre. Conclusion : Et les patients et les thérapeutes attachaient de la valeur aux données quantitatives issues de l'évaluation. Quelle que soit la technologie utilisée, les patients apprécient une étroite relation physiothérapeute-patient. Une constante collaboration entre les cliniciens et les chercheurs devrait nous guider dans la conversion de la technologie en outils d'intérêt clinique.
Mots clés : accident vasculaire cérébral, équilibre postural, évaluation des résultats des patients, technologie
Balance and gait deficits are among the most significant physical consequences of stroke and lead to increased fall risk.1 Comprehensive balance and gait assessment by a physiotherapist is essential to developing treatments aimed at regaining safe independent mobility. Conventional assessment tools used in rehabilitation may identify impairments in balance and gait performance but do not identify the underlying pathophysiological mechanisms responsible for these deficits, which is essential for targeted fall prevention and rehabilitation strategies.1
Biomechanics technologies, such as force plates and pressure-sensitive mats, have been used in research to provide detailed quantitative information on control of balance and gait but have rarely been incorporated into clinical practice.2 Understanding the clinician's perceptions and experience of these technologies would be helpful in developing clinical tools and improving the ongoing collaboration between clinicians and researchers required for knowledge translation.3,4
Patient-centred care involves incorporating patients' perspectives in the provision of health services.5,6 Studies have focused on patients' perspectives of physiotherapy treatment and outcomes, but not on patients' experience of assessments.7–9 Our study therefore aimed to explore the perspectives of both physiotherapists and patients on the use of biomechanics technology in managing balance and mobility impairments after stroke.
Methods
Design overview
We used a descriptive, qualitative study approach to obtain an in-depth understanding of participants' experiences.10 We conducted face-to-face, one-on-one semi-structured interviews with people with stroke to allow for free expression of thoughts; a focus group with physiotherapists fostered interaction during discussion of their experiences. Our study was approved by the Research Ethics Boards at Toronto Rehabilitation Institute—University Health Network (TRI-UHN); participants provided written informed consent before participation.
Background of clinic assessment
The Balance, Mobility & Falls Clinic at TRI-UHN, in operation since 2009, is a unique model of care that partners researchers (including author AM) and physiotherapists (including authors KB and EI) in the patient-care setting to accelerate translation of research into clinical practice. Researchers, along with clinic and primary front-line physiotherapists, collaboratively developed, trialled, and modified a balance and mobility assessment using biomechanics technology. Researchers provided education to physiotherapists regarding the technological measures. Clinic physiotherapists acted as knowledge brokers to facilitate knowledge translation. Assessments were initially conducted by the clinic therapists and were followed by patient-specific consultations with primary treating therapists, which allowed a shared understanding of the information gained; factors that influence balance, mobility, or fall risk; and potential therapeutic interventions. Ongoing feedback on clinical utility guided modification of the assessment protocol and report to align with clinical assessment frameworks and needs.
Patients were eligible for assessment if they were able to stand unsupported for at least 10 seconds and walk without physical assistance, with or without a gait aid, for at least 5 meters. The assessment occurred at the point in each patient's stay when he or she met the eligibility criteria and again before discharge. At the time of our study, the assessments had evolved to become standard care and were conducted independently by the primary treating physiotherapists. A trained health care student provided technical support to operate the equipment and process data for the clinical report. Assessments occurred within the clinic (located on a different floor from the patient care unit) and required approximately 1 hour to fully complete.
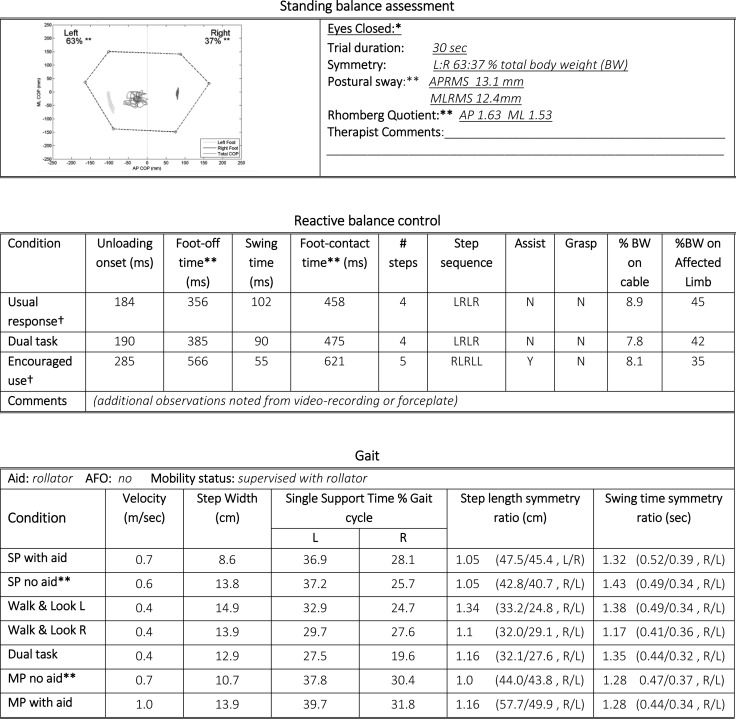
The clinic assessment focuses on three main tasks: (1) walking, measured by a pressure-sensitive walkway;11 (2) postural control in standing, measured with forceplates;12 and (3) perturbation-evoked reactive stepping, using forceplates and a lean-and-release methodology.13 Changes in task conditions can be used to expose different control problems or to increase challenge (e.g., performing task with eyes closed, performing a concurrent cognitive task). In the lean-and-release test, patients lean forward on a cable, which is released unpredictably to induce a reactive step. Patients wear a harness attached to an overhead track support for additional safety. An example of a clinic report can be found in Figure 1.
Figure 1.
Abridged example of the clinic report.
This report is an example only and does not reflect the full clinic report or represent one individual patient's assessment data. Additional information provided in the report is referenced below. Formatting of the report has also been altered for clarity for the reader.
AP=anteroposterior; ML=mediolateral; RMS=root-mean-square; BW=body weight; L=left; R=right; Y=yes; N=no; SP=self-paced; MP=maximal pace; DT=dual task.
*Additional conditions and data include eyes open, max loading/excursion to right and left, and stand in midline.
**Healthy reference values provided to therapists.
†Five trials completed and data provided for usual response and encouraged-use conditions of reactive balance control assessment.
DT conditions require the patient to perform the task while counting backwards by sevens; cognitive task may be altered depending on the patient's cognitive–communicative deficits. Rhomberg quotient provided represents the value for eyes closed divided by eyes open, expressed in both AP and ML directions. Graphs of step-to-step variability values (step length and time) across conditions are also provided.
Participants
We recruited a convenience sample of adult in-patients in the Stroke Service who had completed a clinic assessment, were able to tolerate a 45–60 minute interview, and could understand and communicate in English. All eligible patients who indicated an interest in research involvement were approached consecutively by a research assistant; their participation in this study was not disclosed to the primary physiotherapists. Between January and June 2012, over two data-collection periods (to accommodate researcher availability), we recruited a total of 10 patients; recruitment stopped when recurrent themes became apparent in the data. To ensure a range of experiences and to reduce bias in responses, we included at least 1 patient per participating physiotherapist. One patient interview was discontinued because of cognitive–communication difficulties that only became apparent during the interview; our subsequent analysis therefore includes data from 9 patients (3 women, 6 men), aged 34–85 years.
We recruited all four physiotherapists (two men, two women) employed in the inpatient Stroke Service, all of whom were highly experienced in stroke rehabilitation, ranging from 12 to 23 years. Our focus group included only three physiotherapists because the fourth was unable to attend; this participant completed an individual semi-structured interview instead.
To ensure anonymity, we assigned identifying letters (E–H) to physiotherapists and identifying numbers (1–10) to patients.
Data collection
Members of the research team (EI, KB, AM) who were clinic team members were not involved in the data collection or early analysis phase to avoid any potential influence they might have had on the results. Four researchers external to the clinic were involved in data collection: Two (CT, PP) conducted the patient interviews, and two acted as moderator (BL) and note taker (HJ) for the therapist focus group. A semi-structured question guide consisting of open-ended questions guided interactions (see Boxes 1 and 2). The interviewer and moderator were free to vary the exact wording and order of questions in response to participants. The focus group and interviews were digitally audio-recorded; recordings were transferred to a secure server, transcribed verbatim, and then de-identified. Interviewers created detailed field notes and held regular debriefings.
Box 1.
Interview guide for semi-structured patient interviews
| Question |
|---|
| Can you tell me how your stroke has affected you in terms of getting around? |
| Last week you went up to the clinic where you underwent a series of tests. Can you tell me about what happened while you were there? |
| Why do you think you were there? |
| What was the hardest thing you were asked to do? What was the easiest? |
| What do you think you got out of this experience? |
| As you may know, every patient does the tests when they come and before they leave. What would you tell another patient about to go through these tests? |
Box 2.
Interview guide for physiotherapist focus group and interview
| Question |
|---|
| Tell us your understanding of the purpose of the clinic. |
| What have your experiences been with the clinic model of assessment? |
| What are some of the challenges you've experienced? What things have helped you? |
| Do you communicate the results to your patients? If yes, how? If not, why not? |
| How have the assessments impacted you, in terms of your practice and beyond? |
| What would you add/take away from the clinic? How do you think the clinic can be further developed? |
Data analysis
All transcripts were read by the interviewers (PP, BL, HJ, CT) to gain an overall sense of the data. Constant comparative analysis of patient transcripts refined the interviewing process.14 Transcripts from the first four patient interviews and the focus group were coded independently by all four interviewers, using a line-by-line inductive approach.15 We then created a coding table for use with the remaining transcripts, which were coded and reviewed by teams of two interviewers. To ensure rigour of the coding process, a senior member of the team (CC) coded a portion of a single transcript using the coding table. All transcripts and codes were entered into NVivo 10 software (QSR International Inc., Burlington, ON) to organize data for further analysis. Similar codes were clustered to identify themes, which were refined over several stages. Regular debriefing within the research team addressed different interpretations of the data.
Results
Several themes emerged from the data. Two themes were specific to the technology: (1) clinical applications of the assessment and (2) facilitators of and challenges to the use of technology. Other themes were (1) communication between physiotherapists and patients and (2) patients' sense of security during the assessment and the confidence they gained from the experience.
Perspectives on the use of technology in assessment
Clinical application
Both patients and physiotherapists noted that the assessment provided specific quantitative information. A few patients reported that the results helped them understand and provided further insight into their balance and mobility problems:
I think it's fantastic that there is something like this that can target specific areas about each individual person.
(Patient 3)
Physiotherapists similarly described the value of sharing the quantitative results with patients to draw attention to their abilities. They also found it particularly helpful for patients who were unaware of deficits affecting their mobility:
I was able to give him some feedback … so from this point of view, it gave a bit of meaning, because I had some exact numbers to go by.
(Physiotherapist F)
Patients also noted that the results revealed challenges to balance control that they had not previously recognized:
It wasn't until [the physiotherapist] reviewed the test papers with me that I found that I never really moved my left leg.
(Patient 1)
All physiotherapists agreed that the assessment results were valuable for confirming clinical reasoning and allowed them to track changes precisely over time, but comments varied as to whether results influenced treatment:
Does it change our treatment? No, but does it show the impact of change over time, you know … It's more detailed.
(Physiotherapist E)
I have somebody right now who where we did the perturbation testing, they wouldn't step with one leg … so I am trying to think about that in terms of my treatment.
(Physiotherapist H)
More broadly, physiotherapists commented on the close interaction between research and clinical staff and identified the detailed assessments as a resource for clinical questions:
The idea of researchers and clinicians working together, which is kind of unique and different which I really like … clinicians can help to drive some of the research and vice versa, as well as trying to get best practice into clinical practice.
(Physiotherapist H)
Facilitators and challenges
Physiotherapists identified a learning curve and ongoing challenges with using the technological measures:
Just starting to feel a bit more comfortable with interpreting the data that we've received, the report that we receive—I'm still struggling with it, it's not, it's still not easy, but I'm feeling better about what I'm seeing, and how to interpret it.
(Physiotherapist E)
Clinic support staff were identified as invaluable in providing technological support, including operating equipment and processing the clinical reports:
Getting the technical support for the computer, because if I had to run the computer I would never use it.
(Physiotherapist G)
Physiotherapists also acknowledged the work completed by the clinic's knowledge brokers to adapt and develop standardized clinical protocols:
I think they've made it a little more clinician-friendly for us.
(Physiotherapist E)
All physiotherapists identified time constraints in practice as a major barrier in conducting the assessments among other clinical priorities. The length of the assessment and the short duration of patients' hospital stay were described as being among the contributing factors:
When I have a full caseload … and tough discharges … it can be quite hard to get everything done that I want to get done, in a timely fashion.
(Physiotherapist H)
Physiotherapists also identified space or geographical location as a barrier to incorporating the technology into regular practice:
That would be absolutely fabulous to have [the overhead harness system] very close to our therapeutic area. You know, to have to go and take somebody off over there, also for people to see that, “Hey this isn't so bad, that's cool, let me try that too.” I think that we have to have it close enough that we take away that fear … “Oh, we're going to the assessment in the big lab.”
(Physiotherapist E)
Perspectives on themes explored beyond technology
Communication
Patients expressed mixed views about their orientation to the assessment. Many said they had received sufficient information about the assessment process but would have liked more information about the purpose of the assessment and the relevance of the findings to their care:
I mean we just want to know whatever you are doing, right? … What do they hope to achieve … how is it helpful.
(Patient 5)
One patient received a more detailed explanation of the assessment and appreciated that it was linked to his treatment plan:
Knowing that, you know, my physiotherapist was going to have further insight in helping me with my rehabilitation was really exciting to me.
(Patient 3)
When asked about patient communication, physiotherapists did not mention describing the purpose of the assessment; instead, they noted the importance of sharing results and the need to adapt their explanations to individual patients' needs and interest:
There are people that are numbers people … we go into the numbers with them, but there are people that just need it explained to them in a very simple fashion.
(Physiotherapist E)
Sense of security and confidence
Some patients expressed fear or anxiety about the more challenging assessments, specifically the lean-and-release balance perturbation assessment. The physiotherapists also acknowledged that this assessment could elicit anxiety:
Being in the harness … I think that's probably most challenging for some of our elderly patients, just that whole getting over the fear, and not knowing what to expect.
(Physiotherapist E)
I find even that some people just no matter what, they just, there's a fear, they just can't do it.
(Physiotherapist G)
Despite feeling anxious, many patients told us that they felt secure because of the trust they placed in their physiotherapist:
I know [physiotherapist] was there … if I'm going to fall, well, [physiotherapist] will catch me … you have confidence in, well let's say your partner. Because [physiotherapist] becomes my partner whenever I am doing anything.
(Patient 10)
A few patients reinforced this idea, stating that “trust the physiotherapist” was the best piece of advice they could give to others. They also mentioned that their sense of security improved as they became more familiar with the task.
Physiotherapists expressed a desire to use the overhead harness system in treatment to conduct high-level balance perturbation training:
To actually let somebody get to the edge [of falling], and figure out, or maybe not figure out, but be supported in that.
(Physiotherapist H)
It's really hard to safely push people around and see what their balance reactions are like. We do it in a variety of different ways, but not to the same degree that we can with the harness in place … the patient's … ability to let go and try things, is really important too.
(Physiotherapist G)
Patients expressed increased confidence in their abilities when they were able to accomplish the more challenging balance assessments. One patient with a prior history of falls also suggested that the harness allowed for the opportunity to be safely assessed and suggested using it for training:
I took only two small steps, so I would have fallen. And I don't know how you can practice that unless you're supported by something. I would've liked to have that several times. So that you can, your reaction becomes more habitual … I think it's a very good thing to do, it gives you energy and it gives you confidence.
(Patient 6)
Discussion
Our study sought the perspectives of both physiotherapists and in-patients on a biomechanics-based technological assessment of balance and mobility after stroke. The assessment has several benefits: providing quantitative information, providing patients with insight into their balance control, and enabling therapists to track change. Patients mentioned the technology less often than physiotherapists and were more apt to discuss their physiotherapist–patient relationship—specifically, the importance of trust and clear communication to alleviate any anxiety about the assessment.
Perspectives on the use of technology in assessment
Physiotherapists described some benefits of the quantitative data derived from the assessment, but its influence on treatment was less clearly articulated; this is an important area to explore as the clinical use of such assessments evolves. The mixed response may suggest that some measures are more informative than others; for example, a quantitative value of load on the affected limb may help track treatment progress without, in itself, providing novel insight, whereas the reactive balance control assessment may identify underlying balance control issues beyond what clinicians can observe.
Physiotherapists described challenges with interpretation of the information provided by the technological measure but reported they had progressively gained familiarity in this area, possibly because of the clinic's knowledge translation strategies. To improve knowledge of biomechanical measures, research must aid clinical interpretation and further establish clinically significant thresholds of change.
It is possible that information was revealed by the assessment but not used in treatment because of knowledge gaps related to training strategies. For example, observed dual-task changes in performance may indicate cognitive or attentional influences on balance and gait,16 but limited evidence is available to guide dual-task training.17 Studies revealing the capacity to modify the organization and timing of postural responses for balance control through targeted training are only just emerging.18–20
Finally, the stated value of quantitative data in evaluating change remains noteworthy. It has been well documented that observation-based clinical measures can mask the actual mechanisms underlying change in performance: Functional performance can improve even where there is little evidence of restoration of the paretic limb's contribution to balance control during standing21 or when responding to voluntary22 or external perturbations.23 Further exposure to this physiological information for individual patients may better reveal not only whether change is occurring with treatment but what is changing and thus lead to new approaches.
Our physiotherapist participants expressed a wish that they could incorporate the overhead harness system into the treatment area to facilitate more challenging balance-related training, including perturbation training.20 Reactive balance control, despite its importance to falls, is the least-tested component of balance;2 the desire to use the harness may then suggest a change in therapeutic approach prompted by the use of this assessment in clinical practice.
The results of our study can be used to consider the evolution of technology into clinically useful tools. Ongoing research can help identify key variables that expose underlying sources of impairment linked to task performance. Such research would support improved clinical interpretation, more focused treatment, and a better understanding of clinically meaningful change. Therapist feedback suggests that this will likely require continued collaboration between clinicians and researchers. Our physiotherapist participants suggested that technological measures need to continue to evolve to become clinically feasible tools integrated into today's demanding clinical practice. The development of game-based technology24 and wearable wireless accelerometers25 could be promising, inexpensive alternatives.
Perspectives on themes explored beyond technology
Patients placed more emphasis on the interpersonal aspects of their relationship with their physiotherapist than on the technology. This finding supports previous research concluding that patients are not comfortable evaluating the technical components of therapy and focus instead on their therapist's care.26,27 Within these relationships, patients most value individualized care, support, and open communication.28,29
Despite apprehension about the assessment of perturbation-evoked compensatory stepping, patients trusted their physiotherapist to keep them safe. Improved communication to familiarize patients with each test could also increase their sense of security. Patients also felt that completing the assessment made them more aware of their capabilities, a finding that supports the use of the clinic in educating patients on balance, gait, and falls prevention.
Limitations
Our study has several limitations. First, the physiotherapists in our focus group were highly experienced; future research incorporating the perspectives of less experienced physiotherapists could provide a more comprehensive exploration of this assessment.30 Second, although we do not believe that physiotherapists in the focus group censored their responses, the physiotherapist who was interviewed one-on-one may have had more opportunity to discuss opinions. Moreover, the therapists knew of clinic team members' involvement in the study, and therefore, even with safeguards of anonymity, it is possible that responses may have been tempered. Clinic team members were deliberately restricted from early data analysis to ensure that they did not unduly influence the results. Third, our study was limited to 10 patients; it is possible that had recruitment continued, new themes might have emerged or been refined. Fourth, although the questions posed to participants were open ended, it is possible that the interview guide or the nature of the follow-up questions influenced participants' comments. Finally, our findings should be considered in the context of the clinic measures and assessments; it is possible that use of or exposure to different tests or technological measures might have yielded different results.
Conclusion
Our study is the first to describe physiotherapist and patient perspectives on the use of biomechanics technology to assess balance and mobility after stroke. The physiotherapists found these quantitative data beneficial to aid patient insight, confirm clinical impressions, and track patient progress over time. Despite mixed opinions of the assessment's influence in guiding treatment, therapists advocated using the overhead harness system to incorporate more challenging reactive balance control training into treatment, which suggests support for the evolution of practice. Additional research is needed to explore the use of technological measures in clinical practice and to verify and extend our findings. Irrespective of technological advances in practice, patients' comments suggest that good communication and a trusting physiotherapist–patient relationship are integral to ensuring a positive assessment experience.
Key Messages
What is already known on this topic
Stroke rehabilitation requires a strong therapeutic relationship between patient and physiotherapist to achieve mobility goals. Technology use is commonplace in research but, to this point, has seen limited expansion into the clinical setting.
What this study adds
This study is the first to explore the perspectives of physiotherapists and their patients on the use of technology in clinical assessment. The quantitative information was perceived to be beneficial for patients in providing insight into their balance and mobility abilities and for physiotherapists as an objective measure of patient progress. An overhead harness system was deemed valuable by both groups to enable safe assessment and training of more challenging reactive balance control.
Physiotherapy Canada 2015; 67(1);1–8; doi:10.3138/ptc.2013-63
References
- 1.Weerdesteyn V, de Niet M, van Duijnhoven HJ, et al. Falls in individuals with stroke. J Rehabil Res Dev. 2008;45(8):1195–213. http://dx.doi.org/10.1682/JRRD.2007.09.0145. Medline:19235120. [PubMed] [Google Scholar]
- 2.Sibley KM, Straus SE, Inness EL, et al. Balance assessment practices and use of standardized balance measures among Ontario physical therapists. Phys Ther. 2011;91(11):1583–91. doi: 10.2522/ptj.20110063. http://dx.doi.org/10.2522/ptj.20110063. Medline:21868613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baumbusch JL, Kirkham SR, Khan KB, et al. Pursuing common agendas: a collaborative model for knowledge translation between research and practice in clinical settings. Res Nurs Health. 2008;31(2):130–40. doi: 10.1002/nur.20242. http://dx.doi.org/10.1002/nur.20242. Medline:18213622. [DOI] [PubMed] [Google Scholar]
- 4.Graham ID, Logan J, Harrison MB, et al. Lost in knowledge translation: time for a map? J Contin Educ Health Prof. 2006;26(1):13–24. doi: 10.1002/chp.47. http://dx.doi.org/10.1002/chp.47. Medline:16557505. [DOI] [PubMed] [Google Scholar]
- 5.Cott CA, Boyle J, Fay J, et al. Client-centred rehabilitation: a report to the Ontario Ministry of Health and Long-Term Care. Toronto: Arthritis Community Research Evaluation Unit; 2001. [Google Scholar]
- 6.National Physiotherapy Advisory Group. Essential competency profile for physiotherapists in Canada. Ottawa: The Group; 2009. [Google Scholar]
- 7.Galvin R, Cusack T, Stokes E. Physiotherapy after stroke in Ireland: a qualitative insight into the patients' and physiotherapists' experience. Int J Rehabil Res. 2009;32(3):238–44. doi: 10.1097/MRR.0b013e32832b083c. http://dx.doi.org/10.1097/MRR.0b013e32832b083c. Medline:19381097. [DOI] [PubMed] [Google Scholar]
- 8.Calhoun R, Meischke H, Hammerback K, et al. Older adults' perceptions of clinical fall prevention programs: a qualitative study. J Aging Res. 2011;2011:867341. doi: 10.4061/2011/867341. http://dx.doi.org/10.4061/2011/867341. Medline:21629712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kramer AM. Rehabilitation care and outcomes from the patient's perspective. Med Care. 1997;35(6) Suppl:JS48–57, discussion JS58–63. doi: 10.1097/00005650-199706001-00009. Medline:9191714. [DOI] [PubMed] [Google Scholar]
- 10.Gibson BE, Martin DK. Qualitative research and evidence-based physiotherapy practice. Physiotherapy. 2003;89(6):350–8. http://dx.doi.org/10.1016/S0031-9406(05)60027-2. [Google Scholar]
- 11.Patterson KK, Gage WH, Brooks D, et al. Evaluation of gait symmetry after stroke: a comparison of current methods and recommendations for standardization. Gait Posture. 2010;31(2):241–6. doi: 10.1016/j.gaitpost.2009.10.014. http://dx.doi.org/10.1016/j.gaitpost.2009.10.014. Medline:19932621. [DOI] [PubMed] [Google Scholar]
- 12.Mansfield A, Mochizuki G, Inness EL, et al. Clinical correlates of between-limb synchronization of standing balance control and falls during inpatient stroke rehabilitation. Neurorehabil Neural Repair. 2012;26(6):627–35. doi: 10.1177/1545968311429688. http://dx.doi.org/10.1177/1545968311429688. Medline:22275158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Inness EL, Mansfield A, Lakhani B, et al. Impaired reactive stepping among patients ready for discharge from inpatient stroke rehabilitation. Phys Ther. doi: 10.2522/ptj.20130603. Epub 2014 Aug 7. http://dx.doi.org/10.2522/ptj.20130603. Medline:25104795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Strauss A, Corbin J. Basics of qualitative research: grounded theory procedures and techniques. London: Sage; 1990. [Google Scholar]
- 15.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88. doi: 10.1177/1049732305276687. http://dx.doi.org/10.1177/1049732305276687. Medline:16204405. [DOI] [PubMed] [Google Scholar]
- 16.Woollacott M, Shumway-Cook A. Attention and the control of posture and gait: a review of an emerging area of research. Gait Posture. 2002;16(1):1–14. doi: 10.1016/s0966-6362(01)00156-4. http://dx.doi.org/10.1016/S0966-6362(01)00156-4. Medline:12127181. [DOI] [PubMed] [Google Scholar]
- 17.Yang YR, Wang RY, Chen YC, et al. Dual-task exercise improves walking ability in chronic stroke: a randomized controlled trial. Arch Phys Med Rehabil. 2007;88(10):1236–40. doi: 10.1016/j.apmr.2007.06.762. http://dx.doi.org/10.1016/j.apmr.2007.06.762. Medline:17908563. [DOI] [PubMed] [Google Scholar]
- 18.Marigold DS, Eng JJ, Dawson AS, et al. Exercise leads to faster postural reflexes, improved balance and mobility, and fewer falls in older persons with chronic stroke. J Am Geriatr Soc. 2005;53(3):416–23. doi: 10.1111/j.1532-5415.2005.53158.x. http://dx.doi.org/10.1111/j.1532-5415.2005.53158.x. Medline:15743283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gray VL, Juren LM, Ivanova TD, et al. Retraining postural responses with exercises emphasizing speed poststroke. Phys Ther. 2012;92(7):924–34. doi: 10.2522/ptj.20110432. http://dx.doi.org/10.2522/ptj.20110432. Medline:22421735. [DOI] [PubMed] [Google Scholar]
- 20.Mansfield A, Inness EL, Komar J, et al. Training rapid stepping responses in an individual with stroke. Phys Ther. 2011;91(6):958–69. doi: 10.2522/ptj.20100212. http://dx.doi.org/10.2522/ptj.20100212. Medline:21511992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.de Haart M, Geurts AC, Huidekoper SC, et al. Recovery of standing balance in postacute stroke patients: a rehabilitation cohort study. Arch Phys Med Rehabil. 2004;85(6):886–95. doi: 10.1016/j.apmr.2003.05.012. http://dx.doi.org/10.1016/j.apmr.2003.05.012. Medline:151796. [DOI] [PubMed] [Google Scholar]
- 22.Garland SJ, Willems DA, Ivanova TD, et al. Recovery of standing balance and functional mobility after stroke. Arch Phys Med Rehabil. 2003;84(12):1753–9. doi: 10.1016/j.apmr.2003.03.002. http://dx.doi.org/10.1016/j.apmr.2003.03.002. Medline:14669179. [DOI] [PubMed] [Google Scholar]
- 23.van Asseldonk EHF, Buurke JH, Bloem BR, et al. Disentangling the contribution of the paretic and non-paretic ankle to balance control in stroke patients. Exp Neurol. 2006;201(2):441–51. doi: 10.1016/j.expneurol.2006.04.036. http://dx.doi.org/10.1016/j.expneurol.2006.04.036. Medline:16814283. [DOI] [PubMed] [Google Scholar]
- 24.Clark RA, Bryant AL, Pua Y, et al. Validity and reliability of the Nintendo Wii Balance Board for assessment of standing balance. Gait Posture. 2010;31(3):307–10. doi: 10.1016/j.gaitpost.2009.11.012. http://dx.doi.org/10.1016/j.gaitpost.2009.11.012. Medline:20005112. [DOI] [PubMed] [Google Scholar]
- 25.Mancini M, Horak FB. The relevance of clinical balance assessment tools to differentiate balance deficits. Eur J Phys Rehabil Med. 2010;46(2):239–48. Medline:20485226. [PMC free article] [PubMed] [Google Scholar]
- 26.Cleary PD, McNeil BJ. Patient satisfaction as an indicator of quality care. Inquiry. 1988;25(1):25–36. Medline:2966123. [PubMed] [Google Scholar]
- 27.Burroughs TE, Davies AR, Cira JC, et al. Understanding patient willingness to recommend and return: a strategy for prioritizing improvement opportunities. Jt Comm J Qual Improv. 1999;25(6):271–87. doi: 10.1016/s1070-3241(16)30444-8. Medline:10367265. [DOI] [PubMed] [Google Scholar]
- 28.Delbanco TL. Enriching the doctor-patient relationship by inviting the patient's perspective. Ann Intern Med. 1992;116(5):414–8. doi: 10.7326/0003-4819-116-5-414. http://dx.doi.org/10.7326/0003-4819-116-5-414. Medline:1736775. [DOI] [PubMed] [Google Scholar]
- 29.Melander Wikman A, Faltholm Y. Patient empowerment in rehabilitation: “somebody told me to get rehabilitated. Adv Physiother. 2006;8(1):23–32. http://dx.doi.org/10.1080/14038190500494774. [Google Scholar]
- 30.McGlynn M, Cott CA. Weighing the evidence: clinical decision making in neurological physical therapy. Physiother Can. 2007;59(4):241–252. http://dx.doi.org/10.3138/ptc.59.4.241. [Google Scholar]