Abstract
Existing evidence suggests that communication failures are common in the operating room, and that they lead to increased complications, including infections. Use of a surgical safety checklist may prevent communication failures and reduce complications. Initial data from the World Health Organization Surgical Safety Checklist (WHO SSC) demonstrated significant reductions in both morbidity and mortality with checklist implementation. A growing body of literature points out that while the physical act of “checking the box” may not necessarily prevent all adverse events, the checklist is a scaffold on which attitudes towards teamwork and communication can be encouraged and improved. Recent evidence reinforces the fact the compliance with the checklist is critical for the effects on patient safety to be realized.
Keywords: surgical checklist, surgical briefing, surgical safety, communication, compliance
1. The Surgical Safety Checklist
In 2009, the World Health Organization (WHO) published the Surgical Safety Checklist (SSC) as part of their Safe Surgery Saves Lives campaign. The checklist was adapted from the field of aviation, where checklist use is standard practice. In aviation, checklists were developed in response to a crash involving an experienced pilot operating a new airplane with features that were significantly different from previous models. Shortly after takeoff, the plane stalled and crashed. An investigation revealed that the pilot had forgotten to perform one of the steps necessary for takeoff. In response, the checklist was created to prevent future avoidable disasters.(1)
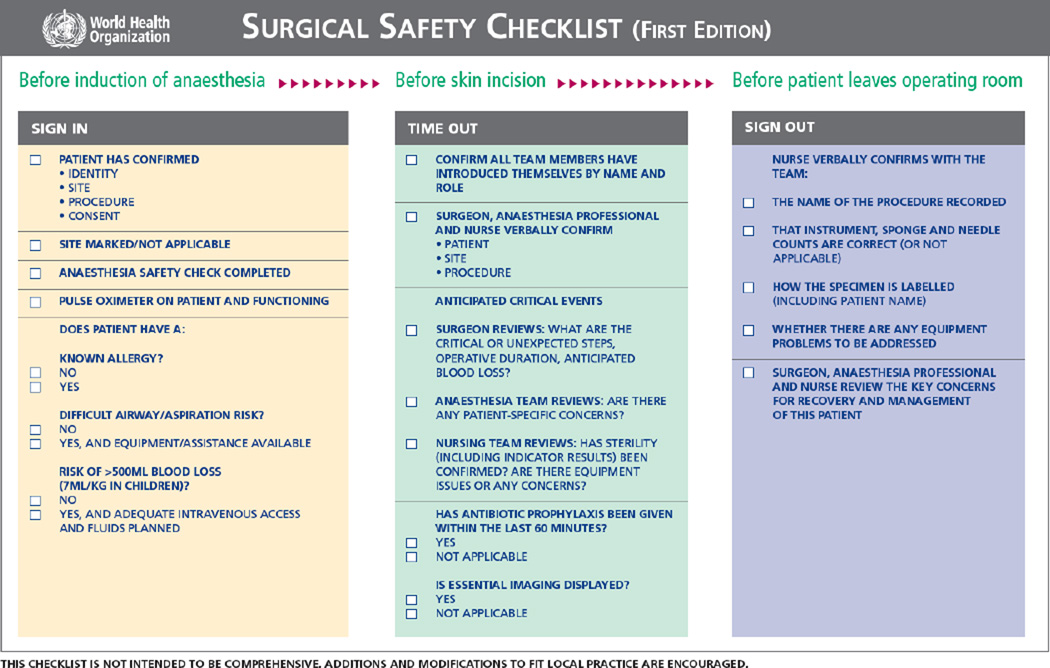
With more than 200 million operations performed annually, the WHO recognized the importance of addressing surgical safety when the checklist was introduced. The purpose of the checklist was to help operating room (OR) teams remember important details that may be missed during an operation. In addition, it served as a tool to encourage teamwork and communication.(2) In a sense, the WHO came to the same conclusion that the plane crash investigation team had: even highly skilled OR teams need tools to help them achieve optimal results. The initial WHO SSC was piloted at eight diverse hospitals around the world and contained 19 items that were to be addressed at defined time points during the operation (Figure 1).(3) The items included in the SSC are aimed at preventing uncommon but serious errors by reminding the team to confirm patient identity, surgical site, and other important characteristics such as comorbid conditions or anticipated complications. Results from the initial prospective, sequential, time-series observational study showed significant reductions in complications, in-hospital mortality, rates of unplanned reoperation, and surgical site infection (SSI) compared to pre-checklist rates. (4)
Figure 1.
Copy of World Health Organization Surgical Safety Checklist.
Since then, the WHO SSC has been implemented in more than 4,000 hospitals worldwide.(5) Hospitals are encouraged to customize the checklist to their needs, but the general format remains the same. Studies validating these various checklists have continued to show, for the most part, a benefit when the SSC or similar checklist is used, (6–11) but the mechanism by which this occurs is unclear. Recent high-profile reports have highlighted the pitfalls of SSCs, such as inconsistent implementation and compliance.(12) In an era of increasing complexity of care, it appears that the checklist is serving as a conduit for improved teamwork and communication through which the improved outcomes result.
The aim of this paper is to review the literature related to SSC use as a communication tool, with a focus on how the checklist is associated with team behaviors and attitudes in the OR. In addition, we describe scenarios where use of the SSC is associated with changes in patient outcomes. We reviewed studies that have been collated by the senior author, who has extensively studied the fields of OR safety, communication and checklist use for the past 10 years. We included studies that addressed the use of the checklist as a tool for improved communication in the OR, with an emphasis on changes in both team behaviors and clinical outcomes after implementation. Additional studies were selected that described compliance with the SSC and how it may be affected by variations in implementation strategy.
2. Communication Lapses are Common
Safety within the OR is an important public health concern. It is estimated that of the complications that occur within the hospital setting, more than half are associated with surgical procedures.(13) Every operation has a series of steps that must be performed correctly every time: surgeons must use the correct equipment, the equipment must be available and in proper working order, and drugs need to be administered in a timely and appropriate fashion. Errors can occur at any step with potential for threats to patient safety. As their roles in an operation are interdependent, it is incumbent on the anesthesia team, the nursing staff, and surgeons to communicate effectively to prevent avoidable complications such as wrong site surgery and inappropriate antibiotic administration.
Despite this, research has shown that surgeons, anesthesiologists, and nurses have rather different concepts of what constitutes teamwork and communication in the OR.(14, 15) One study used the Safety Attitudes Questionnaire (SAQ) to assess perception of patient safety in the OR. The SAQ is a standardized survey that uses a five-point Likert scale to measure items such as teamwork and safety.(16) This particular study found that women reported significantly lower aggregated scores than men on the domain “teamwork climate” (69 vs 76, p<0.05). (17) A separate study investigated specific aspects of teamwork and found that nurses reported significantly lower scores than surgeons regarding reception of nursing input (3.8 vs 4.3, p<0.001), ability to voice concern (3.5 vs 3.7, p=0.03), and whether physicians and nurses work well as a team (3.3 vs 3.7, p<0.001). (14) The consequences of this disparity can be serious. In one study investigating reports of wrong site surgery, OR personnel voiced concern in only 22% of cases (p<0.001). Of these times, surgeons responded to the concern 69% of the time. Pooled results predicted that in cases with the potential for wrong-site surgery, concerns would be raised and addressed only 41% of the time.(18)
While wrong site surgery is an uncommon event, communication failures are common, occurring every 7–8 minutes and affecting up to 30% of interactions in the OR.(19, 20) For a routine case lasting 2–3 hours, this means that up to 25 attempts at communication may be unsuccessful. Use of a checklist may prevent more than half of communication failures from occurring (21) by orienting the team to the individual patient, alerting each member to potential complications, and encouraging team members to voice concern when they notice an error occurring.
3. The Checklist can Improve Communication and Teamwork
One of the primary arguments in favor of checklists is that they help to decrease surgically associated morbidity and mortality, and can be implemented in most settings. Use of system-wide checklists can improve compliance with other metrics, such as increased timely antibiotic administration, decreased unexpected delays in the schedule, and reduced time spent outside of the OR gathering supplies during an operation.(21–23) Timely antibiotic administration has been linked to a decrease in surgical site infection. In one study, pre-incision antibiotics were not administered 12.1% of the time; after introduction of a checklist, this number decreased to 7.1% (p=0.015).(23) While introducing the checklist can initially be viewed as disruptive, staff members typically have a favorable attitude after it has been initiated.(24)
Substantial work has been undertaken to understand if the use of checklists actually improves communication in the OR. In a pilot study investigating the utility of pre-procedural briefing in cardiac surgery (similar to the WHO SSC), the number of miscommunication events declined by 50% in the briefing group compared to the group that did not use the briefing tool.(21) Other studies have found that communication failures declined by two thirds after initiation of a surgical briefing.(24) In a study investigating pre- and post-implementation scores using the SAQ, respondents were more likely agree that checklists are important for safety (4.58 vs 4.79, p=0.0058), and they were more likely to report a culture that encouraged team members to voice concern (4.02 vs 4.21, p=0.0225). Additionally, 93.4% of the clinicians who responded to the survey stated that if they were undergoing an operation, they would want the checklist used.(25)
Critics of the SSC have noted that while use of the checklist may identify problems, the person conducting the checklist is ultimately responsible for resolving the problem and redirecting the team.(26) For example, if the checklist demonstrates that the patient did not receive appropriate antibiotics in a timely fashion, the surgeon, anesthesiologist, and circulating nurse must rectify this mistake prior to proceeding with the operation. This begins to address an important concern: while the checklist itself might be improving patient safety, there may be something different about teams who routinely use the checklist. Checklists are rarely comprehensive enough to catch every possible error. Instead, proper use of the checklist may be a marker for teamwork and cooperation within the OR.
4. Is it the Checklist or the Teamwork?
Regardless of checklist use, the link between team behaviors and patient safety is well recognized. Infrequent use of team behaviors (defined in one study as “briefing,” “information sharing,” “inquiry,” “vigilance and awareness,” “assertion,” and “contingency management”) is associated with increased risk of death and other complications,(27) while high levels of communication and collaboration are associated with overall lower rates of risk-adjusted morbidity.(28) Other evidence shows a correlation between increased teamwork and a lower frequency of errors during an operation.(29) Wiegmann, in examining when errors in the OR are discovered and by whom, concluded that while poor teamwork can lead to errors, good teamwork leads to the detection and correction of mistakes.(30)
Investigators have attempted to describe the link between checklist use and improved patient outcomes. One explanation is that use of the checklist improves the safety culture within an institution by facilitating communication. Makary and colleagues administered an OR based version of the SAQ to assess changes after implementation of an OR briefing protocol. They found that introduction of an OR briefing improved collaboration amongst providers. Respondents reported increased scores on items such as awareness of surgical site brought about by the briefing (3.74 vs 3.18, p<0.001), coordinated efforts by surgical staff and anesthesia staff (4.54 vs 3.68, p<0.000), and on the importance of the briefing to patient safety (3.24 vs 2.75, p<0.001).(31)
However, checklist implementation may introduce new challenges that had not previously been considered. In a viewpoint discussing checklist use, Rydenfalt contends that merely introducing a checklist without monitoring compliance may actually make the OR less safe because previous safety checks are dropped.(32) OR staff have reported in interviews that use of the checklist can interrupt the performance of other safety tasks that are simultaneously being performed by individuals. Additionally, without a firm sense of commitment to the checklist it may become a routine activity of checking off boxes without actually driving behavior change or improvement. (33) Running through the list in such fashion may give OR staff a false sense of security that issues have truly been resolved when in fact they have not. (34) Without providing team members proper instruction regarding the use and value of the checklist, it may actually become a nuisance to the OR staff.
While there is a significant amount of data showing that checklist use leads to improvements in patient outcomes, investigators have also performed checklist audits to evaluate how the OR team uses the SSC in everyday practice. Levy and colleagues examined the efficacy of the checklist for ensuring performance in the OR and found that administrative records confirmed 100% performance while auditing by observers in the OR recorded less than 50% completion for most elements, and in some cases less than 10% of the checklist elements were completed.(35) Subsequently, the same group organized safety workshops as well as a stakeholder engagement group to customize the checklist for local concern. With these two interventions, overall adherence improved from 30% to 96% (p<0.001).(36)
5. Case Study
A recent report raised serious questions about the utility and effectiveness of surgical checklists. In 2010, the Canadian Province of Ontario mandated that each hospital use the WHO SSC and that they report their compliance. In this real-world observational study, hospitals were evaluated before and after implementation of the SSC. Information about compliance was abstracted from administrative records. Change in surgical mortality was the primary outcome, but the investigators also looked at other outcomes such as morbidity and readmission. The results of the study showed that despite widespread adoption of the WHO SSC, there was no significant difference in mortality (0.71% vs 0.65%, p=0.13) or surgical complications (3.86% vs 3.83%, p=0.29). (12)
It is unclear why the results of the Ontario study were so different from the original WHO study. The findings sparked a debate about what the surgical community should expect from the SSC, and whether its use was directly associated with a change in outcome. One of the criticisms of the Ontario study was related to implementation strategy, as it seemed that individual hospitals were responsible for implementation without being given administrative support. In the WHO SSC study, the task of implementation required considerable resources and support in order to be effective. Additionally, there was concern that compliance with the SSC was likely lower than what it had been in previous studies so the expected effects were not realized.(37) Despite operational flaws, many say that the findings from Ontario should be seriously considered, as the observational nature of this study is likely to be characteristic of typical use of the checklist.(38, 39) The results found in the rigorously controlled environment of a randomized controlled trial do not always approximate the effects that are seen in “real world” conditions, which may explain why there was no difference in morbidity or mortality rates in Ontario. Additionally, simply telling people to change their behavior without providing any guidance or support on how to do so may not be the most effective strategy.
6. Conclusion
The modern surgical environment is complex, and communication errors are relatively common. As described, used of the SSC has become common throughout the world. While checklists show promise in the reduction of surgical morbidity and mortality, there is also evidence that these improvements are not realized without careful attention to implementation strategy. When deciding to implement checklists in the OR, administrators should assess the climate of their hospital in order to make the checklist relevant to those who will be using it rather than an additional hurdle to jump over. Providing feedback to teams regarding patient outcomes and OR performance may be a valuable strategy to promote buy-in at the provider level.(33) In addition, encouraging customization of the checklist to fit the needs of the team may promote a feeling of ownership over the checklist, increasing compliance along the way. (33, 36) Without the support of staff members, it is unlikely that the checklist will lead to any changes in patient outcomes. For now, the surgical community should view the checklist as a tool for improving communication and safety culture, and be realistic about its direct impact on patient safety.
Acknowledgments
Research reported in this publication was supported by the National Institute of Diabetes And Digestive and Kidney Diseases of the National Institutes of Health under Award Number T32DK070555. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gawande A. The checklist manifesto: How to get things right. 1st ed. New York, NY: Metropolitan Books; 2010. [Google Scholar]
- 2.World Alliance for Patient Safety. WHO guidelines for safe surgery 2009: Safe surgery saves lives. Geneva: World Health Organization; 2009. [PubMed] [Google Scholar]
- 3.WHO surgical safety checklist and implementation manual [Internet] []. Available from: http://www.who.int/patientsafety/safesurgery/ss_checklist/en/ http://resolver.lib.washington.edu/resserv?sid=Refworks&charset=utf-8&__char_set=utf8&genre=article&aulast=World%20Alliance%20for%20Patient%20Safety&volume=2014&issue=09%2F29&atitle=WHO%20surgical%20safety%20checklist%20and%20implementation%20manual&au=World%20Alliance%20for%20Patient%20Safety%20&.
- 4.Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat AH, Dellinger EP, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009 Jan 29;360(5):491–499. doi: 10.1056/NEJMsa0810119. [DOI] [PubMed] [Google Scholar]
- 5.Surgical safety web map [Internet] 2012 []. Available from: http://maps.cga.harvard.edu:8080/Hospital/ http://resolver.lib.washington.edu/resserv?sid=Refworks&charset=utf-8&__char_set=utf8&genre=article&aulast=Center%20for%20Geographic%20Analysis%2C%20Harvard%20University&auinit=%20Harvard%20University&date=2012&volume=2014&issue=09%2F29&atitle=Surgical%20Safety%20Web%20Map&au=Center%20for%20Geographic%20Analysis%2C%20Harvard%20University%20&.
- 6.de Vries EN, Prins HA, Crolla RM, den Outer AJ, van Andel G, van Helden SH, et al. Effect of a comprehensive surgical safety system on patient outcomes. N Engl J Med. 2010 Nov 11;363(20):1928–1937. doi: 10.1056/NEJMsa0911535. [DOI] [PubMed] [Google Scholar]
- 7.Neily J, Mills PD, Young-Xu Y, Carney BT, West P, Berger DH, et al. Association between implementation of a medical team training program and surgical mortality. JAMA. 2010 Oct 20;304(15):1693–1700. doi: 10.1001/jama.2010.1506. [DOI] [PubMed] [Google Scholar]
- 8.van Klei WA, Hoff RG, van Aarnhem EE, Simmermacher RK, Regli LP, Kappen TH, et al. Effects of the introduction of the WHO "surgical safety checklist" on in-hospital mortality: A cohort study. Ann Surg. 2012 Jan;255(1):44–49. doi: 10.1097/SLA.0b013e31823779ae. [DOI] [PubMed] [Google Scholar]
- 9.Bliss LA, Ross-Richardson CB, Sanzari LJ, Shapiro DS, Lukianoff AE, Bernstein BA, et al. Thirty-day outcomes support implementation of a surgical safety checklist. J Am Coll Surg. 2012 Dec;215(6):766–776. doi: 10.1016/j.jamcollsurg.2012.07.015. [DOI] [PubMed] [Google Scholar]
- 10.Borchard A, Schwappach DL, Barbir A, Bezzola P. A systematic review of the effectiveness, compliance, and critical factors for implementation of safety checklists in surgery. Ann Surg. 2012 Dec;256(6):925–933. doi: 10.1097/SLA.0b013e3182682f27. [DOI] [PubMed] [Google Scholar]
- 11.Young-Xu Y, Neily J, Mills PD, Carney BT, West P, Berger DH, et al. Association between implementation of a medical team training program and surgical morbidity. Arch Surg. 2011 Dec;146(12):1368–1373. doi: 10.1001/archsurg.2011.762. [DOI] [PubMed] [Google Scholar]
- 12.Urbach DR, Govindarajan A, Saskin R, Wilton AS, Baxter NN. Introduction of surgical safety checklists in ontario, canada. N Engl J Med. 2014 Mar 13;370(11):1029–1038. doi: 10.1056/NEJMsa1308261. [DOI] [PubMed] [Google Scholar]
- 13.Gawande AA, Thomas EJ, Zinner MJ, Brennan TA. The incidence and nature of surgical adverse events in colorado and utah in 1992. Surgery. 1999 Jul;126(1):66–75. doi: 10.1067/msy.1999.98664. [DOI] [PubMed] [Google Scholar]
- 14.Carney BT, West P, Neily J, Mills PD, Bagian JP. Differences in nurse and surgeon perceptions of teamwork: Implications for use of a briefing checklist in the OR. AORN J. 2010 Jun;91(6):722–729. doi: 10.1016/j.aorn.2009.11.066. [DOI] [PubMed] [Google Scholar]
- 15.Mills P, Neily J, Dunn E. Teamwork and communication in surgical teams: Implications for patient safety. J Am Coll Surg. 2008 Jan;206(1):107–112. doi: 10.1016/j.jamcollsurg.2007.06.281. [DOI] [PubMed] [Google Scholar]
- 16.Sexton JB, Helmreich RL, Neilands TB, Rowan K, Vella K, Boyden J, et al. The safety attitudes questionnaire: Psychometric properties, benchmarking data, and emerging research. BMC Health Serv Res. 2006 Apr 3;6:44. doi: 10.1186/1472-6963-6-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carney BT, Mills PD, Bagian JP, Weeks WB. Sex differences in operating room care giver perceptions of patient safety: A pilot study from the veterans health administration medical team training program. Qual Saf Health Care. 2010 Apr;19(2):128–131. doi: 10.1136/qshc.2008.028233. [DOI] [PubMed] [Google Scholar]
- 18.Blanco M, Clarke JR, Martindell D. Wrong site surgery near misses and actual occurrences. AORN J. 2009 Aug;90(2) doi: 10.1016/j.aorn.2009.07.010. 215,8, 221-222. [DOI] [PubMed] [Google Scholar]
- 19.Hu YY, Arriaga AF, Peyre SE, Corso KA, Roth EM, Greenberg CC. Deconstructing intraoperative communication failures. J Surg Res. 2012 Sep;177(1):37–42. doi: 10.1016/j.jss.2012.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lingard L, Espin S, Whyte S, Regehr G, Baker GR, Reznick R, et al. Communication failures in the operating room: An observational classification of recurrent types and effects. Qual Saf Health Care. 2004 Oct;13(5):330–334. doi: 10.1136/qshc.2003.008425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Henrickson SE, Wadhera RK, Elbardissi AW, Wiegmann DA, Sundt TM., 3rd Development and pilot evaluation of a preoperative briefing protocol for cardiovascular surgery. J Am Coll Surg. 2009 Jun;208(6):1115–1123. doi: 10.1016/j.jamcollsurg.2009.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nundy S, Mukherjee A, Sexton JB, Pronovost PJ, Knight A, Rowen LC, et al. Impact of preoperative briefings on operating room delays: A preliminary report. Arch Surg. 2008 Nov;143(11):1068–1072. doi: 10.1001/archsurg.143.11.1068. [DOI] [PubMed] [Google Scholar]
- 23.de Vries EN, Dijkstra L, Smorenburg SM, Meijer RP, Boermeester MA. The SURgical PAtient safety system (SURPASS) checklist optimizes timing of antibiotic prophylaxis. Patient Saf Surg. 2010 Apr 13;4(1) doi: 10.1186/1754-9493-4-6. 6,9493-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lingard L, Regehr G, Orser B, Reznick R, Baker GR, Doran D, et al. Evaluation of a preoperative checklist and team briefing among surgeons, nurses, and anesthesiologists to reduce failures in communication. Arch Surg. 2008 Jan;143(1) doi: 10.1001/archsurg.2007.21. 12,7; discussion 18. [DOI] [PubMed] [Google Scholar]
- 25.Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat AH, Dellinger EP, et al. Changes in safety attitude and relationship to decreased postoperative morbidity and mortality following implementation of a checklist-based surgical safety intervention. BMJ Qual Saf. 2011 Jan;20(1):102–107. doi: 10.1136/bmjqs.2009.040022. [DOI] [PubMed] [Google Scholar]
- 26.Hu YY, Arriaga AF, Roth EM, Peyre SE, Corso KA, Swanson RS, et al. Protecting patients from an unsafe system: The etiology and recovery of intraoperative deviations in care. Ann Surg. 2012 Aug;256(2):203–210. doi: 10.1097/SLA.0b013e3182602564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mazzocco K, Petitti DB, Fong KT, Bonacum D, Brookey J, Graham S, et al. Surgical team behaviors and patient outcomes. Am J Surg. 2009 May;197(5):678–685. doi: 10.1016/j.amjsurg.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 28.Davenport DL, Henderson WG, Mosca CL, Khuri SF, Mentzer RM., Jr Risk-adjusted morbidity in teaching hospitals correlates with reported levels of communication and collaboration on surgical teams but not with scale measures of teamwork climate, safety climate, or working conditions. J Am Coll Surg. 2007 Dec;205(6):778–784. doi: 10.1016/j.jamcollsurg.2007.07.039. [DOI] [PubMed] [Google Scholar]
- 29.Catchpole K, Mishra A, Handa A, McCulloch P. Teamwork and error in the operating room: Analysis of skills and roles. Ann Surg. 2008 Apr;247(4):699–706. doi: 10.1097/SLA.0b013e3181642ec8. [DOI] [PubMed] [Google Scholar]
- 30.Wiegmann DA, ElBardissi AW, Dearani JA, Daly RC, Sundt TM., 3rd Disruptions in surgical flow and their relationship to surgical errors: An exploratory investigation. Surgery. 2007 Nov;142(5):658–665. doi: 10.1016/j.surg.2007.07.034. [DOI] [PubMed] [Google Scholar]
- 31.Makary MA, Mukherjee A, Sexton JB, Syin D, Goodrich E, Hartmann E, et al. Operating room briefings and wrong-site surgery. J Am Coll Surg. 2007 Feb;204(2):236–243. doi: 10.1016/j.jamcollsurg.2006.10.018. [DOI] [PubMed] [Google Scholar]
- 32.Rydenfalt C, Johansson G, Odenrick P, Akerman K, Larsson PA. Compliance with the WHO surgical safety checklist: Deviations and possible improvements. Int J Qual Health Care. 2013 Apr;25(2):182–187. doi: 10.1093/intqhc/mzt004. [DOI] [PubMed] [Google Scholar]
- 33.Russ SJ, Sevdalis N, Moorthy K, Mayer EK, Rout S, Caris J, et al. A qualitative evaluation of the barriers and facilitators toward implementation of the WHO surgical safety checklist across hospitals in England. Ann Surg. 2015 Jan;261(1):81–91. doi: 10.1097/SLA.0000000000000793. [DOI] [PubMed] [Google Scholar]
- 34.Whyte S, Lingard L, Espin S, Baker GR, Bohnen J, Orser BA, et al. Paradoxical effects of interprofessional briefings on OR team performance. Cogn Tech Work. 2008 Oct;10(4):287–294. [Google Scholar]
- 35.Levy SM, Senter CE, Hawkins RB, Zhao JY, Doody K, Kao LS, et al. Implementing a surgical checklist: More than checking a box. Surgery. 2012 Sep;152(3):331–336. doi: 10.1016/j.surg.2012.05.034. [DOI] [PubMed] [Google Scholar]
- 36.Putnam LR, Levy SM, Sajid M, Dubuisson DA, Rogers NB, Kao LS, et al. Multifaceted interventions improve adherence to the surgical checklist. Surgery. 2014 Aug;156(2):336–344. doi: 10.1016/j.surg.2014.03.032. [DOI] [PubMed] [Google Scholar]
- 37.Leape LL. The checklist conundrum. N Engl J Med. 2014 Mar 13;370(11):1063–1064. doi: 10.1056/NEJMe1315851. [DOI] [PubMed] [Google Scholar]
- 38.Avidan MS, Evers AS. Surgical safety checklists in Ontario, Canada. N Engl J Med. 2014 Jun 12;370(24):2350–2351. doi: 10.1056/NEJMc1404583. [DOI] [PubMed] [Google Scholar]
- 39.Albert RK. Surgical safety checklists in Ontario, Canada. N Engl J Med. 2014 Jun 12;370(24):2350. doi: 10.1056/NEJMc1404583. [DOI] [PubMed] [Google Scholar]