Abstract
Purpose The purpose of this study was to evaluate the outcomes of perilunate dislocations and fracture-dislocations treated with arthroscopically assisted mini-invasive reduction and fixation.
Methods Between June 2012 and May 2014, 24 patients who had a dorsal perilunate dislocation or fracture-dislocation were treated with arthroscopically assisted reduction and percutaneous fixation. The mean follow-up was 14.8 months (range 6–32 months).
Clinical outcomes were evaluated on the basis of range of motion; grip strength; Mayo Wrist Score; Quick Disabilities of the Arm, Shoulder and Hand (QuickDASH) questionnaire; and Patient-Rated Wrist Evaluation (PRWE) score. Radiographic evaluations included time to scaphoid union, carpal alignments, and any development of arthritis.
Results The range of flexion-extension motion of the injured wrist averaged 86% of the values for the contralateral wrist. The grip strength of the injured wrist averaged 83% of the values for the contralateral wrists. The mean QuickDASH score was 6, and the mean PRWE score was 10. According to the Mayo Wrist Scores, overall functional outcomes were rated as excellent in 13 patients (54%), good in 6 (25%), fair in 4 (17%), and poor in 1 (4%). Scaphoid nonunion developed in one patient. Reduction obtained during the operation was maintained within normal ranges in all patients. Arthritis had not developed in any patient at final follow-up.
Conclusions Arthroscopically assisted mini-invasive reduction with percutaneous fixation is a reliable and favorable alternative in the treatment of perilunate injuries according to our early follow-up results.
Level of Evidence: Level IV, Therapeutic.
Keywords: perilunate dislocation, scaphoid fracture, minimally invasive surgery, wrist arthroscopy
Perilunate injuries represent a spectrum of condition that includes ligamentous and/or bony disruption of the wrist. The pathway of injury may be strictly perilunar in so-called “pure ligamentous” perilunate dislocations (PLDs) through the lesser arc, or the injury may cause perilunate fracture-dislocations (PLFDs) through the greater arc, most commonly through the scaphoid (transscaphoid PLFDs). They are rare but devastating injuries, often the result of high-energy trauma.1 2 3
The key to successful treatment of perilunate injuries is to achieve early anatomic reduction and maintain the carpal alignment, no matter how the bones are dislocated or fractured.4 Closed reduction and cast treatment for perilunate injuries have shown an unacceptable failure rate in terms of quality of reduction and outcome.4 For this reason, surgical treatment with open reduction of the carpal bones, repair or reconstruction of the ligaments, and internal fixation of the fractures has been generally accepted for PLDs and PLFDs.3 4 5 6 7 8 9 10 11 12 However, open surgery requires dissection of the important capsular and ligamentous structures of the wrist, which may led to capsular scarring and joint stiffness. Furthermore, there is increased chance of damage to the already tenuous blood supply to the scaphoid and torn ligament. Recently, arthroscopically assisted mini-invasive management of PLDs and PLFDs has been suggested by several authors.3 4 13 14 15 16 Combined with fluoroscopy, wrist arthroscopy allows anatomic reduction and precise percutaneous internal fixation of the carpal bones with minimal tissue dissection. This technique may encourage healing with less stiffness, but at this time there are few series available to support this notion.3 The purpose of this study was to review the outcomes of arthroscopic reduction and percutaneous fixation of a series of patients with acute PLDs and PFLDs.
Patients and Methods
Twenty-five consecutive patients with acute dorsal PLDs or PLFDs were treated with arthroscopically assisted reduction and percutaneous fixation between June 2012 and May 2014. One patient did not return for follow-up after removal of the Kirschner wires (K-wires). The remaining 24 patients returned for a comprehensive evaluation. The evaluation consisted of an interview, physical examination, and standard anteroposterior (AP) and lateral radiographs. The radiolunate and scapholunate angles were measured to assess the alignment of the carpal bones. Each patient was assigned a Mayo Wrist Score (MWS) after evaluation for pain, functional status, range of motion, and grip strength.5 Patients' subjective outcomes were evaluated with the Quick Disabilities of the Arm, Shoulder, and Hand (QuickDASH) questionnaire17 and Patient-Rated Wrist Evaluation (PRWE) score.18 The mean follow-up was 14.8 months (range, 6–32 months).
Among the 24 patients (21 men and 3 women) who formed the study cohort, 20 had transscaphoid dorsal PLFDs, and four had dorsal PLDs. The four PLDs were all Herzberg stage IIA injuries (the lunate subluxated out of its fossa but remains partially reduced and rotated less than 90°). All injuries were closed. The mean age at the time of injury was 28 years (range 17–51 years). The dominant wrist was injured in nine patients. The average time from injury to surgery was 8 days (range 2–20 days). Because many patients were referred to our hospital (a tertiary orthopedic center) several days after the injury, only eight patients were treated within 1 week. Three patients had concomitant fractures outside the injured wrist: one intertrochanteric femoral fracture, one ipsilateral radial head fracture, and one contralateral distal radius fracture. Nine patients had median nerve symptoms after the wrist trauma.
Operative Technique
Reduction of the Dislocation of the Capitolunate Joint
Closed reduction of the dislocations of the capitolunate joint had been attempted for all patients at the time of initial presentation. Eleven of the 24 dislocations were reduced. For the remaining 13 dislocations, we tried close reduction again in the operation room under brachial plexus block before arthroscopy was performed. Eight dislocations were reduced under anesthesia, but this still failed in five. We then proceeded to arthroscopically assisted reduction of the capitolunate joint under traction of the wrist arthroscopic traction tower. The 3–4 portal was used for initial inspection. The volarly tilting lunate usually provides enough space for the placement of the scope and the inspection of the radiocarpal joint. We found that the failure of close reduction was due to the volarly tilting lunate (along with a proximal scaphoid fragment in trans-scaphoid PLFDs) getting stuck by the capitate or interposed torn palmar capsular ligaments. With finger-trap suspension, we used a Freer elevator or shoulder arthroscopic probe to reduce the dislocation arthroscopically by a “shoehorn maneuver” (Fig. 1). We found that the 4–5 portal was convenient to apply this maneuver because the instruments were directly facing the subluxated lunate. All the five dislocations were arthroscopically reduced successfully by this technique.
Fig. 1.
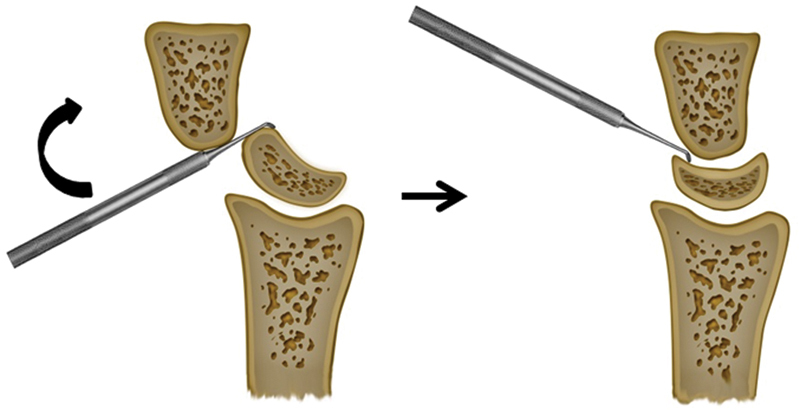
Arthroscopic reduction of the capitolunate joint by a “shoehorn maneuver.”
Perilunate Dislocations
The 3–4 and 4–5 portals were used to perform a thorough examination of the radiocarpal joint. Usually, initial vision was rather obscure. Débridement of intra-articular hematoma, raised ligament flaps, and bony or chondral debris was always required to improve the vision. We used wet arthroscopy to facilitate the débridement and controlling the bleeding. Thus, the tourniquet was not inflated in almost all cases. The triangular fibrocartilage complex (TFCC), volar and intercarpal ligaments, were examined by direct inspection and manual testing with an arthroscopic probe. TFCC tears were addressed according to the injury types. All volar ligament injuries were treated with débridement after the carpal fractures and dislocations were precisely reduced and fixed. Cartilage damages were assessed and the unstable edges were treated with débridement.
The midcarpal joint was examined through radial and ulnar midcarpal portals. The scapholunate (SL) and lunotriquetral (LT) ligaments were assessed by a probe. Any soft tissue or bony fragments interposed between the SL and LT intervals were débrided or removed to facilitate reduction of the intercarpal joint. Concomitant chondral injuries were identified and débrided.
Under a fluoroscopy unit, two K-wires were placed toward the lunate from the scaphoid and triquetrum respectively, without crossing the intercarpal interval (Fig. 2a–d). If the lunate was not in neutral position (i.e., in volar or dorsal tilting), the wrist was passively extended or flexed to restore the normal radiolunate (RL) angle. The RL joint was then temporarily transfixed with a percutaneous K-wire inserted from the dorsal distal radius (Fig. 2e). Under direct visualization through the midcarpal portal, reduction of the SL and LT intervals was conducted by manipulating the K-wires of the scaphoid and triquetrum. Correction of steps or rotational deformity between the intercarpal intervals could be obtained by a probe or depressor through the midcarpal portal (Fig. 2f,g). The K-wires were then driven across the intercarpal intervals into the lunate (Fig. 2h). In cases with grossly unstable and easily redislocated SL joints (3 of 4 PLDs in our series), which means both primary and secondary stabilizers are incompetent, we augmented the SL ligament by a dorsal capsulodesis through a mini-invasive approach. We extended 3–4 portal to a 2-cm incision. The dorsal capsule was exposed but not opened. Two suture anchors were placed into the scaphoid and the lunate, respectively, under fluoroscopic control, 1 cm away from the SL interval. After the SL interval was reduced and fixed with two wires as just described, sutures from the two anchors were then tied together outside the dorsal capsule (Fig. 3).
Fig. 2.
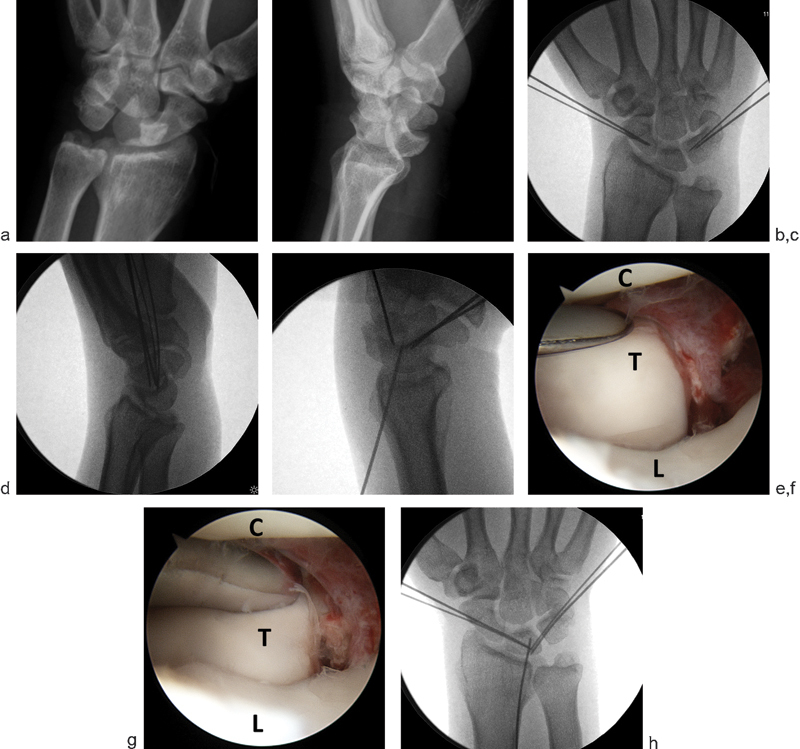
(a,b) PA and lateral radiographs showing a perilunate dislocation. (c,d) PA and lateral radiographs showing the preparing of the K-wires. Note the dorsal tilting of the luntate. (e) The RL joint is transfixed with a K-wire inserted from the dorsal distal radius when the lunate was in neutral position. (f,g) Correction of steps and rotational deformity between the LT intervals by a depressor. C: capitate. T: triquetrum. L: lunate. (h) The K-wires were driven across the intercarpal intervals into the lunate.
Fig. 3.

Augmentation of the SL ligament through a mini-invasive approach.
Although PLDs are regard as “pure ligamentous” injuries, we found that concomitant carpal bone fractures are not uncommon. In our four PLD patients, two had displaced intra-articular triquetral fractures, which required arthroscopic assisted percutaneous reduction and fixation (Fig. 4a–f).
Fig. 4.
(a,b) 30-year-old amateur golf player. Displaced triquetral fracture was reduced and fixed by percutaneous pinning in a patient with PLD. C: capitate. T: triquetrum. L: lunate. (c,d) Postoperative PA and lateral radiographs. Note that the triquetral fracture was reduced and fixed by a percutaneous wire. (e,f) Carpal alignment was maintained at 10-month postop. This patient returned back to the games at 3-month postop.
One patient who had associated combined TFCC large central tear and unclear tear was treated with débridement of the central tear and repair of the ulnar tear.
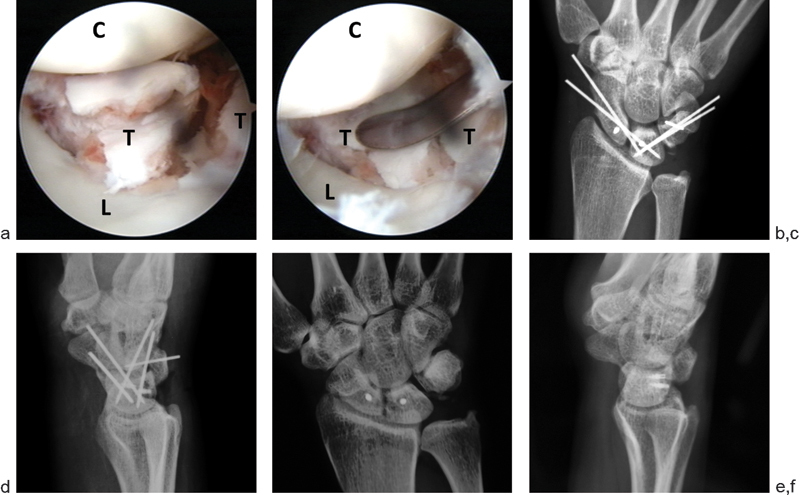
Trans-Scaphoid Perilunate Fracture-Dislocations
A thorough examination and débridement of the radiocarpal and midcarpal joints was the same as described earlier. Although there was no significant SL dissociation radiographically, we found that almost all patients (19 of the 20 patients) had hemorrhage and some attenuation of scapholunate ligament. Furthermore, two patients had concomitant SL ligament avulsion from the lunate (Fig. 5). Evaluation at midcarpal joint confirmed that these two ligament injuries were Geissler grade III injuries, which required additional scapholunate pinning.
Fig. 5.
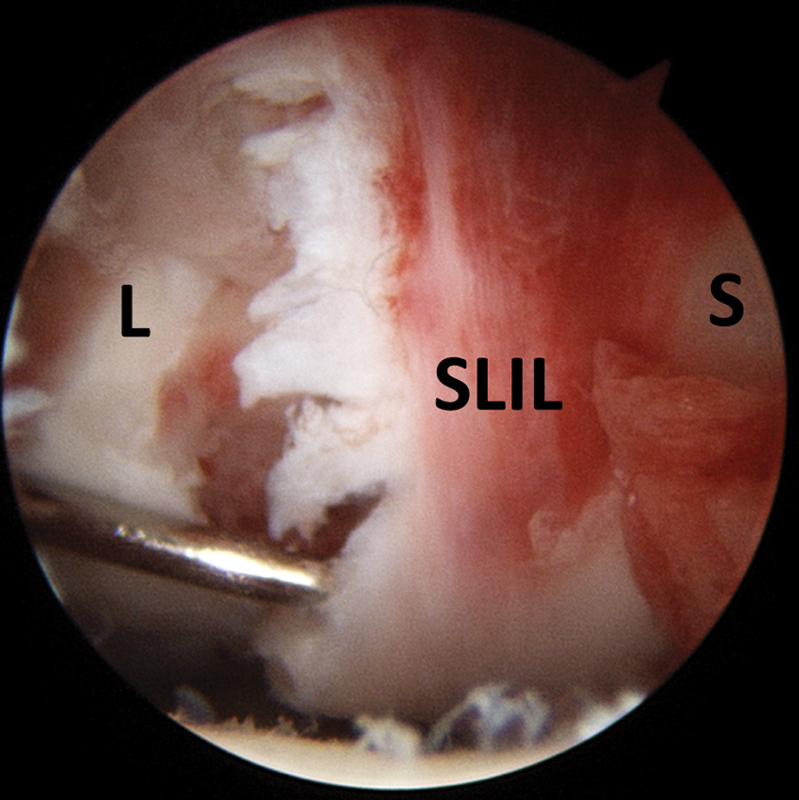
SL ligament (SLIL) avulsion from the lunate in a patient had trans-scaphoid PLFD. L: lunate. S: scaphoid.
The scaphoid fractures were treated first. In transscaphoid PLFDs, the scaphoid fractures are usually significantly displaced and sometimes comminuted (Fig. 6a,b). The most critical and technical demanding step was the arthroscopically assisted reduction and percutaneous fixation of the scaphoid fracture. The wrist was placed on the operation table. Many times, attempts at manual close reduction were unsatisfactory. In these cases, we preplaced a guide wire along the central axis of the distal fragment from the scaphoid tubercle, not crossing the fracture line. With grossly unstable or comminuted fractures, one or two more antirotation wires were introduced into the distal fragment. One or two additional K-wires were placed into distal fragment as joysticks for arthroscopic reduction. We found two joysticks were more efficient to correct the three-dimensional displacement of the fracture (Fig. 6c). The wrist was placed in traction and the fractures were visualized at ulnar midcarpal portal (Fig. 6d). The fracture was then reduced by controlling the joysticks. Sometimes added leverage may be required by a probe or a K-wire joystick placed at proximal fragment. Attention should be paid to correct the rotational displacement, as well as translational displacement, in both the sagittal and the coronal plane. Some residual gap might be present, which could be reduced by placing a compression screw later. After the anatomic reduction was achieved, the assistant would drive the guide wire and antirotation wire across the fracture line to the proximal fragment to hold the reduction. We used cannulated headless Acutrak screws (Acumed, Beaverton, OR, USA) for all scaphoid fracture fixations. Retrograde reaming and screw placement were performed after the traction was off and the wrist was put in extension on the operation table. This would facilitate the surgeon to apply compression force across the fracture, frequently using fluoroscopy to gauge the depth of screw placement. For the five patients with proximal one-third scaphoid fractures, the cannulated screw was placed from dorsal approach. In these cases, the guide wire was advanced out to the dorsal wrist while the wrist was flexed. Reaming and screw placement were conducted from a stab incision over the dorsal wrist. In cases with significant fracture comminution or instability, one antirotation wire was left to facilitate fracture stabilization. All the wires were cut and buried underneath the skin.
Fig. 6.
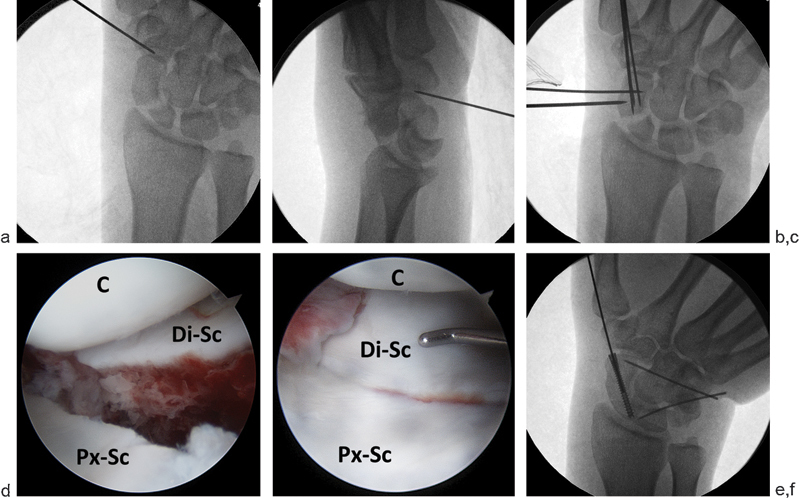
(a,b) PA and lateral radiographs showing a transscaphoid perilunate dislocation. (c) Two joysticks are used to correct the three-dimensional displacement of the scaphoid fracture. (d) Midcarpal arthroscopy showing the displaced scaphoid fracture. C: capitate. Di-Sc: distal scaphoid. Px-Sc: proximal scaphoid. (e,f) Accurate reduction and fixation of the scaphoid fracture. C: capitate. Di-Sc: distal scaphoid. Px-Sc: proximal scaphoid.
Associated soft tissue injuries and carpal malalignments were addressed the same as described for perilunate dislocations. Three patients with TFCC injuries (two large central tears with unstable flaps, one partial dorsal tear) were treated with débridement. Reduction and compression of the fracture, placement of the screw, and correction of the carpal alignment were confirmed both fluoroscopically and arthroscopically (Fig. 6e,f).
Postoperative Management
After the operation, four patients with TFCC injuries were immobilized in a long-arm thermoplastic cast with forearm in semi-supination, and then in a short-arm splint for 6 weeks. All other wrists were immobilized in short-arm thermoplastic cast after the operation. The thumb was incorporated in the cast for trans-scaphoid PLFD. The K-wires and splint were removed at 8 weeks postoperatively, followed by active wrist motion exercise. Manual activities and sports were started after the scaphoid united.
Results
Close reduction and percutaneous fixation was achieved in all 24 patients in our series. The mean operation time was 170 minutes (range 140–300 minutes).
Of the 20 scaphoid fractures, 15 were wrist fractures and five were proximal one-third fractures. Twelve of the 20 fractures had comminution. Arthroscopic inspection showed small to moderate capitate cartilage loss in eight wrists, but no real capitate fracture was noted. Two patients had fracture of the volar rim of the lunate, and three patients had triquetrum fracture.
The normal carpal alignments were restored and maintained for all patients at final evaluation. Nineteen of the 20 scaphoid fractures healed at a mean time of 13 weeks (range 9–20 weeks). The patient with scaphoid nonunion did not want further treatment at final evaluation because he seldom had wrist pain and he functioned well. The proximal fragment of the scaphoid showed increased density, but there was no collapse, and the Gilula arcs were congruent.
For the nine patients with median nerve symptoms, the symptoms resolved within 2 weeks after arthroscopic reduction, and no patient required carpal tunnel release.
At final follow-up, the mean flexion was 55° (range 35–75°), which was 84% compared with the contralateral wrist. The mean extension was 57° (range, 45–75°), 88% of the contralateral side. The mean grip strength was 33 kg (range, 8–48 kg), which was 83% of the contralateral wrist.
The mean Mayo Wrist Score was 86 (range 40–100), with excellent in 13 patients, good in 6, fair in 4, and poor in 1. The patient who had a poor result sustained associated central TFCC tear and complained of ulnar-sided wrist pain with grip and forearm pronation-supination activities. The mean QuickDASH score was 6 (range 0–65) and the PRWE score was 10 (range 0–63).
All 24 patients (12 were manual labor workers) were able to return to their preinjury occupations at a mean time of 4.9 months (range 1–12). Three labor workers returned to some reduced workloads, while the other 21 patients returned to their previous work.
Discussion
Management of perilunate injuries remains challenging and controversial. Unacceptable outcomes of closed reductions and cast treatments, along with the recognition that functional recovery closely parallels the accuracy of restoring carpal alignment, have led to increasing enthusiasm for open treatment.3 16 Many series have shown good outcomes of open reduction and internal fixation with dorsal, volar, or combined approach.3 4 5 6 7 8 9 10 11 12 19 Open surgery, however, involves soft tissue dissection, which may lead to capsular scarring, joint stiffness, and damage of the already tenuous vascular supply to the scaphoid.
Chou et al20 reported the favorable outcome of percutaneous fixation under fluoroscopic guidance alone for 24 acute transscaphoid PLFDs. However, accurate reduction of displaced scaphoid fracture as well as carpal alignment is very difficult to achieved under fluoroscopy guidance alone. In their series, they observed one patient with radial wrist pain and a bone spur caused by an unreduced scaphoid at 10 months after the initial surgery. Arthroscopy allows complete visualization of the carpal bones, joints, and fractures. Combined with fluoroscopy, arthroscopy contributes a minimally invasive and more efficient method to assist anatomic reduction and percutaneous fixation.3 However, this method is technically challenging, and at this time there are few series available to support it.13 14 15 16 Park13 first reported three cases in 2005, and then Jeon16 reported four cases. Recently, Wong14 reported 21 transscaphoid PLFDs, and Kim15 reported 20 PLDs and PLFDs; both series noted encouraging outcomes.
Similar to Wong and Kim's series, our series of 24 PLDs and PLFDs showed favorable results when compared with the series of open techniques reported between 2004 and 2014 (Table 1). Furthermore, for patients with open surgery, sports and heavy labor are rarely possible before 6 months, and usually require 12 months of continuous rehabilitation to regain good function.19 The result of our study suggested a quicker recovery. The average time of returning to former occupation was 4.9 months. One amateur golf player (PLD) and one amateur basketball player (PLFD) were able to return to their games at 3 months and 6 months postoperative, respectively. Nineteen of 24 patients (79%) achieved excellent or good results according to Mayo Wrist Score as early as 1 year postoperation.
Table 1. Summary of reported series of PLDs and PLFDs, 2004–2014.
| Author (year) |
Type of Surgery | Cases | Pathology | Average Follow-Up (m) |
Flexion-Extension Arc (% of Contralateral) | Grip Strengh (% of Contralateral) | Average Mayo Wrist Score |
No. of Scaphoid Nonunions (Nonunion Rate) |
|
|---|---|---|---|---|---|---|---|---|---|
| PLD | PLFD | ||||||||
| Trumble8 (2004) | Open | 22 | 22 | 0 | 49 | 80 | 77 | – | – |
| Knoll9 (2005) | Open | 25 | 0 | 25 | 44.3 | 83 | 80 | – | 0 |
| Souer10 (2007) | Open | 18 | 6 | 12 | 45.5 | 55–71 | 67–76 | 66–71 | 2 (17%) |
| Forli11 (2010) | Open | 18 | 11 | 7 | 156 | 76 | 87 | 76 | 1 (14%) |
| Kremer12 (2010) | Open | 39 | 9 | 30 (20 scaphoid fractures) | 66.5 | 63 | 71 | 70 (Excellent or good results in 36% patients) |
2 (10%) |
| Wong14 (2008) | Arthroscopic | 21 | 0 | 21 | 36 | 88 | 87 | 80 | 1 (5%) |
| Kim15 (2012) | Arthroscopic | 20 | 5 | 15 | 31.2 | 79 | 78 | 79 | 2 (13%) |
| Our series (2015) | Arthroscopic | 24 | 4 | 20 | 14.8 | 86 | 83 | 86 (Excellent or good results in 79% patients) |
1 (5%) |
One important prerequisite of this mini-invasive treatment is that close reduction of capitolunate joint can be achieved. Because many of the patients did not present to our institution at the time of initial injury, the largest interval between injury and close reduction of the capitolunate joint was more than 2 weeks in our series. In the five cases with failed close reduction by manipulation, we had no difficulty in achieving arthroscopically assisted close reduction by means of the previously mentioned “shoehorn maneuver.”
Although 12 patients in our series had severely comminuted and displaced scaphoid fractures, only one of the 20 transscaphoid PLFDs developed scaphoid nonunion. This may be partly because arthroscopically assisted reduction and fixation allow reliable reduction of the fracture and preservation of an already tenuous blood supply to scaphoid.21 22 Besides, we used cannulated compression screws instead of K-wires for scaphoid fixation in all cases for better mechanical stability.23 Additional K-wire was placed when there was significant instability or comminution.
One limitation of this study is that this is not a randomized study with open surgery for comparison. Another limitation is the short follow-up time. Although it is noted that further improvement usually occurs with time and use 1 year after the open surgery,20 we also agree with Forli et al12 that degenerative changes are likely to increase with time, which might modify the functional outcome. In our series, the normal carpal alignments were maintained, and there were no signs of degenerative changes for all patients at final follow-up. Nonetheless, long-term results are required to provide better support to the notion that the arthroscopically assisted technique is a reliable and favorable alternative in the treatment of perilunate injuries.
Disclosure
No benefits in any form have been received or will be received related directly or indirectly to the subject of this article.
Footnotes
Conflict of Interest None
References
- 1.Mayfield J K, Johnson R P, Kilcoyne R K. Carpal dislocations: pathomechanics and progressive perilunar instability. J Hand Surg Am. 1980;5(3):226–241. doi: 10.1016/s0363-5023(80)80007-4. [DOI] [PubMed] [Google Scholar]
- 2.Johnson R P. The acutely injured wrist and its residuals. Clin Orthop Relat Res. 1980;(149):33–44. [PubMed] [Google Scholar]
- 3.Herzberg G. Perilunate and axial carpal dislocations and fracture-dislocations. J Hand Surg Am. 2008;33(9):1659–1668. doi: 10.1016/j.jhsa.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 4.Weil W M, Slade J F III, Trumble T E. Open and arthroscopic treatment of perilunate injuries. Clin Orthop Relat Res. 2006;445(445):120–132. doi: 10.1097/01.blo.0000205889.11824.03. [DOI] [PubMed] [Google Scholar]
- 5.Cooney W P, Bussey R, Dobyns J H, Linscheid R L. Difficult wrist fractures. Perilunate fracture-dislocations of the wrist. Clin Orthop Relat Res. 1987;(214):136–147. [PubMed] [Google Scholar]
- 6.Herzberg G, Forissier D. Acute dorsal trans-scaphoid perilunate fracture-dislocations: medium-term results. J Hand Surg [Br] 2002;27(6):498–502. doi: 10.1054/jhsb.2002.0774. [DOI] [PubMed] [Google Scholar]
- 7.Budoff J E. Treatment of acute lunate and perilunate dislocations. J Hand Surg Am. 2008;33(8):1424–1432. doi: 10.1016/j.jhsa.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 8.Trumble T, Verheyden J. Treatment of isolated perilunate and lunate dislocations with combined dorsal and volar approach and intraosseous cerclage wire. J Hand Surg Am. 2004;29(3):412–417. doi: 10.1016/j.jhsa.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 9.Knoll V D, Allan C, Trumble T E. Trans-scaphoid perilunate fracture dislocations: results of screw fixation of the scaphoid and lunotriquetral repair with a dorsal approach. J Hand Surg Am. 2005;30(6):1145–1152. doi: 10.1016/j.jhsa.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 10.Souer J S, Rutgers M, Andermahr J, Jupiter J B, Ring D. Perilunate fracture-dislocations of the wrist: comparison of temporary screw versus K-wire fixation. J Hand Surg Am. 2007;32(3):318–325. doi: 10.1016/j.jhsa.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 11.Forli A, Courvoisier A, Wimsey S, Corcella D, Moutet F. Perilunate dislocations and transscaphoid perilunate fracture-dislocations: a retrospective study with minimum ten-year follow-up. J Hand Surg Am. 2010;35(1):62–68. doi: 10.1016/j.jhsa.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 12.Kremer T, Wendt M, Riedel K, Sauerbier M, Germann G, Bickert B. Open reduction for perilunate injuries—clinical outcome and patient satisfaction. J Hand Surg Am. 2010;35(10):1599–1606. doi: 10.1016/j.jhsa.2010.06.021. [DOI] [PubMed] [Google Scholar]
- 13.Park M J, Ahn J H. Arthroscopically assisted reduction and percutaneous fixation of dorsal perilunate dislocations and fracture-dislocations. Arthroscopy. 2005;21(9):1153. doi: 10.1016/j.arthro.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 14.Wong T C, Ip F K. Minimally invasive management of trans-scaphoid perilunate fracture-dislocations. Hand Surg. 2008;13(3):159–165. doi: 10.1142/S0218810408004018. [DOI] [PubMed] [Google Scholar]
- 15.Kim J P, Lee J S, Park M J. Arthroscopic reduction and percutaneous fixation of perilunate dislocations and fracture-dislocations. Arthroscopy. 2012;28(2):196–20300. doi: 10.1016/j.arthro.2011.08.299. [DOI] [PubMed] [Google Scholar]
- 16.Jeon I H, Kim H J, Min W K, Cho H S, Kim P T. Arthroscopically assisted percutaneous fixation for trans-scaphoid perilunate fracture dislocation. J Hand Surg Eur Vol. 2010;35(8):664–668. doi: 10.1177/1753193410375781. [DOI] [PubMed] [Google Scholar]
- 17.Hudak P L Amadio P C Bombardier C; The Upper Extremity Collaborative Group (UECG). Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected] Am J Ind Med 1996296602–608. [DOI] [PubMed] [Google Scholar]
- 18.MacDermid J C. Development of a scale for patient rating of wrist pain and disability. J Hand Ther. 1996;9(2):178–183. doi: 10.1016/s0894-1130(96)80076-7. [DOI] [PubMed] [Google Scholar]
- 19.Melone C P Jr, Murphy M S, Raskin K B. Perilunate injuries. Repair by dual dorsal and volar approaches. Hand Clin. 2000;16(3):439–448. [PubMed] [Google Scholar]
- 20.Chou Y C, Hsu Y H, Cheng C Y, Wu C C. Percutaneous screw and axial Kirschner wire fixation for acute transscaphoid perilunate fracture dislocation. J Hand Surg Am. 2012;37(4):715–720. doi: 10.1016/j.jhsa.2012.01.019. [DOI] [PubMed] [Google Scholar]
- 21.Toh S, Nagao A, Harata S. Severely displaced scaphoid fracture treated by arthroscopic assisted reduction and osteosynthesis. J Orthop Trauma. 2000;14(4):299–302. doi: 10.1097/00005131-200005000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Slade J F, Lozano-Calderón S, Merrell G, Ring D. Arthroscopic-assisted percutaneous reduction and screw fixation of displaced scaphoid fractures. J Hand Surg Eur Vol. 2008;33(3):350–354. doi: 10.1177/1753193408090121. [DOI] [PubMed] [Google Scholar]
- 23.Christodoulou L S, Kitsis C K, Chamberlain S T. Internal fixation of scaphoid non-union: a comparative study of three methods. Injury. 2001;32(8):625–630. doi: 10.1016/s0020-1383(01)00018-3. [DOI] [PubMed] [Google Scholar]


