Abstract
Purpose
To characterize the urologic symptoms of a subset of urologic chronic pelvic pain syndrome (UCPPS) patients who have both a high somatic symptom burden and a wide symptom distribution fitting a “poly-symptomatic, poly-syndromic” (PSPS) pattern of presentation.
Materials and Methods
81 UCPPS patients enrolled in the NIDDK MAPP Research Network Study at the Washington University in St. Louis and the University of Alabama at Birmingham sites completed a symptom questionnaire to assess their somatic symptom burden and its distribution, the Genitourinary Pain Index (GUPI) to assess their UCPPS symptoms and impact on quality of life, and self-reported treatment-seeking behaviors for their UCPPS symptoms. The PSPS symptom pattern was defined as self-report of numerous painful and non-painful somatic symptoms across many organ systems and symptom categories on the PSPS questionnaire.
Results
UCPPS patients with the PSPS pattern reported more severe genitourinary pain on a Likert scale, more frequent pain in the past week, and more widespread distribution of the pain in the genital and pelvic areas compared to UCPPS patients without PSPS. PSPS patients also had significantly higher scores on the pain subscale, quality of life subscale (worse), and the total scores on the GUPI questionnaire than patients without PSPS. Patients with the PSPS pattern reported significantly more treatment-seeking behaviors than other patients.
Conclusion
The PSPS pattern might be an important phenotypic factor to assess in the evaluation of UCPPS with clinical and research implications. This may be a distinct clinical subgroup among UCPPS patients.
Keywords: interstitial cystitis, chronic prostatitis, somatic symptoms
Introduction
Patients with urologic chronic pelvic pain syndrome (UCPPS), which includes interstitial cystitis/bladder pain syndrome (IC/BPS) or chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS), commonly report bothersome symptoms outside the genitourinary tract. These extra-pelvic symptoms may be painful (e.g., abdominal pain) or non-painful (e.g., numbness, dizziness, palpitation).1, 2 We have previously shown that about one out of four UCPPS patients reported numerous somatic symptoms in a classic “poly-symptomatic, poly-syndromic” (PSPS) pattern of presentation.3 The defining features of PSPS are that patients complain of numerous symptoms that are also widely distributed across multiple organ systems.4-11 The poly-symptomatic group reports both pain and non-painful symptoms.
Currently it is unclear if patients with the PSPS pattern might represent a phenotypically distinct subgroup of the UCPPS population, different from patients without the PSPS pattern (i.e., those with more focused, non-systemic complaints). There is evidence in the literature that high somatic symptom burden in IBS patients is associated with significantly greater numbers of gastrointestinal symptoms, psychiatric disorders, physicians consulted, telephone calls to physicians, urgent care visits, medication changes, missed worked days, and higher total health care costs compared to other IBS patients.12-14 The objective of this study was to characterize the urologic symptoms of a subset of UCPPS patients who have both a high somatic symptom burden and a wide symptom distribution fitting a PSPS pattern of presentation. Specifically, we compared the severity of UCPPS pain, frequency of pain, quality of life, and treatment-seeking behaviors between UCPPS participants with and without the PSPS pattern.
Materials and Methods
Study population and design
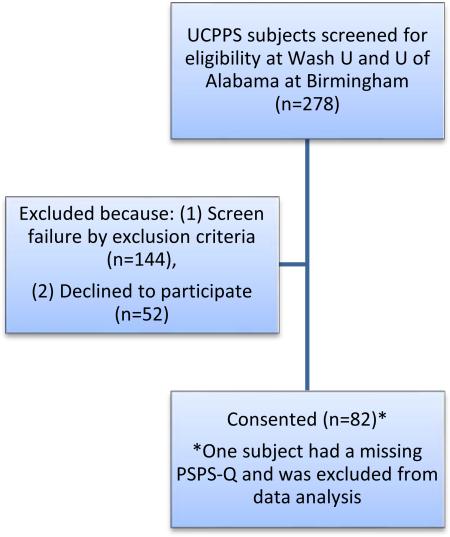
81 UCPPS patients enrolled in the NIDDK MAPP (Multi-disciplinary Approach to the Study of Chronic Pelvic Pain) Research Network Study at Washington University in St Louis and the University of Alabama between March 2010 and December 2012 completed the following questionnaires during their baseline research visit, including: (1) PSPS-Q symptom measure,3 (2) the Genitourinary Pain Index (GUPI) questionnaire,15 as well as (3) questions about self-reported treatment-seeking behaviors over the past two weeks. The inclusion and exclusion criteria are listed in Table 1. An enrollment flow chart is presented in Appendix B. Patient demographics are presented in Table 2. The study was approved by the institutional review boards.
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria: |
| (1) males or females at least 18 years of age |
| (2) ability to provide written, informed consent |
| (3) a response of at least 1 on a pain, pressure or discomfort scale (0 to 10) perceived to be related to the bladder/prostate and/or pelvic region |
| (4) fulfilled one of the following MAPP symptom criteria (IC/BPS and/or CP/CPPS): |
| To meet the MAPP IC/BPS symptom criteria, males* or females had to report an unpleasant sensation of pain, pressure or discomfort, perceived to be related to the bladder and/or pelvic region, associated with lower urinary tract symptoms. The IC/BPS symptoms must be present for the majority of the time during any 3 months in the previous 6 months, and have been present for the majority of the time during the most recent 3 months. |
| To meet the MAPP CP/CPPS symptom criteria (males* only), males had to report pain or discomfort in any of the 8 Male Genitourinary Pain Index (GUPI) pain domains. In addition, these CP/CPPS symptoms had to have been present for the majority of the time during any 3 months in the previous 6 months. |
|
*Males may enter the MAPP study through IC/BPS and/or CP/CPPS symptom criteria.
|
| Exclusion criteria: |
| (1) on-going symptomatic urethral stricture, (2) on-going neurological disease or disorder affecting the bladder, (3) bowel fistula, (4) a history of cystitis caused by tuberculosis, radiation therapy, or cytoxan/cyclophosphamide therapy, (5) augmentation cystoplasty or cystectomy, (6) a history of cancer except skin cancer, (7) active Crohn's disease, ulcerative colitis, systemic lupus erythematosis, rheumatoid arthritis, multiple sclerosis, human immunodeficiency virus infection, (8) current major psychiatric disorder or medical issues that would interfere with study participation (e.g. dementia, psychosis, upcoming major surgery), (9) severe cardiac, pulmonary, renal, or hepatic disease that in the physician's judgment would preclude participation. Males were also excluded for: (10) unilateral orchalgia without pelvic symptoms, (11) history of transurethral microwave thermotherapy, transurethral needle ablation or balloon dilation of the prostate, prostate cryosurgery, or laser prostate procedure. |
| Deferral criteria: |
| (1) definitive treatment for acute epididymitis, urethritis or vaginitis in the past 3 months, (2) unevaluated hematuria, (3) a history of prostate biopsy or transurethral resection of the prostate in the past 3 months, (4) positive urine pregnancy test. |
Table 2.
Patient demographics
| UCPPS with PSPS | UCPPS without PSPS | p-value | ||
|---|---|---|---|---|
| No. of participants (%) | 24 (30%) | 57 (70%) | ||
| Sex | Female | 19 (79%) | 29 (51%) | 0.025* |
| Male | 5 (21%) | 22 (49%) | ||
| Race | White | 24 (100%) | 50 (88%) | 0.098 |
| Black | 0 (0%) | 7 (12%) | ||
| Others | 0 (0%) | 0 (0%) | ||
| Ethnicity | Hispanic | 1 (4%) | 5 (9%) | 0.66 |
| Non-Hispanic | 23 (96%) | 52 (91%) | ||
| Mean age (SD) | 42.8 (14.3) | 49.1 (15.8) | 0.096 | |
| Mean duration of UCPPS symptoms in years (SD) | 9.1 (12.6) | 15.5 (12.8) | 0.163 | |
| Mean age of UCPPS symptom onset (SD) | 33.8 (17.6) | 35.0 (16.8) | 0.782 | |
| Interstitial cystitis symptom index, ICSI (SD) | 11.7 (5.1) | 8.8 (5.0) | 0.048* | |
| Interstitial cystitis problem index, ICPI (SD) | 10.3 (4.0) | 7.4 (4.6) | 0.026* | |
| Medications (no. of participants) | Elmiron | 12 | 19 | |
| Tricyclics | 11 | 16 | ||
| Antihistamines | 3 | 8 | ||
| Muscle relaxants | 3 | 2 | ||
| Narcotics | 5 | 3 | ||
| NSAIDs | 4 | 7 | ||
| Antiepileptics | 2 | 5 |
The MAPP Research Network represents an interdisciplinary approach to study UCPPS. The network includes six discovery sites that conduct the research studies and two core sites that coordinate data collection, analyze tissue samples, and provide technical support. The somatic symptom measure (described below) was only administrated to MAPP participants at the Washington University in St Louis and the University of Alabama sites, thus only participants from those two sites were included in this report.
Assessment
The somatic symptom measure (PSPS questionnaire) consists of 59 self-reported symptom items that assess patients’ somatic symptom burden and its distribution (see Appendix A). Information about this instrument is provided in a previous publication describing the successful utilization of this instrument with UCPPS patients.3 The items in this questionnaire were derived from the Perley-Guze symptom checklist used to characterize somatization and Briquet's disorder. To be consistent with Perley-Guze's original description of a poly-symptomatic presentation affecting multiple organ systems,5, 6, 8-11 we have defined the PSPS symptom pattern as self-report of 25 or more somatic symptoms in 9 or more symptom categories on the PSPS questionnaire for females. Because males cannot have gynecologic symptoms (group 7 in the questionnaire, see Appendix A), PSPS symptom presentation was operationalized as having 21 or more symptoms in 8 or more symptom categories for males. Participants with the PSPS symptom pattern have both high somatic symptom burden and wide symptom distribution.
The Genitourinary Pain Index (GUPI) questionnaire was used to assess their UCPPS symptoms and impact on quality of life in the past week.15 The GUPI has been previously validated and has specifically been demonstrated to have discriminant validity, concurrent validity and reliability, and it has been externally validated through correlation with response to therapy.15 It queries the location of pain (for males: pain or discomfort in the perineum, testicles, tip of the penis, or below the waist in the pubic or bladder areas; for females: entrance to vagina, vagina, urethra, or below the waist in the pubic or bladder areas), characteristics of the pain (pain or discomfort as the bladder fills, relieved by voiding, during urination, or during/after sex), frequency of pain over the last week, associated urinary symptoms, and quality of life assessment. The GUPI contains several subscales (pain, urinary, quality of life) and a total GUPI score.
Participants were also asked to provide information about self-reported treatment-seeking behaviors over the past two weeks. The specific questions asked were: Have your urologic or pelvic pain symptoms been severe enough that they caused you to do the followings in the past 2 weeks (yes or no response to each question): (1) contacted a healthcare provider by telephone or e-mail, (2) seen a provider in his/her office, (3) made a trip to the emergency room or urgent care center, (4) had your medication changed, (5) undergone a medical procedure?
Statistical Analysis
Statistical analysis was performed using SAS® 9.2 software (SAS Institute, Cary, NC). Chi-square tests were conducted for dichotomous variables, substituting Fisher's exact tests for expected cell sizes <5. Multiple regression equations were conducted to compare numeric symptom variables between groups controlling for sex. Correlations were used to compare two numeric variables. An alpha value of p<0.05 was chosen to define statistical significance (two-tailed tests).
Results
24 out of 81 (30%) UCPPS participants had PSPS presentation characterized by both high somatic symptom burden and wide symptom distribution. In terms of demographics (Table 2), more UCPPS patients with the PSPS pattern were female compared to those without PSPS (80% versus 51%). UCPPS patients with PSPS also had higher interstitial cystitis symptom index and problem index scores. There was no difference between the PSPS group and the other patients in terms of patient age, age of onset, duration of UCPPS symptoms, race, or ethnicity.
As shown in Table 3, UCPPS patients with the PSPS pattern reported more severe genitourinary pain on a 0 to 10 Likert scale, more frequent pain in the past week, and more widespread distribution of the pain in the genital and pelvic areas compared to UCPPS patients without PSPS (after correction for sex difference). PSPS patients also had significantly higher scores on the pain subscale, quality of life subscale (poorer QOL), and the total scores on the GUPI questionnaire than patients without PSPS.
Table 3.
Severity of UCPPS symptoms
| UCPPS with PSPS N=24 Mean (SD) | UCPPS without PSPS N=57 Mean (SD) | p-value, corrected for sex | |
|---|---|---|---|
|
Pain rating: What number best describes your average pain or discomfort on the days that you had it, over the last week? (0 to 10 Likert scale) |
6.3 (2.1) | 5.0 (2.3) | 0.040 |
|
Pain frequency: How often have you had pain or discomfort in any of these areas over the last week? (0=never, 1=rarely, 2=sometimes, 3=often, 4=usually, 5=always) |
3.8 (1.2) | 2.8 (1.3) | 0.040 |
|
Pain distribution: Sum of the first 8 pain-related questions on GUPI questionnaire.* Higher number is consistent with more widespread distribution of the pain in the genital and pelvic areas (maximum of 8). |
5.6 (2.0) | 3.9 (1.9) | 0.008 |
| GUPI pain subscale | 15.7 (4.6) | 11.7 (4.5) | 0.006 |
| GUPI urinary subscale | 6.3 (2.6) | 4.4 (2.7) | 0.070 |
| GUPI quality of life subscale** | 9.2 (2.5) | 6.9 (2.8) | 0.003 |
| GUPI total score | 31.2 (8.6) | 23.0 (8.5) | 0.003 |
|
Self-reported treatment-seeking behaviors: Have your urologic or pelvic pain symptoms been severe enough that they caused you to do any of the followings in the past 2 weeks?*** (maximum of 5) |
1.0 (1.3) | 0.5 (0.9) | 0.040 |
In the last week, have you experienced any pain or discomfort in the following areas? (for males: in the perineum, testicles, tip of the penis, or below the waits in the pubic or bladder areas; for females: entrance to vagina, vagina, urethra, or below the waist in the pubic or bladder areas). In the last week, have you experienced: (1) Pain or burning during urination? (2) Pain or discomfort during or after sexual intercourse? (3) Pain or discomfort as your bladder fills? (4) Pain or discomfort relieved by voiding?
(1) How much have your symptoms kept you from doing the kinds of things you would usually do, over the last week? (0=none, 1=only a little, 2=some, 3=a lot). (2) How much did you think about your symptoms, over the last week? (0=none, 1=only a little, 2=some, 3=a lot). (3) If you were to spend the rest of your life with your symptoms just the way they have been during the last week, how would you feel about that? (0=delighted, 1=pleased, 2=mostly satisfied, 3=mixed, 4=mostly dissatisfied, 5=unhappy, 6=terrible).
(1) Contacted a healthcare provider (physician, nurse, physical therapist or other provider) by telephone or e-mail? (2) Seen a healthcare provider in his/her office? (3) Made a trip to an emergency room or urgent care center? (4) Had a medication changed (new medication or different dose)? (5) Undergone a medical procedure?
The sum of recent self-reported treatment-seeking behaviors (e.g., contacted a healthcare provider by telephone or e-mail, saw a provider in the office, made a trip to an emergency room or urgent care center, had a medication change in the past two weeks) was higher among UCPPS patients with the PSPS pattern than in other patients.
Discussion
UCPPS is a heterogeneous syndrome with diverse clinical presentations. Some patients have predominantly urinary symptoms, some have symptoms restricted to the pelvis and lower abdomen, and one-fourth have widespread somatic symptoms involving many organ systems.3 It is likely that this syndrome has a multifactorial etiology that prevents an intervention with a single etiologically-based mechanism to achieve positive outcomes in clinical trials.16 Thus a critical research priority is to stratify the UCPPS population into clinically distinct phenotypes, with the goal of being able to target treatments based on patient-specific phenotypic features and pathophysiology.17, 18
This study identified a subset of UCPPS patients with a PSPS pattern of systemic symptom presentation. Patients with the PSPS pattern reported more frequent and severe genitourinary pain, more widespread distribution of the pain within the genital and pelvic areas, poorer quality of life, and more self-reported treatment-seeking behaviors compared to patients without PSPS. The difference in total mean GUPI scores between patients with and without PSPS was about 8 points, a statistically significant difference. A 4-point change in total GUPI score has previously been shown to be associated with a clinically significant change in symptoms that can be perceived by patients.15 Data from this study suggested that the PSPS pattern, which is characterized by both high somatic symptom burden and wide symptom distribution, should be considered in the clinical phenotyping of UCPPS. The PSPS Questionnaire (Appendix A) may have clinical utility as a screening tool to identify patients with the PSPS pattern in about five minutes.
In the multi-institutional MAPP study, Krieger et al showed that UCPPS patients who have an additional non-urologic co-morbid syndromes such as irritable bowel syndrome (IBS), fibromyalgia (FM) or chronic fatigue syndrome (CFS) reported more severe urologic symptoms, worse quality of life, and more depression and anxiety compared to patients without the co-morbid pain syndromes.19 The PSPS patients identified in this study also have “systemic symptom presentation.” However, our PSPS group were conceptually different because PSPS patients reported both pain and non-painful symptoms across multiple organ systems, unlike co-morbid pain syndromes (e.g. IBS) which only focus on pain in one of the organ systems of interest (e.g. in the gastrointestinal tract). Even though the operational definition of “systemic symptom presentation” was different between the Krieger study and the current study, the findings of the two studies are complimentary, i.e., UCPPS patients with systemic symptom presentation have more severe symptoms and decreased quality of life compared to those with primarily pelvic symptoms.
This study's identification of a subset of UCPPS patients with a PSPS pattern of presentation is strikingly similar to a subset of IBS patients previously found to have a high somatic symptom burden and wide symptom distribution.12, 20 This pattern of symptom presentation in the IBS patients was found to be associated with severity and frequency of gastrointestinal symptoms, poorer quality of life, less treatment adherence, greater utilization of health care resources, and higher total health care costs.12-14, 20
Historically, functional pain researchers have concentrated on functional pain presentations with a focus on the organ system of interest. Other researchers have suggested that these functional pain symptoms are dynamic and have wide distribution in other organ systems. The PSPS concept encompasses both aspects of the behaviors of these symptoms to consider not only multiple symptoms of both pain and non-pain character that are distributed beyond the organ system of interest throughout all the body's organ systems. Because the PSPS pattern is defined by both high symptom burden and wide symptom distribution, this concept brings these two approaches to these syndromes together in one all-encompassing model. The PSPS concept may facilitate better coordination of care for these patients among their healthcare providers.
Intuitively, in the PSPS pattern subgroup, it may not make sense to focus the management on the “peripheral” end organs alone (e.g., with intravesical instillation, physiotherapy, or pentosan polysulfate). Addressing the lead pelvic symptoms might not ameliorate the global suffering of patients with the PSPS pattern. Classifying the heterogeneous UCPPS population into phenotypic subgroups based on PSPS symptom burden can facilitate the management of patients with these complex presentations. These patients need a specialized care plan designed for patients with PSPS presentations (see Table 4 for a concise summary).6 Treatment is orchestrated by a single physician who develops a therapeutic alliance with the patient and follows the patient on a regular basis.21, 22 The aim is to protect the patient from iatrogenic morbidity from unnecessary medical treatments and procedures and to support the patient in developing healthy coping behaviors and making optimal decisions. It is possible that UCPPS patients with the PSPS pattern might be especially challenging to manage because of: (i) more severe pain/symptoms, (ii) more widespread symptom distribution, and (iii) more importantly, the pathophysiology that underlies the PSPS presentation is poorly understood.
Table 4.
A primer for managing patients with PSPS (based on North et al 2010)6
| • Treatment is orchestrated by a single physician who develops a therapeutic alliance with the patient and follows the patient on a regular basis. The aim is to protect the patient from iatrogenic morbidity from unnecessary medical procedures and to support the patient in developing healthy coping behaviors and making optimal decisions. |
| • Success will depend on winning the patient's confidence without allowing her symptomatic behavior to exhaust the physician's sympathy. |
| • The physician should strive to discuss the patient's life problems, concerns, and goals achievement rather than simply ordering additional tests and X- rays or yet another medication or more surgery without objective indications of their necessity. |
| • The most frequent complications are repeated surgical procedures (with its comorbidities), drug dependence, martial instability, and suicidal attempts. Avoid surgery, other invasive procedures, and medications that are potentially dangerous or with abuse potential unless clearly indicated based on objective signs, symptoms, and sufficient diagnostic evaluation. |
| • Cognitive behavioral therapy appears to be effective based on a review of published randomized, controlled trials.24 Other types of psychotherapy or counseling might be helpful and a referral to a clinical psychologist or other mental health professional maybe indicated. |
| • Psychiatric consultation may be helpful in reducing the extent and cost of medical care based on a controlled, randomized study.25 Some patients may be reluctant to consult a psychiatrist, but psychotropic medications may help to alleviate the symptoms of depression and anxiety. One-time diagnostic evaluation by a psychiatrist may be helpful to provide guidance to the treating physician. |
The PSPS perspective has much to offer to clinical interventional research as well as clinical practice. Previous research has found that patients with the PSPS pattern have poorer clinical outcomes.12, 23 The PSPS pattern cannot be assumed to be a specific medical condition or a psychiatric disorder. The etiology of this symptom pattern is unknown. Lack of attention to this important subset of patients in the sample may diminish the clinical response, obscure findings on treatment efficacy, and increase the difficulty in conducting the research.12 Research studies thus need to account for patients with the PSPS pattern in the analysis of the data. This does not necessarily mean excluding these patients from studies, but identifying them and controlling for their presence in the sample or by analyzing their data separately from the rest of the UCPPS patients. Because patients with the PSPS pattern require different approaches to their management, research on treatments for them need to be individualized for patients with their presentation.
As shown in Table 2, more UCPPS patients with the PSPS pattern were females compared to other patients (80% versus 51%). One finding is a significant difference concerning females in both subsamples. The results presented in Table 3 were already corrected for the sex difference. But still the question was whether the observations applied to UCPPS males. We did not perform a sex-specific comparison (male PSPS vs. male without PSPS) because the number of males with PSPS in our cohort was too small (5 individuals) to make a confident comparison. Targeting more male UCPPS participants in future studies would permit further examination of PSPS in either gender.
This study was not without some methodological limitations. The questionnaires covered only a shorter time frame and thus did not capture the longer course of symptom progression or regression. The health seeking behavior questions only solicited a “yes or no” response from participants in the past two weeks. The data reported in the present study was based on the values from the baseline visit when the PSPS-Q was also administrated concurrently. In future studies, we will analyze the MAPP longitudinal dataset to provide additional insights on health seeking behaviors over time. Even though PSPS patients have higher QOL subscale scores on the GUPI (implying poorer QOL), the GUPI QOL questions were not adequate to fully assess the impact on QOL. Additional validated QOL questionnaires such as SF-12 or SF-36 should be used in future studies, and conclusions about QOL based on GUPI questions should be interpreted judiciously.
Although the symptom questionnaire measured the PSPS presentation that is characteristic of somatization disorder, the specific instrument used in the study has not been validated for making the diagnosis of somatization disorder in this study population. Undoubtedly there may be some overlap, and research is needed to compare the PSPS algorithm used for this study with measures of somatization disorder criteria to fully explicate their relationship.
Conclusion
Participants with the poly-symptomatic, poly-syndromic (PSPS) pattern of presentation, characterized by both high somatic symptom burden and wide symptom distribution, reported more severe genitourinary pain, more frequent pain in the past week, more widespread distribution of the pain within the genital and pelvic areas, poorer quality of life, and more treatment-seeking behaviors compared to patients without PSPS. The data suggest that the PSPS pattern of symptom presentation might be an important phenotypic factor to assess in the clinical phenotyping of UCPPS.
Acknowledgement
We would like to thank Vivien Gardner, Rebecca Bristol and Alexandra Klim for recruitment of participants, and Drs. Gregory S. Sayuk and David H. Alpers at Washington University School of Medicine for critical review of the manuscript.
Funding:
The project described was supported by Award Number U01DK082315 (Multi-disciplinary Approach to the Study of Chronic Pelvic Pain MAPP Research Network) from the National Institute of Diabetes and Digestive and Kidney Diseases. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the National Institutes of Health.
Abbreviations
- CP/CPPS
chronic prostatitis/chronic pelvic pain syndrome
- GUPI
genitourinary pain index
- PSPS
poly-symptomatic, poly-syndromic
- IC/BPS
interstitial cystitis/bladder pain syndrome
- IBS
irritable bowel syndrome
- FM
fibromyalgia
- CFS
chronic fatigue syndrome
- UCPPS
urologic chronic pelvic pain syndrome
Appendix A: PSPS-Q (Poly-symptomatic Poly-syndromic Questionnaire)
For the following symptom list, we would like to know if you have ever had a lot of trouble with the symptom (circle Yes or No).
Group 1:
Headache
Feeling generally sick
Group 2:
Blindness
Paralysis
Numbness and tingling (anesthesia)
Inability to speak (aphonia)
Convulsions or seizures
Unconsciousness
Amnesia (periods of time without memory)
Deafness
Hallucinations (e.g. seeing visions, hearing voices)
Difficulty urinating
Trouble walking
Other conversion symptoms (e.g. any unusual spells)
Group 3:
Fatigue
Lump in throat or inability to swallow
Fainting spells
Blurred vision (not just due to needing glasses)
Unexplained weakness of body or limbs
Painful urination
Group 4:
Breathing difficulty
Palpitation or irregular heartbeat
Anxiety attacks
Chest pain
Dizziness (without fainting)
Group 5:
Lack of appetite (anorexia)
Unintentional weight loss
Marked fluctuation in weight
Nausea
Abdominal bloating
Inability to tolerate several kinds of food
Diarrhea
Constipation
Group 6:
Abdominal pain
Vomiting
Group 7: (* not applicable to males)
Painful menstruation (dysmenorrhea)
Menstrual irregularities
Amenorrhea (don't count menopause)
Excessive bleeding with menstrual periods
Group 8:
Loss of interest in sex
Frigidity or impotence
Painful sexual intercourse (dyspareunia)
Other difficulties with sex or sexual organs
Vomiting all 9 months of pregnancy or hospitalized for vomiting during pregnancy
Group 9:
Back pain
Joint pain without swelling or redness in more than 1 joint
Painful extremities (limbs, hands, feet, not counting joints)
Burning pain of the sexual organs or rectum
Other bodily pains
Group 10:
Nervousness
Fears
Depressed feelings
Need to quit work or inability to carry regular duties because of feeling sick
Crying easily
Feeling life is hopeless
Thinking a good deal about dying
Wanting to die
Thinking of suicide
Suicidal attempts
Appendix
Appendix B: Enrollment flow chart
Reference
- 1.Clauw DJ, Schmidt M, Radulovic D, et al. The relationship between fibromyalgia and interstitial cystitis. J Psychiatr Res. 1997;31:125. doi: 10.1016/s0022-3956(96)00051-9. [DOI] [PubMed] [Google Scholar]
- 2.Erickson DR, Morgan KC, Ordille S, et al. Nonbladder related symptoms in patients with interstitial cystitis. J Urol. 2001;166:557. [PubMed] [Google Scholar]
- 3.Lai HH, North CS, Andriole GL, et al. Polysymptomatic, polysyndromic presentation of patients with urological chronic pelvic pain syndrome. J Urol. 2012;187:2106. doi: 10.1016/j.juro.2012.01.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Diagnostic and Statistical Manual of Mental Disorders. 4th Edition, Text Revision ed. American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- 5.Feighner JP, Robins E, Guze SB, et al. Diagnostic criteria for use in psychiatric research. Arch Gen Psychiatry. 1972;26:57. doi: 10.1001/archpsyc.1972.01750190059011. [DOI] [PubMed] [Google Scholar]
- 6.North CS, Yutzy SH. Somatization Disorder. In: Goodwin DW, North CS, Yutzy SH, editors. Goodwin and Guze's Psychiatric Diagnosis. 6th Ed ed. Oxford University Press; New York, NY: pp. 207–225, 2010. [Google Scholar]
- 7.Perley MJ, Guze SB. Hysteria--the stability and usefulness of clinical criteria. A quantitative study based on a follow-up period of six to eight years in 39 patients. N Engl J Med. 1962;266:421. doi: 10.1056/NEJM196203012660901. [DOI] [PubMed] [Google Scholar]
- 8.Woodruff RA, Jr., Clayton PJ, Guze SB. Hysteria: an evaluation of specific diagnostic criteria by the study of randomly selected psychiatric clinic patients. Br J Psychiatry. 1969;115:1243. doi: 10.1192/bjp.115.528.1243. [DOI] [PubMed] [Google Scholar]
- 9.Yutzy SH, Parish BS. Somatoform Disorders. In: Hales RE, Yudofsky SC, Gabbard GO, editors. The American Psychiatric Publishing Textbook of Psychiatry. 5th ed ed. American Psychiatric Pub; Washington DC: pp. 609–642, 2008. [Google Scholar]
- 10.Guze SB. The diagnosis of hysteria: what are we trying to do? Am J Psychiatry. 1967;124:491. doi: 10.1176/ajp.124.4.491. [DOI] [PubMed] [Google Scholar]
- 11.Woodruff RA., Jr. Hysteria: an evaluation of objective diagnostic criteria by the study of women with chronic medical illnesses. Br J Psychiatry. 1968;114:1115. doi: 10.1192/bjp.114.514.1115. [DOI] [PubMed] [Google Scholar]
- 12.North CS, Downs D, Clouse RE, et al. The presentation of irritable bowel syndrome in the context of somatization disorder. Clin Gastroenterol Hepatol. 2004;2:787. doi: 10.1016/s1542-3565(04)00350-7. [DOI] [PubMed] [Google Scholar]
- 13.Creed F, Tomenson B, Guthrie E, et al. The relationship between somatisation and outcome in patients with severe irritable bowel syndrome. J Psychosom Res. 2008;64:613. doi: 10.1016/j.jpsychores.2008.02.016. [DOI] [PubMed] [Google Scholar]
- 14.Sayuk GS, Elwing JE, Lustman PJ, et al. High somatic symptom burdens and functional gastrointestinal disorders. Clin Gastroenterol Hepatol. 2007;5:556. doi: 10.1016/j.cgh.2006.11.024. [DOI] [PubMed] [Google Scholar]
- 15.Clemens JQ, Calhoun EA, Litwin MS, et al. Validation of a modified National Institutes of Health chronic prostatitis symptom index to assess genitourinary pain in both men and women. Urology. 2009;74:983. doi: 10.1016/j.urology.2009.06.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shoskes DA, Nickel JC, Kattan MW. Phenotypically directed multimodal therapy for chronic prostatitis/chronic pelvic pain syndrome: a prospective study using UPOINT. Urology. 2010;75:1249. doi: 10.1016/j.urology.2010.01.021. [DOI] [PubMed] [Google Scholar]
- 17.Nickel JC, Shoskes D, Irvine-Bird K. Clinical phenotyping of women with interstitial cystitis/painful bladder syndrome: a key to classification and potentially improved management. J Urol. 2009;182:155. doi: 10.1016/j.juro.2009.02.122. [DOI] [PubMed] [Google Scholar]
- 18.Shoskes DA, Nickel JC, Rackley RR, et al. Clinical phenotyping in chronic prostatitis/chronic pelvic pain syndrome and interstitial cystitis: a management strategy for urologic chronic pelvic pain syndromes. Prostate Cancer Prostatic Dis. 2009;12:177. doi: 10.1038/pcan.2008.42. [DOI] [PubMed] [Google Scholar]
- 19.Krieger JN, Stephens A, Landis JR, et al. Non-urologic syndromes and severity of urological pain symptoms: Baseline evaluation of the National Institutes of Health Multidisciplinary Approach to Pelvic Pain Study. J Urol. 2013;189:e181. [Google Scholar]
- 20.North CS, Hong BA, Alpers DH. Relationship of functional gastrointestinal disorders and psychiatric disorders: implications for treatment. World J Gastroenterol. 2007;13:2020. doi: 10.3748/wjg.v13.i14.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Monson RA, Smith GR., Jr. Current concepts in psychiatry. Somatization disorder in primary care. N Engl J Med. 1983;308:1464. doi: 10.1056/NEJM198306163082407. [DOI] [PubMed] [Google Scholar]
- 22.Martin RL. Problems in the diagnosis of somatization disorder: effects on research and clinical practice. Psychiat Ann. 1988;18:357. [Google Scholar]
- 23.Sayuk GS, Elwing JE, Lustman PJ, et al. Predictors of premature antidepressant discontinuation in functional gastrointestinal disorders. Psychosom Med. 2007;69:173. doi: 10.1097/PSY.0b013e318031391d. [DOI] [PubMed] [Google Scholar]
- 24.Kroenke K. Efficacy of treatment for somatoform disorders: a review of randomized controlled trials. Psychosom Med. 2007;69:881. doi: 10.1097/PSY.0b013e31815b00c4. [DOI] [PubMed] [Google Scholar]
- 25.Smith GR, Jr., Monson RA, Ray DC. Psychiatric consultation in somatization disorder. A randomized controlled study. N Engl J Med. 1986;314:1407. doi: 10.1056/NEJM198605293142203. [DOI] [PubMed] [Google Scholar]