Abstract
Gorham's disease is a rare disorder of uncertain etiology characterized by spontaneous and progressive osteolysis of one or more skeletal bones. Till date, less than 200 cases have been reported in the international literature with about 51 cases involving the maxillofacial site. The radiographic findings associated with Gorham's disease are particularly dramatic, as in some cases a complete resorption of the involved bone can occur, leading to the definition of phantom bone or disappearing bone disease. The purpose of this review is to make our community aware of this rare entity and to discuss the etiopathology, clinical presentation, radiographic findings, histopathology, differential diagnoses and treatment modalities for patients with vanishing bone disease.
Keywords: Gorham's disease, mandible, massive osteolysis, vanishing bone disease
INTRODUCTION
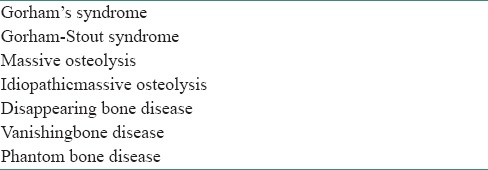
Gorham's disease also called as vanishing bone disease, acute spontaneous absorption of bone, hemangiomatosis, lymphangiomatosis, is a rare disease characterized by proliferation of thin-walled vascular channels which leads to destruction and resorption of osseous matrix.[1] Numerous names have been used in the literature [Table 1].
Table 1.
Synonyms used for Gorham's disease[1]
Idiopathic osteolysis was first described in 1838 by Jackson as a case of disappearing humerus and led him title his work as ‘a boneless arm′.[1] It was Romer in 1924 who reported first case in jaws. Complete mandible lysis was reported by Thoma in 1933.[2] It was Gorham in 1954 and Gorham and Stout in 1955 who presented a case series.[1] The condition was named after these physicians, Lemuel Whittington Gorham and Arthur Purdy Stout as Gorham and Stout syndrome.[3]
Since the initial description of this disease, 60 years have elapsed; but the etiology of Gorham's disease is still very speculative. There is no evidence of a malignant, neuropathic, or infectious component involved in the causation of this disorder.[4]
ETIOPATHOLOGY
Till date, the exact etiology and nature of the disease process remains undetermined. The pathologic process is the replacement of normal bone by an aggressively expanding nonneoplastic vascular tissue[5,6] similar to a hemangioma or lymphangioma.
Presence of wide capillary-like vessels is the main feature of the disease. It is likely that the blood flow through these vessels is slow, which produces local hypoxia and lowering of the pH, favoring the activity of various hydrolytic enzymes.[4] Strong activity of acid phosphatase and leucine aminopeptidase in mononuclear perivascular cells which are in contact with bone indicates that these cells are important in the process of osseous resorption.[7]
Active hyperemia, changes in local pH and mechanical forces promote bone resorption. Gorham and Stout hypothesized that trauma may trigger the process by stimulating the production of vascular granulation tissue and that “osteoclastosis” is not necessary.[1] Whereas, Devlin et al., have suggested that bone resorption in patients with Gorham disease is due to enhanced osteoclast activity and interleukin 6 plays a role in the increased resorption of bone.[6] Evidence that osteolysis is due to an increased number of stimulated osteoclasts was presented by Moller et al.,[8] Cellular and humoral mechanisms of osteoclast formation and bone resorption was reported by Hirayama et al., which suggested that the increase in osteoclast is not due to an increase in the number of circulating osteoclast precursors, but rather is due to an increase in the sensitivity of these precursors to humoral factors, which promote osteoclast formation and bone resorption.[9] It has also been suggested that thyroid C cells and calcitonin may play an important role in the pathogenesis of Gorham's disease.[10]
CLINICAL FEATURES
Gorham's disease is a rare condition of osteolysis without sex, race, or age predilection; affecting bones in different regions. Based on clinical, histological and radiological features; diagnosis is difficult and requires exclusion of neoplastic, inflammatory, infectious and endocrinologic disease.[11] Disappearing bone disease can be severely disabling and about 16% of cases are fatal. It is usually monocentric, but locally aggressive with resorption of the affected bone extending into adjacent soft tissues.[12] Many investigators believe that massive osteolysis is an aggressive form of skeletal angiomatosis that is related to vascular proliferation and shows regional involvement, frequently involving the shoulder and hip areas[13] and has been termed as hemangiomatosis of bone.[14]
Massive osteolysis has been documented in patients upto 70 years of age, but most affected patients are children and young adults. About 50% of all patients report an episode of trivial trauma before the diagnosis.[14] The most typical presentation is that of osteolysis of a single bone or the bones connected by a shared joint, such as the shoulder. Shoulder is one of the most commonly involved areas, along with the skull and pelvic girdle. The osteolytic process is often painless allowing patients to continue with daily activities. Spontaneous fractures are common and may be the first sign of the disease.[8] Lack of bone healing following fracture is the hallmark of the disease.
In 30% of affected patients, maxillofacial involvement is noted, with the mandible being the most frequently affected jaw bone. Sign and symptoms include mobile teeth, pain, malocclusion, deviation of mandible and clinically obvious facial deformity. Obstructive sleep apnea syndrome has been noted secondary to posterior mandibular displacement after extensive osteolysis. Pathologic fracture of mandible may also occur.[14] Involvement of temporomandibular joint (TMJ) by Gorham disease can be mistaken for TMJ dysfunction.[12]
Although the degree of osseous deformity in patients with massive osteolysis may become severe, serious complications are infrequent. Paraplegia related to spinal cord involvement may occur in patients who have involvement of vertebrae.[15] Thoracic cage, pulmonary or pleural involvement can lead to compromise of respiratory function and death can ensue. Infection of bone and septic shock, though rare, have also been reported.[16]
Heffeze et al., described the criteria for diagnosis of massive osteolysis as:[17]
Minimal or no osteoblastic response and absence of dystrophic calcification;
Positive biopsy for angiomatous tissue;
Absence of cellular atypia;
Evidence of local progressive osseous resorption;
Non-expansile, non-ulcerative lesion;
Absence of visceral involvement;
Osteolytic radiographic pattern;
Negative hereditary, metabolic, neoplastic, immunologic or infectious etiology.
A number of cases in the maxillofacial region present with an initial swelling. Anavi et al., reviewed that the mean duration of symptoms before diagnosis was 6.4 years with the initial histopathological diagnosis inaccurate in 45% of cases, which highlights the difficulty faced by the clinician and the pathologists when attempting to diagnose the condition.[18]
INVESTIGATIONS
The standard laboratory tests are usually within normal limits and do not help in diagnosis of massive osteolysis. The serum alkaline phosphatase level may be slightly elevated.[4]
Radiographs, computed tomography (CT), and magnetic resonance imaging (MRI) have all been used.[1]
During the initial stage of the lesion, radiolucent foci appear in the intramedullary or subcortical regions, resembling findings seen in patchy osteoporosis. Subsequently, slowly progressive atrophy, dissolution, fracture, fragmentation and disappearance of a portion of the bone occur with tapering or “pointing” of the remaining osseous tissue and atrophy of soft tissues.[4] Panoramic radiograph shows resorption and decreased vertical height of the mandibular body with the resorption extended towards the basal bone[1] Figure 1.
Figure 1.

Radiographic image shows radiolucency in 35, 36, 37 and38 region with their displacement and root resorption. The teeth show no bony support. Right side of mandible appears normal (Courtesy: Dong Q, Zhang Y,Sun C, Guo J. Gorham-Stout syndrome affecting the left mandible: A case report.J Exp Therapeut Med 2012:162-4)
Radioisotope bone scan may show increased vascularity on initial images and subsequently, an area of decreased uptake corresponding to the site of diminished or absent osseous tissue. However, these results have been variable.[19]
HISTOPATHOLOGY
The microscopic findings contrast sharply with the striking clinical and radiographic findings. In the early stages, tissue removed from radiolucent defects consists of a nonspecific vascular proliferation intermixed with fibrous connective tissue and a chronic inflammatory cell infiltrate composed of lymphocytes and plasma cells. The vascular proliferation varies in intensity and is characterized by thin-walled channels. Osteoclastic reaction in adjacent bone fragments is usually not conspicuous.[14] According to Johnson and McClure there are two stages: The first with vascular proliferation, followed by a second stage in which residual fibrous tissue replaces resorbed bone[20] [Figure 2].
Figure 2.
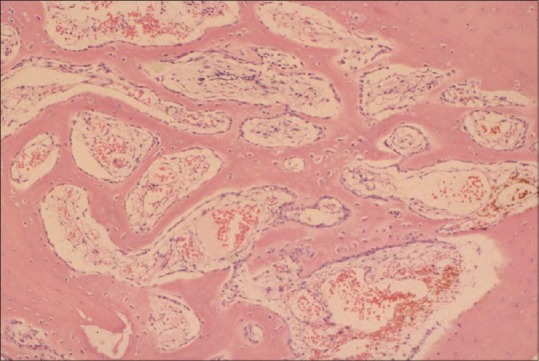
Histopathological image shows vascular proliferation intermixed with fi brous connective tissue and a chronic infl ammatory cell infi ltrate with thinning of bony trabeculae (H&E stain, ×100). (courtesy: www.tumorlibrary.com/case/detail.jsp?image_id=1629)
TREATMENT
Management of Gorham's disease is a challenge for clinicians. The medical treatment for Gorham's disease includes radiation therapy, antiosteoclastic medications (bisphosphonates),[21] and alpha-2b interferon.[22] Surgical options include resection of the lesion and reconstruction using bone grafts and/or prostheses. In most cases, bone grafts tend to undergo resorption and are not helpful. Unfortunately, no single treatment modality has proven effective in arresting the disease. In patients who receive high-dose radiation therapy, the potential for secondary malignancy and growth restriction exists and should be considered before embarking on this mode of treatment.[1]
DIFFERENTIAL DIAGNOSIS
The diagnosis of Gorham's disease should be suspected or made only after excluding other common underlying causes of osteolysis.[12] Aneurysmal bone cyst, extensive metastatic bone disease and osteosarcoma are some of the lesions that resemble vanishing bone disease and can be confirmed with a biopsy.[1]
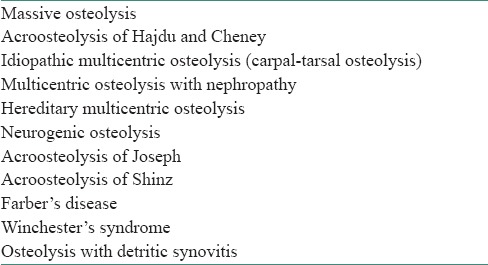
When Gorham's disease involves the mandible, the role of the periodontologist is extremely important. Gorham's disease should be included among the pathologic entities mimicking periodontal disease on radiograph, such as inflammatory disease (e.g. osteomyelitis), endocrine disease (e.g. hyperparathyroidism), intraosseous malignancies or metastases, lymphoma, histiocytosis X, mainly eosinophilic granuloma, infective process (e.g. tuberculosis and actinomycosis) and odontogenic tumors[23] [Table 2].
Table 2.
Differential diagnosis of osteolysis syndromes[24]
CONCLUSION
Gorham's massive osteolysis is one of the five classical types of idiopathic osteolysis. The diagnosis is based on anamnestic data (nonhereditary), biochemical data (absence of nephropathy), radiographical data (progressive monocentric osteolysis without periosteal reaction) and histological data (intraosseous angiomatosis with either capillaries or lymph vessels, or both; eventually fibrosis).[25]
It is a rare musculoskeletal disorder with unknown etiology and nonspecific pathology. It is therefore important for oral pathologists to be aware of its existence as a rare case of osteolysis in maxillofacial skeleton. We believe that disease is not as rare as it seems, but rather remains misdiagnosed.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Kiran DN, Anupama A. Vanishing bone disease: A review. J OralMaxillofac Surg. 2011;69:199–203. doi: 10.1016/j.joms.2010.05.088. [DOI] [PubMed] [Google Scholar]
- 2.Sharma A, Iyer N, Mittal A, Das D, Sharma S. Vanishing mandible. J Oral Sci. 2010;52:513–6. doi: 10.2334/josnusd.52.513. [DOI] [PubMed] [Google Scholar]
- 3.Ravindran R, Karunakaran A. Gorham's disease of the mandible. Case Rep Dent 2013. 2013 doi: 10.1155/2013/723583. 723583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel DV. Gorham's disease or massive osteolysis. Clin Med Res. 2005;3:65–74. doi: 10.3121/cmr.3.2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dickson GR, Hamilton A, Hayes D, Carr KE, Davis R, Mollan RA. An investigation of vanishing bone disease. Bone. 1990;11:205–10. doi: 10.1016/8756-3282(90)90215-k. [DOI] [PubMed] [Google Scholar]
- 6.Devlin RD, Bone HG, Roodman GD. Interleukin-6: A potential mediator of the massive osteolysis in patients with Gorham-Stout disease. J Clin Endocrinol Metab. 1996;81:1893–7. doi: 10.1210/jcem.81.5.8626854. [DOI] [PubMed] [Google Scholar]
- 7.Heyden G, Kindblom LG, Nielsen JM. Disappearing bone disease. A clinical and histological study. J Bone Joint Surg Am. 1977;59:57–61. [PubMed] [Google Scholar]
- 8.Moller G, Priemal M, Amling M, Werner M, Kuhlmey A, Delling G. The Gorham-Stout syndrome (Gorham's massive osteolysis). A report of six cases with histopathological findings. J Bone Joint Surg Br. 1999;81:501–6. doi: 10.1302/0301-620x.81b3.9468. [DOI] [PubMed] [Google Scholar]
- 9.Hirayama T, Sabokbar A, Itonaga I, Watt-Smith S, Athanasou NA. Cellular and humoral mechanisms of osteoclast formation and bone resorption in Gorham-Stout disease. J Pathol. 2001;195:624–30. doi: 10.1002/path.989. [DOI] [PubMed] [Google Scholar]
- 10.Korsic M, Jelasic D, Potocki K, Giljević Z, Aganović I. Massive osteolysis in a girl with agenesis of thyroid C cells. Skeletal Radiol. 1998;27:525–8. doi: 10.1007/s002560050433. [DOI] [PubMed] [Google Scholar]
- 11.Escande C, Schouman T, Françoise G, Haroche J, Ménard P, Piette JC, et al. Histological features and management of a mandibular Gorham disease: A case report and review of maxillofacial cases in the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:e30–7. doi: 10.1016/j.tripleo.2008.02.028. [DOI] [PubMed] [Google Scholar]
- 12.Raghuveer HP, Jayalekshmy R. Gorham's massive osteolysis of themandible-a progressive radiographic presentation. Dentomaxillofac Radiol. 2009;38:292–5. doi: 10.1259/dmfr/73198793. [DOI] [PubMed] [Google Scholar]
- 13.Malik R, Malik R, Tandon S, Tandon P. Skeletal angiomatosis-rare cause of bone destruction: A case report with review of literature. Indian J Pathol Microbiol. 2008;51:515–8. doi: 10.4103/0377-4929.43745. [DOI] [PubMed] [Google Scholar]
- 14.Neville BW, Damn DD, Allen CM, Bouqout JK. 2nd ed. Philadelphia: WB Saunders Co; 2002. Oral and Maxillofacial Pathology; pp. 541–2. [Google Scholar]
- 15.Halliday DR, Dahlin DC, Pugh DG, Young HH. Massive osteolysis and angiomatosis. Radiology. 1964;82:637–44. doi: 10.1148/82.4.637. [DOI] [PubMed] [Google Scholar]
- 16.Kery L, Wouters HW. Massive osteolysis: Report of two cases. J Bone Joint Surg Br. 1970;52:452–9. [PubMed] [Google Scholar]
- 17.Heffez L, Doku HC, Carter BL, Feeney JE. Perspective on massive osteolysis: Report of a case and review of literature. Oral Surg Oral Med Oral Pathol. 1983;55:331–43. doi: 10.1016/0030-4220(83)90185-8. [DOI] [PubMed] [Google Scholar]
- 18.Anavi Y, Sabes WR, Mintz S. Gorhams disease affecting the maxillofacial skeleton. Head Neck. 1989;11:550–7. doi: 10.1002/hed.2880110614. [DOI] [PubMed] [Google Scholar]
- 19.Spieth ME, Greenspan A, Forrester DM, Ansari AN, Kimura RL, Gleason-Jordan I. Gorham's disease of the radius: Radiographic, scintigraphic, and MRI findings with pathologic correlation. A case report and review of the literature. Skeletal Radiol. 1997;26:659–63. doi: 10.1007/s002560050306. [DOI] [PubMed] [Google Scholar]
- 20.Johnson PM, McClure JG. Observations of massive osteolysis: A review of the literature and report of a case. Radiology. 1958;71:28–42. doi: 10.1148/71.1.28. [DOI] [PubMed] [Google Scholar]
- 21.Gutirrrez RM, Spjut HJ. Skeletal angiomatosis: Report of three cases and review of the literature. Clin Orthop Relat Res. 1972;85:82–97. [PubMed] [Google Scholar]
- 22.Hagberg H, Lamberg K, Astrom G. Alpha-2b interferon and oral clodronate for Gorham's disease. Lancet. 1997;350:1822–3. doi: 10.1016/S0140-6736(05)63639-2. [DOI] [PubMed] [Google Scholar]
- 23.Mignogna MD, Fedele S, Lo Russo L, Lanza A, Marenzi G, Sammartino G. Gorham's disease of the mandible mimicking periodontal disease on radiograph. J Clin Periodontol. 2005;32:1022–6. doi: 10.1111/j.1600-051X.2005.00745.x. [DOI] [PubMed] [Google Scholar]
- 24.Resnick D. Osteolysis and chondrolysis. In: Resnick D, editor. Diagnosis of bone and jiont disorders. 4thed. Philadelphia: W.B.Saunders Co; 2002. p. 4920. [Google Scholar]
- 25.van der Linden-van der Zwaag H, Onvlee GJ. Massive osteolysis (Gorham's disease) affecting the femur. Acta Orthop Belg. 2006;72:261–8. [PubMed] [Google Scholar]


