Abstract
Objective
To assess the association of insurance status on infant rehospitalization in a population-based setting.
Methods
In this longitudinal retrospective study, hospitalizations were tracked for one year after birth discharge for 203,031 infants born in hospitals during 2008 using data from the New York State Inpatient Database. Relative risk was estimated using multivariable negative binomial regression models.
Results
Rehospitalization occurred in 9,010 infants (4.4%). Medicaid coverage and being uninsured were strong predictors of rehospitalizations after adjustment for birth weight and other factors. Medicaid also bears a disproportionate share of the economic burden. Normal birth weight infants have the lowest risk, but comprise the majority of costs. Jaundice and acute bronchiolitis were the leading causes of rehospitalization within 30 days and one year, respectively.
Discussion
Future research can explore the preventability of rehospitalizations, and evaluate novel strategies for discharge and postnatal care coordination especially for uninsured and Medicaid-enrolled infants.
Keywords: Readmission, Infants, Insurance, Medicaid, Risk Factors, Cost
INTRODUCTION
Reducing rehospitalizations is important in order to improve the quality of health care and lower costs, and is also a key component of the Affordable Care Act.1,2 While most attention has been focused on the elderly Medicare population, rehospitalizations have also been shown to be common and costly in children and youth.3–8 However, less is known about rehospitalizations during early infancy. Earlier studies have found associations between increased rehospitalization and low birth weight/prematurity, Black race, urban residence, and low maternal socioeconomic status.4–10 However, many of these previous analyses addressed primarily infants in specific health plans or hospital systems, or on subsets of infants such as those born preterm. An analysis of readmission in 15 states found Medicare and Medicaid to be associated with higher risk-adjusted readmission rates compared to those with private insurance in the general population, but this same study found no difference between Medicaid and private insurance for pediatrics age 1 to 17.11 To our knowledge, there are few large population-based studies that focus on rehospitalizations among infants in the first year after birth discharge and none that focus on the impact of insurance status in diverse multi-payer, all-birth weight populations.
The aim of this study was to examine the association of insurance as a risk factor for rehospitalizations in the first year after birth discharge in a large contemporary ethnically diverse population that encompasses all birth weights and all payer types. We hypothesized that Medicaid insurance is an independent predictor of increased risk of rehospitalization. We also described the impact of insurance status on the extent, causes, and costs of these rehospitalizations.
METHODS
Data Source
We conducted a longitudinal retrospective study using administrative hospitalization data from the 2008 and 2009 New York State Inpatient Database (SID). The SID, part of the Healthcare Cost & Utilization Project (HCUP) sponsored by the Agency for Healthcare Research & Quality, includes the universe of discharges for all inpatient stays in non-government hospitals. The SID carries clinical and non-clinical information on all patients including age, sex, race, insurance status, length of stay, discharge status, and ICD-9-CM diagnostic and procedure codes.12 The SID has several strengths including a large multi-ethnic population in addition to availability of comprehensive data on patients with all insurance types. The New York SID is an ideal database for this study in that it has an HCUP-generated synthetic patient identifier that allows revisit analysis, and this identifier has been verified in a large percentage (85.3% in 2008) of the infant population.13 The New York SID also has the birth weight measured in grams recorded for all newborns.
Study population – inclusion and exclusion criteria
The study population included all infants born alive in hospitals within the state of New York during 2008. The population was identified using admission type and hospital birth flag variables included in the database. Subjects with missing synthetic patient identifiers (N=32,569 records; 13.4%) and those that died in-hospital before discharge (N=645, 0.3%) were excluded. These excluded patients had similar birth weight, LOS, and costs as the study population, but they were more likely to be Hispanic (32% vs. 14% in the study population, p<.001) and female (57% vs. 51%, p<.001) and less likely to be White (28% vs. 50%, p<.001). Newborns with birth weight less than 500 grams (N=15; 0.1%), and those listed as having “Medicare” or “other” insurance (n=4,069; 2.0%) on the discharge record were excluded. Thus, the final study cohort included 203,031 infants.
Independent variables
The main exposure of interest was insurance status of the newborn, categorized as private (commercial), Medicaid, or uninsured as documented (“primary payer”) on the hospital discharge record. Newborns were classified into four well-recognized categories based on recorded birth weights in the New York SID: normal (2500 grams or higher), low birth weight (1500 – 2499 grams), very low birth weight (1000 – 1499 grams), and extremely low birth weight (<1000 grams).14 We also included the following subject-level determinants in our model of rehospitalization: race, sex, median household income in patient’s zip code of residence, birth by Cesarean section, and initial length of stay. The SID database contains six race categories: White, Black, Hispanic, Asian/Pacific Islander, other, and unknown. We collapsed Asian/Pacific Islander and Other into one category. Median household income is an HCUP-generated variable based on census data that ranks median income in each zip code into four quartiles, which we collapsed into two categories: above and below the median. Cesarean section was defined by ICD-9-CM codes V30 – V39 that have a fifth digit of 1. Length of stay during birth hospitalization was defined as the period in days from the birth admission date to the discharge date.
Primary Outcome
Rehospitalization, the primary outcome measure, was defined as a hospital admission at least one day apart from the initial birth discharge. Hospital admissions that occurred on the same day as the birth stay discharge were considered transfers and not counted as rehospitalizations. The follow-up period for these patients (N=2,030) began after discharge from the “transferred to” hospital.15 Rehospitalizations during the first year after birth discharge were identified and assessed at three sub-intervals – within 30 days, 31 – 90 days, or 91 – 365 days of birth discharge – based on precedents in the general readmission literature.16,17
We evaluated the economic impact of rehospitalizations in terms of total costs. Costs were estimated from total charges using a cost-to-charge ratio supplied by HCUP.18 To assess the most common causes of rehospitalization, we used the primary ICD-9-CM diagnosis code documented for each rehospitalization.
Analyses
We first examined the distribution of data and calculated the baseline descriptive statistics for all variables included in the analyses. Negative binomial regression using a generalized estimating equations (GEE) approach was used to model rehospitalization and produce relative risks and 95% confidence intervals.20,21 The GEE approach accounts for correlation between subjects treated in the same hospital and produces population-averaged relative risk estimates.22 We performed stratified analysis by birth weight and birth length of stay to check for potential confounding. We also tested for two-way interaction between all combinations of variables and tested for multicollinearity. We tested differences in mean costs of rehospitalization across payer type and birth weight using generalized linear models with a log link and gamma distribution, adjusting for the same covariates as in our rehospitalization model. As inferences drawn from cost models are sometimes sensitive to distribution type, we performed a sensitivity analysis using a normal distribution.23,24 All statistical analysis was conducted using SAS/STAT software, Version 9.2 of the SAS system for UNIX (SAS Institute Inc., Cary, NC, USA). This project was approved by the Case Western Reserve University Institutional Review Board.
RESULTS
The study population included 203,031 live births, of which 51% had private insurance, 41% were on Medicaid and 9% were uninsured. Overall, 92.3% were normal birth weight, 6.4% were LBW, 0.8% were VLBW, and 0.5% were ELBW (Table 1). The distribution across payer types was relatively similar although overall low birth weight (<2500 g) was more common in newborns covered by Medicaid than those with private insurance (8.7% vs. 6.4%, p<.001). The racial/ethnic distribution was 50% White, 16% Black, and 14% Hispanic, with the remaining 18% classified as “other”. White newborns were most likely to be covered by private insurance, while the majority of Black and Hispanic newborns were covered by Medicaid. Low birth weight (all categories) was more common in Blacks than in Whites or Hispanics (11.8%, 6.5%, 7.5% respectively; p<.001).
Table 1. Baseline Characteristics of Newborns in the Study Population by Insurance Status.
| N (% of total) | Total | Private Insurance |
Medicaid Insurance |
Uninsured | p-value |
|---|---|---|---|---|---|
| No. of Newborns | N=203,031 | N=102,539 | N=82,590 | N=17,902 | |
| Birth Weight Size | p<.001 | ||||
| Normal (>2500 g) | 187,773 (93) | 95,495 (93) | 75,599 (92) | 16,679 (93) | |
| LBW (1500 - 2499 g) | 12,860 (6) | 5,938 (6) | 5,795 (7) | 1,127 (6) | |
| VLBW (1000 - 1499 g) | 1,526 (1) | 716 (1) | 729 (1) | 81 (0) | |
| ELBW (<1000 g) | 872 (0) | 390 (0) | 467 (1) | 15 (0) | |
| Race | p<.001 | ||||
| White | 101,242 (50) | 69,998 (68) | 27,073 (33) | 4,171 (23) | |
| Black | 32,019 (16) | 8,710 (8) | 18,804 (23) | 4,505 (25) | |
| Hispanic | 28,209 (14) | 6,988 (7) | 18,460 (22) | 2,761 (15) | |
| Other | 36,904 (18) | 14,346 (14) | 16,357 (20) | 6,201 (35) | |
| Missing | 4,657 (2) | 2,497 (2) | 1,896 (2) | 264 (1) | |
| Sex | p<.001 | ||||
| Male | 102,876 (51) | 51,966 (51) | 41,777 (51) | 9,133 (51) | |
| Female | 100,155 (49) | 50,573 (49) | 40,813 (49) | 8,769 (49) | |
| Median Household income in zip code of residence |
p<.001 | ||||
| Below state median | 98,202 (48) | 38,168 (37) | 54,068 (65) | 5,966 (33) | |
| Above state median | 87,647 (43) | 63,325 (62) | 21,188 (26) | 3,134 (18) | |
| C-section | p<.001 | ||||
| Yes | 70,462 (35) | 39,771 (39) | 25,400 (31) | 5,291 (30) | |
| No | 132,569 (65) | 62,798 (61) | 57,190 (69) | 12,611 (70) |
Abbreviations – LBW: Low Birth Weight, VLBW: Very Low Birth Weight, ELBW – Extremely Low Birth Weight.
Race is missing for 4,665 (2.3%) subjects, and median income in zip code of residence is missing for 17,228 subjects. Insurance status and other characteristics are measured at baseline (birth).
Rehospitalizations occurred in 9,010 infants (4.4% of the cohort); of these rehospitalized infants, 81% had one rehospitalization, 13% had two rehospitalizations, and 6% had three or more hospitalizations – for a total of 11,820 rehospitalizations. The first 30 days after discharge from birth-hospitalization had the highest rate of readmissions. Overall, rehospitalizations accounted for 98,437 bed days and costs of $79.3 million.
A higher percentage of newborns with Medicaid coverage and the uninsured were rehospitalized at each time period compared to the privately insured (Table 2). The rehospitalization outcomes also showed a dose-response relationship between lower birth weight category and increased rehospitalization percentage. The percentage rehospitalized was lowest among Whites and highest among Hispanics at each time period. Percentages for Black infants were comparable to Whites within the first 30 days, but became increasingly higher at subsequent time points.
Table 2. Rehospitalizations of Newborns in First Year of Life.
| Rehospitalization within 30 days |
Rehospitalization 31 – 90 days |
Rehospitalization 91 – 365 days |
Rehospitalization within 365 days |
|||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| No. | % | No. | % | No. | % | No. | % | |
|
| ||||||||
| No. of newborns readmitted | 3,524 | 1.74 | 2,477 | 1.22 | 3,751 | 1.85 | 9,010 | 4.44 |
| Insurance Status* | ||||||||
| Private | 1,375 | 1.34 | 790 | 0.77 | 1,263 | 1.23 | 3,211 | 3.13 |
| Medicaid | 1,854 | 2.24 | 1,517 | 1.84 | 2,215 | 2.68 | 5,098 | 6.17 |
| Uninsured | 295 | 1.65 | 170 | 0.95 | 273 | 1.53 | 701 | 3.92 |
| Birth Weight Size* | ||||||||
| Normal (>2500 g) | 2,954 | 1.57 | 2,025 | 1.08 | 3,162 | 1.68 | 7,632 | 4.06 |
| LBW (1500 - 2499 g) | 391 | 3.04 | 308 | 2.40 | 365 | 2.84 | 941 | 7.32 |
| VLBW (1000 - 1499 g) | 83 | 5.44 | 78 | 5.13 | 118 | 7.76 | 223 | 14.61 |
| ELBW (<1000 g) | 96 | 11.01 | 66 | 7.58 | 106 | 12.20 | 214 | 24.54 |
| Race*† | ||||||||
| White | 1,616 | 1.60 | 1,001 | 0.99 | 1,474 | 1.46 | 3,809 | 3.76 |
| Black | 546 | 1.71 | 465 | 1.45 | 731 | 2.28 | 1,596 | 4.98 |
| Hispanic | 638 | 2.26 | 552 | 1.96 | 884 | 3.13 | 1,896 | 6.72 |
| Other | 676 | 1.83 | 417 | 1.13 | 570 | 1.54 | 1,536 | 4.16 |
| Sex* | ||||||||
| Male | 2,006 | 1.95 | 1,452 | 1.41 | 2,155 | 2.10 | 5,157 | 5.01 |
| Female | 1,518 | 1.52 | 1,025 | 1.02 | 1,596 | 1.59 | 3,853 | 3.85 |
| Median HH Income*† | ||||||||
| Under Median | 1,981 | 2.02 | 1,484 | 1.51 | 2,197 | 2.24 | 5,217 | 5.31 |
| Over Median | 1,242 | 1.42 | 830 | 0.95 | 1,336 | 1.52 | 3,156 | 3.60 |
| C-section* | ||||||||
| Yes | 1,112 | 1.58 | 1,040 | 1.48 | 1,456 | 2.07 | 3,260 | 4.63 |
| No | 2,412 | 1.82 | 1,437 | 1.08 | 2,295 | 1.73 | 5,750 | 4.34 |
Chi-square test of within group difference yielded a p-value <0.001 for all four outcomes, suggesting this variable is associated with the outcome.
Race is missing for 4,665 (2.3%) subjects, and median income in zip code of residence is missing for 17,228 subjects. These rates are unadjusted. All characteristics measured at baseline.
Factors that independently affected the risk of rehospitalization are shown in Table 3. Medicaid insurance (relative risk (RR): 1.75, 95%CI: 1.66 – 1.83) or being uninsured (RR: 1.18, 95% CI 1.03 – 1.35) was independently associated with significantly higher risk of rehospitalization at each time period compared to private insurance – controlling for race, income, and birth weight. Decreasing birth weight category and higher birth length of stay were both associated with increased risk of rehospitalization. Hispanic ethnicity was associated with higher adjusted risk of rehospitalization. Although unadjusted readmission rates were higher for Black compared to White infants (Table 2), Black race was associated with lower adjusted risk of readmission within 30 days, and had no effect in later periods (Table 3). Males had 1.30 (95%CI: 1.25 – 1.35) times higher adjusted risk or readmission in one year compared to females. Tests for interaction effects were not significant, and there was no evidence of multicollinearity between any of our model covariates. Stratified analysis by birth weight did not meaningfully change the relative risk of the insurance status variables, suggesting confounding between birth weight and payer status on readmission outcomes was not an issue.
Table 3. Adjusted Risk Factors of Rehospitalization.
| 30 day rehospitalization |
31- 90 day rehospitalization |
91 – 365 day rehospitalization |
Total (One Year) | |
|---|---|---|---|---|
| RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | |
|
| ||||
| Insurance Status | ||||
| Private | Ref | Ref | Ref | Ref |
| Medicaid | 1.51 (1.40, 1.64) | 2.12 (1.92, 2.33) | 1.88 (1.74, 2.04) | 1.75 (1.66, 1.83) |
| Uninsured | 1.15 (1.01, 1.31) | 1.18 (0.99, 1.40) | 1.18 (1.03, 1.35) | 1.17 (1.08, 1.28) |
| Birth Weight Size | ||||
| Normal (>2500 g) | Ref | Ref | Ref | Ref |
| LBW (1500 - 2499 g) | 1.73 (1.54, 1.95) | 1.51 (1.31, 1.74) | 1.11 (0.98, 1.26) | 1.44 (1.34, 1.56) |
| VLBW (1000 - 1499 g) | 2.25 (1.72, 2.93) | 1.55 (1.16, 2.07) | 1.36 (1.07, 1.72) | 1.77 (1.51, 2.08) |
| ELBW (<1000 g) | 3.68 (2.83, 4.78) | 1.64 (1.18, 2.27) | 1.50 (1.16, 1.95) | 2.28 (1.93, 2.70) |
| Race | ||||
| White | Ref | Ref | Ref | Ref |
| Black | 0.80 (0.72, 0.88) | 0.96 (0.86, 1.08) | 1.10 (1.00, 1.21) | 0.96 (0.90, 1.02) |
| Hispanic | 1.12 (1.02, 1.23) | 1.38 (1.24, 1.54) | 1.59 (1.46, 1.73) | 1.35 (1.28, 1.43) |
| Other | 0.97 (0.89, 1.07) | 0.93 (0.82, 1.04) | 0.89 (0.81, 0.98) | 0.93 (0.88, 0.99) |
| Male | 1.29 (1.21, 1.38) | 1.37 (1.26, 1.48) | 1.30 (1.22, 1.39) | 1.30 (1.25, 1.35) |
| C-section birth | 0.75 (0.69, 0.80) | 1.11 (1.01, 1.20) | 0.95 (0.88, 1.02) | 0.92 (0.88, 0.96) |
| Median HH income below median* |
1.20 (1.11, 1.29) | 1.16 (1.06, 1.27) | 1.07 (1.00, 1.15) | 1.15 (1.09, 1.20) |
| Initial Length of Stay† | 1.57 (1.35, 1.82) | 2.43 (2.04, 2.90) | 2.77 (2.39, 3.21) | 1.81 (1.65, 1.99) |
RR = risk ratios. Risk ratios were estimated from multivariable negative binomial regression models.
Median HH income refers to whether or not the zip code the patient resides in has a median household income above or below the statewide median.
Initial length of stay is length of stay at birth stay before discharge home and is log transformed in the model. Risk ratios in bold were significant at p < 0.001.
We show the leading causes of rehospitalization within 30 days (Table 4) and 31 – 365 days (Table 5) post birth stay discharge between those with private and Medicaid insurance. Jaundice was the leading cause of rehospitalization with 30 days among all insurance types. Jaundice, feeding problems, and dehydration combined were the primary cause for 37% of all readmissions within the first 30 days of life. Acute bronchiolitis was the leading cause of readmission beyond 30 days for both Medicaid-enrolled and the privately insured.
Table 4. Leading Causes of Rehospitalization by Insurance Status, within 30 days of Birth Discharge Date.
| Rank | Medicaid | Private |
|---|---|---|
| 1 | Jaundice (27.9%) | Jaundice (44.7%) |
| 2 | Bronchiolitis (5.4%) | Bronchiolitis (4.3%) |
| 3 | Temperature Regulating Disorder (3.4%) | Pyloric Stenosis (3.5%) |
| 4 | Pyloric Stenosis (3.1%) | Temperature Regulating Disorder (2.7%) |
| 5 | Esophageal Reflux (3.1%) | Septicemia (2.0%) |
Table shows the five leading primary causes of rehospitalization within 30 days after discharge from birth hospitalization between Medicaid and the privately insured. Percentages are of the total rehospitalizations among each payer (i.e. column percent). Causes were classified using AHRQ Clinical Classification Software for ICD-9-CM. Non-specific ICD-9-CM codes (e.g. 779.9: unspecified conditions in the perinatal period) were excluded from the ranking.
Table 5. Leading Causes of Rehospitalization by Insurance Status, 31 – 365 days after Birth Discharge Date.
| Rank | Medicaid | Private |
|---|---|---|
| 1 | Bronchiolitis (16.4%) | Bronchiolitis (13.1%) |
| 2 | Pneumonia (4.8%) | Pneumonia (3.3%) |
| 3 | Urinary Tract Infection (3.8%) | Dehydration (2.9%) |
| 4 | Other Upper Resp Infection (3. 1%) | Urinary Tract Infection (2.9%) |
| 5 | Viral Infection (3.0%) | Other Upper Resp Infection (2.6%) |
Table shows the ten leading primary causes of rehospitalization in the period between 31 days and 365 days after discharge from birth hospitalization between Medicaid and the privately insured. Percentages are of the total rehospitalizations among each payer (i.e. column percent). Causes were classified using AHRQ Clinical Classification Software for ICD-9-CM. Non-specific ICD-9-CM codes (e.g. 779.9: unspecified conditions in the perinatal period) were excluded from the ranking.
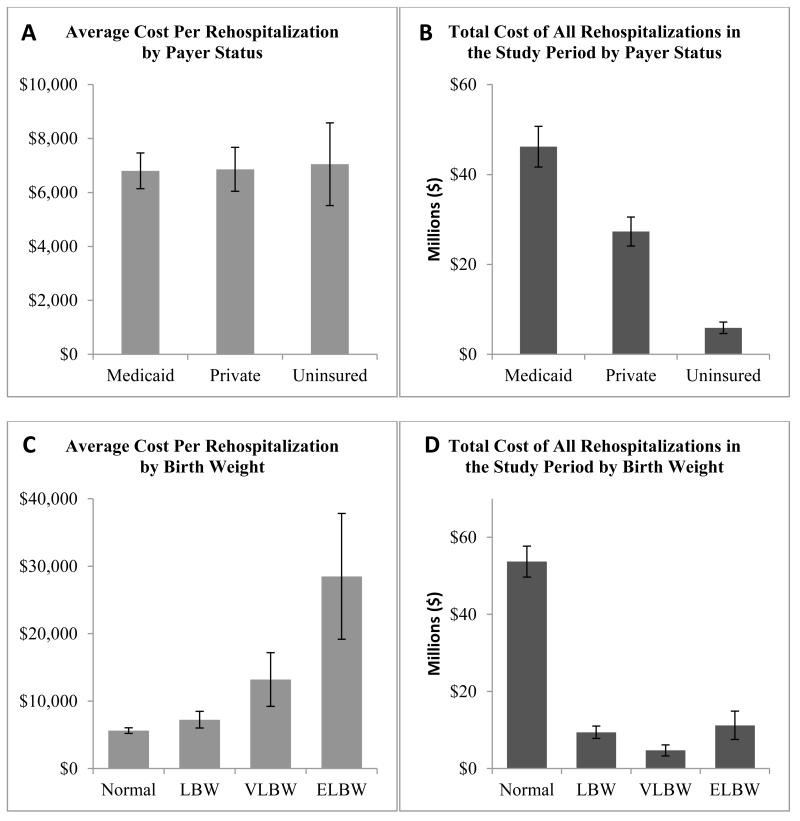
Figure 1 shows economic aspects of rehospitalization according to insurance status at birth and birth weight category. Costs per rehospitalization were similar across all payer types (p=0.10) (Figure 1, panel A); however, infants on Medicaid had the highest number of rehospitalizations and therefore total costs were higher for Medicaid than private insurers (Figure 1, panel B). Birth weight shows an inverse dose-response relationship with average cost per rehospitalization (p<0.001) (Figure 1, panel C). While normal birth weight infants had the lowest average cost per rehospitalization, they accounted for the highest total cost (Figure 1, panel D), primarily because they represented the majority of the population of newborns and the highest absolute number of rehospitalizations. Results were unchanged in sensitivity analysis.
Figure 1. Economic Burden of Rehospitalization by Insurance Status and Birth Weight.
DISCUSSION
Rehospitalization of infants in the first year after birth accounted for a high number of hospital days and substantial burden to the health care system in New York state. Rehospitalization rates were highest within the first 30 days of discharge. Medicaid covered a disproportionate share of low birth weight infants compared to private payers, and was associated with the highest rates of rehospitalization even after controlling for other factors. These results are consistent with previous studies, which found infants with Medicaid had higher odds of rehospitalization.4,7,31 Whereas, these previous studies were conducted only in high-risk newborn populations, our population-based study includes normal and low birth weight infants. Although the majority of infants were covered by private insurance, Medicaid bore almost twice as much of the economic burden of rehospitalizations as commercial insurers. This burden may grow as trends show the share of pediatric hospital care paid by Medicaid is increasing relative to private insurers.33
The reason that Medicaid-enrolled infants have higher odds of rehospitalization even after adjusting for other demographic factors is not clear. It could be due to socioeconomic factors that are associated with being covered by Medicaid, rather than the Medicaid program itself. These factors could include maternal age and education, paternal presence, and living situation. It has been shown that infants born to adolescent mothers, many of whom are on Medicaid, have increased rates of rehospitalization compared with infants born to older mothers.32 It is also possible that treating physicians may be more likely to hospitalize infants overnight if their parent is from a disadvantaged background. However, our results show similarities in the causes and average cost per readmission between Medicaid and private insurance which would seem to refute this possibility.
Previous population-based studies have shown that low birth weight infants utilize a disproportionate share of healthcare costs and services in their initial birth stay.25,26 Our population-based study showed that these costs continued after birth discharge. Low birth weight newborns had the higher rates of rehospitalization which is consistent with findings from previous studies.5,6,27–29 Rehospitalizations of low birth weight infants are generally longer and costlier than those for normal weight infants.30 However, our study showed the majority of rehospitalizations and greatest aggregate costs were in normal-weight infants. The risk of rehospitalization was highest among those on Medicaid among all birth weight categories.
We found that the impact of race as a correlate of rehospitalization was diminished after adjusting for other factors including birth weight, insurance status, and initial length of stay. Although race is often a correlate of poorer outcomes in many clinical areas, there are conflicting data regarding the impact of race on newborn’s readmissions. Some studies have shown that race is not a significant predictor of readmission among infants, while others have found Black race to be protective.6,7
We did not include urban/rural designation in our final model because less than 2% of our study population lived in a rural area as classified by the National Center Health Statistics. A recent population-based study found California infants living in rural counties had lower rehospitalization rates compared to urban counterparts.9 The impact of geography on variation in pediatric readmission is an area that deserves further study.
The primary cause of rehospitalizations in the first 30 days for both normal and low birth weight infants was hyperbilirubinemia, followed by infections and respiratory conditions. Some of these rehospitalization may be potentially avoidable with optimal postnatal care. One study classified jaundice, feeding problems, and dehydration as potentially avoidable within the first ten days of life.34 In our study, these three conditions accounted for 37% of all readmissions within the first 30 days of life. In later time intervals, the primary causes of rehospitalization were more likely to be infectious conditions, such as acute bronchiolitis, pneumonia, and UTI. These conditions may not be as dependent on postnatal care as conditions more associated with earlier admissions. Further research is needed to determine the preventability of these admissions, and to develop and evaluate potentially preventive interventions.
Much of the policy focus on reducing readmissions has been toward transitional care, which include patient education and programs designed to improve the continuity of care as patients leave the hospital.35,36 As it has been shown that areas with high hospital admission rates also have high readmission rates,37 and that there is considerable variation across hospitals in pediatric readmission,38 a complementary approach may be to focus on lowering hospital admissions overall in the pediatric and general population through shared saving incentives, for example, with accountable care organizations, bundled payments, and patient-centered medical homes. It is important to note that much of the research and policy papers regarding reducing readmissions are focused on either seniors or the general population, and suggested interventions may impact infant readmission differently. This study identifies that an important opportunity to reduce newborn infant rehospitalizations could involve improving strategies to reduce readmissions for hyperbilirubinemia. Infant-specific policies such as universal bilirubin screening may be such an intervention to reduce neonatal readmission.39
Caution to limitations of this study include that HCUP data are collected for billing rather than research and thus miscoding could have occurred, potentially biasing the results. We use the baseline measure of insurance status at birth throughout the entire study period, although for some newborns this will change over time. We could not treat insurance as a time-varying covariate as we would only have data on insurance changes among those that had a readmission. However, our data showed that 94% of those on Medicaid at readmission had Medicaid at birth, and 88% with private insurance at readmission had private insurance at birth, indicating insurance status may be relatively stable in the first year of life. The variables that we could adjust for were relatively limited. We did not have data on breastfeeding, which may have been a useful covariate given the high percentage of readmissions attributed to jaundice, dehydration, and feeding problems. Additional parental variables including age, education, and utilization of prenatal care would have been desirable. Complete and accurate information on gestational age would have also been desirable, but we could only estimate gestational age through ICD-9-CM codes. As the SID contained precise measures of birth weight in grams and length of stay we chose to use these variables instead. Birth weight and gestational age are likely to be highly correlated and including both would have probably led to multicollinearity in our models. As for any administrative database, generalizability requires caution.
Conclusion
Rehospitalization in the first year of life placed a substantial economic burden on the New York health care system. Medicaid bears a disproportionate share of low birth weight infants compared to private payers; infants with Medicaid had the highest rates of rehospitalization even after controlling for other factors. While normal birth weight infants had the lowest risk of readmission, our study shows they comprise the majority of the total economic burden and therefore policy interventions aimed at reducing costs should not focus solely on low birth weight infants. This study identifies the extent, predictors, and impact of infant rehospitalizations during the first year of life. Future research can explore the preventability of rehospitalizations, for example, by implementing novel strategies for discharge and postnatal care coordination especially for Medicaid-enrolled infants.
Acknowledgements
This study was supported by grants from the George Gund Foundation (PI: Dr. Cuttler) and the Rainbow Babies and Childrens Hospital Foundation. Dr. Schiltz was supported by the Agency for Healthcare Research and Quality (AHRQ) T32 Institutional Training Grant, #5T32HS000059-18 (PI: Alfred Rimm).
Footnotes
Disclosure: The authors certify that they have no conflicts of interest or financial relationships relevant to this research to disclose.
REFERENCES
- 1.McCannon J, Berwick DM. A new frontier in patient safety. JAMA. 2011;305(21):2221–2222. doi: 10.1001/jama.2011.742. doi:10.1001/jama.2011.742. [DOI] [PubMed] [Google Scholar]
- 2.Kocher RP, Adashi EY. Hospital readmissions and the Affordable Care Act: paying for coordinated quality care. JAMA. 2011;306(16):1794–1795. doi: 10.1001/jama.2011.1561. doi:10.1001/jama.2011.1561. [DOI] [PubMed] [Google Scholar]
- 3.Berry JG, Hall DE, Kuo DZ, et al. Hospital utilization and characteristics of patients experiencing recurrent readmissions within children’s hospitals. JAMA. 2011;305(7):682–690. doi: 10.1001/jama.2011.122. doi:10.1001/jama.2011.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCormick MC, Shapiro S, Starfield BH. Rehospitalization in the first year of life for high-risk survivors. Pediatrics. 1980;66(6):991–999. [PubMed] [Google Scholar]
- 5.Cuevas KD, Silver DR, Brooten D, Youngblut JM, Bobo CM. The cost of prematurity: hospital charges at birth and frequency of rehospitalizations and acute care visits over the first year of life: a comparison by gestational age and birth weight. Am J Nurs. 2005;105(7):56–64. doi: 10.1097/00000446-200507000-00031. quiz 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Escobar GJ, Greene JD, Hulac P, et al. Rehospitalisation after birth hospitalisation: patterns among infants of all gestations. Arch Dis Child. 2005;90(2):125–131. doi: 10.1136/adc.2003.039974. doi:10.1136/adc.2003.039974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morris BH, Gard CC, Kennedy K. Rehospitalization of extremely low birth weight (ELBW) infants: are there racial/ethnic disparities? J Perinatol. 2005;25(10):656–663. doi: 10.1038/sj.jp.7211361. doi:10.1038/sj.jp.7211361. [DOI] [PubMed] [Google Scholar]
- 8.Tommiska V, Tuominen R, Fellman V. Economic costs of care in extremely low birthweight infants during the first 2 years of life. Pediatr Crit Care Med. 2003;4(2):157–163. doi: 10.1097/01.PCC.0000059731.74435.02. doi:10.1097/01.PCC.0000059731.74435.02. [DOI] [PubMed] [Google Scholar]
- 9.Ray KN, Lorch SA. Hospitalization of rural and urban infants during the first year of life. Pediatrics. 2012;130(6):1084–1093. doi: 10.1542/peds.2012-0020. doi:10.1542/peds.2012-0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Young PC, Korgenski K, Buchi KF. Early readmission of newborns in a large health care system. Pediatrics. 2013;131(5):e1538–1544. doi: 10.1542/peds.2012-2634. doi:10.1542/peds.2012-2634. [DOI] [PubMed] [Google Scholar]
- 11.Wier LM, Barrett M, Steiner C, Jiang HJ. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Agency for Health Care Policy and Research (US); Rockville (MD): [Accessed August 2, 2013]. 2006. All-Cause Readmissions by Payer and Age, 2008: Statistical Brief #115. Available at: http://www.ncbi.nlm.nih.gov/books/NBK56036/ [Google Scholar]
- 12.Agency for Healthcare Research & Quality Introduction to the HCUP State Inpatient Database (SID) 2009. 2011 Available at: http://www.hcup-us.ahrq.gov/db/state/siddist/Introduction_to_SID.pdf.
- 13.Agency for Healthcare Research & Quality User Guide: HCUP Supplemental Variables for Revisit Analysis. 2012 Available at: http://www.hcup-us.ahrq.gov/toolssoftware/revisit/UserGuide_SuppRevisitFilesCD_03-10_050812.pdf.
- 14.Reichman NE. Low birth weight and school readiness. Future Child. 2005;15(1):91–116. doi: 10.1353/foc.2005.0008. [DOI] [PubMed] [Google Scholar]
- 15.Barrett M, Steiner C, Andrews R, Kassed C, Nagamine M. Methodological Issues when Studying Readmissions and Revisits Using Hospital Adminstrative Data. Agency for Healthcare Research & Quality; Rockville, MD: 2011. [Google Scholar]
- 16.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. doi:10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 17.Stone J, Hoffman G. Medicare Hospital Readmissions: Issues, Policy Options and PPACA. Congressional Research Service; Washington, D.C.: 2012. [Google Scholar]
- 18.Agency for Healthcare Research and Quality Cost-to-Charge Ratio Files: 2009 Central Distributor State Inpatient Database (CD-SID) User Guide. 2011 Available at: http://www.hcup-us.ahrq.gov/db/state/CCR2009CDUserGuide.pdf.
- 19.Elixhauser A, Steiner C, Palmer L. Clinical Classification Software (CCS), 2012. U.S. Agency for Healthcare Research & Quality; Available at: http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. [Google Scholar]
- 20.Wacholder S. Binomial regression in GLIM: estimating risk ratios and risk differences. Am J Epidemiol. 1986;123(1):174–184. doi: 10.1093/oxfordjournals.aje.a114212. [DOI] [PubMed] [Google Scholar]
- 21.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 22.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–130. [PubMed] [Google Scholar]
- 23.Nixon RM, Thompson SG. Parametric modelling of cost data in medical studies. Stat Med. 2004;23(8):1311–1331. doi: 10.1002/sim.1744. doi:10.1002/sim.1744. [DOI] [PubMed] [Google Scholar]
- 24.Thompson SG, Nixon RM. How sensitive are cost-effectiveness analyses to choice of parametric distributions? Med Decis Making. 2005;25(4):416–423. doi: 10.1177/0272989X05276862. doi:10.1177/0272989X05276862. [DOI] [PubMed] [Google Scholar]
- 25.Russell RB, Green NS, Steiner CA, et al. Cost of hospitalization for preterm and low birth weight infants in the United States. Pediatrics. 2007;120(1):e1–9. doi: 10.1542/peds.2006-2386. doi:10.1542/peds.2006-2386. [DOI] [PubMed] [Google Scholar]
- 26.Schmitt SK, Sneed L, Phibbs CS. Costs of newborn care in California: a population-based study. Pediatrics. 2006;117(1):154–160. doi: 10.1542/peds.2005-0484. doi:10.1542/peds.2005-0484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Underwood MA, Danielsen B, Gilbert WM. Cost, causes and rates of rehospitalization of preterm infants. J Perinatol. 2007;27(10):614–619. doi: 10.1038/sj.jp.7211801. doi:10.1038/sj.jp.7211801. [DOI] [PubMed] [Google Scholar]
- 28.Escobar GJ, Joffe S, Gardner MN, Armstrong MA, Folck BF, Carpenter DM. Rehospitalization in the first two weeks after discharge from the neonatal intensive care unit. Pediatrics. 1999;104(1):e2. doi: 10.1542/peds.104.1.e2. [DOI] [PubMed] [Google Scholar]
- 29.Lamarche-Vadel A, Blondel B, Truffer P, et al. Re-hospitalization in infants younger than 29 weeks’ gestation in the EPIPAGE cohort. Acta Paediatr. 2004;93(10):1340–1345. doi: 10.1080/08035250410032926. [DOI] [PubMed] [Google Scholar]
- 30.Petrou S, Mehta Z, Hockley C, Cook-Mozaffari P, Henderson J, Goldacre M. The impact of preterm birth on hospital inpatient admissions and costs during the first 5 years of life. Pediatrics. 2003;112(6 Pt 1):1290–1297. doi: 10.1542/peds.112.6.1290. [DOI] [PubMed] [Google Scholar]
- 31.Ambalavanan N, Carlo WA, McDonald SA, Yao Q, Das A, Higgins RD. Identification of extremely premature infants at high risk of rehospitalization. Pediatrics. 2011;128(5):e1216–1225. doi: 10.1542/peds.2011-1142. doi:10.1542/peds.2011-1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ray KN, Escobar GJ, Lorch SA. Premature infants born to adolescent mothers: health care utilization after initial discharge. Acad Pediatr. 2010;10(5):302–308. doi: 10.1016/j.acap.2010.07.005. doi:10.1016/j.acap.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 33.Friedman B, Berdahl T, Simpson LA, et al. Annual report on health care for children and youth in the United States: focus on trends in hospital use and quality. Acad Pediatr. 2011;11(4):263–279. doi: 10.1016/j.acap.2011.04.002. doi:10.1016/j.acap.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 34.Paul IM, Lehman EB, Hollenbeak CS, Maisels MJ. Preventable newborn readmissions since passage of the Newborns’ and Mothers’ Health Protection Act. Pediatrics. 2006;118(6):2349–2358. doi: 10.1542/peds.2006-2043. doi:10.1542/peds.2006-2043. [DOI] [PubMed] [Google Scholar]
- 35.Vohr BR, Yatchmink YE, Burke RT, et al. Factors associated with rehospitalizations of very low birthweight infants: Impact of a transition home support and education program. Early Hum Dev. 2011 doi: 10.1016/j.earlhumdev.2011.10.011. doi:10.1016/j.earlhumdev.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 36.Escobar GJ, McCormick MC, Zupancic JAF, et al. Unstudied infants: outcomes of moderately premature infants in the neonatal intensive care unit. Arch Dis Child Fetal Neonatal Ed. 2006;91(4):F238–244. doi: 10.1136/adc.2005.087031. doi:10.1136/adc.2005.087031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Epstein AM, Jha AK, Orav EJ. The relationship between hospital admission rates and rehospitalizations. N Engl J Med. 2011;365(24):2287–2295. doi: 10.1056/NEJMsa1101942. doi:10.1056/NEJMsa1101942. [DOI] [PubMed] [Google Scholar]
- 38.Berry JG, Toomey SL, Zaslavsky AM, et al. Pediatric readmission prevalence and variability across hospitals. JAMA. 2013;309(4):372–380. doi: 10.1001/jama.2012.188351. doi:10.1001/jama.2012.188351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alkalay AL, Bresee CJ, Simmons CF. Decreased neonatal jaundice readmission rate after implementing hyperbilirubinemia guidelines and universal screening for bilirubin. Clin Pediatr (Phila) 2010;49(9):830–833. doi: 10.1177/0009922810363728. doi:10.1177/0009922810363728. [DOI] [PubMed] [Google Scholar]