Abstract
Objective
To evaluate the efficacy of device-guided slow-paced respiration for reducing the frequency and severity of menopausal hot flushes.
Methods
Perimenopausal or postmenopausal women reporting four or more hot flushes per day were recruited into a parallel-group, randomized trial of slow-paced respiration using a portable guided-breathing device. Women were randomly assigned to use a standard device to practice slowing their resting breathing rate to less than 10 breaths per minute for at least 15 minutes every day or use an identical-appearing control device programmed to play relaxing non-rhythmic music while monitoring spontaneous breathing. The primary outcome, change in hot flush frequency over 12 weeks, was assessed using data from validated 7-day diaries abstracted by blinded analysts.
Results
Among the 123 participants, mean age was 53.4 (±3.4) years. Women reported an average of 8.5 (±3.5) hot flushes per day at baseline. After 12 weeks, women randomized to paced respiration (N=61) reported an average reduction of 1.8 (95%CI:0.9–2.6) hot flushes per day (−21%), compared to 3.0 (95%CI:2.1–3.8) hot flushes per day (−35%) in the music-listening group (N=62) (p=0.048). Paced respiration was associated with a 19% decrease in frequency of moderate-to-severe hot flushes, compared with a 44% decrease with music-listening (P=0.02).
Conclusions
In this randomized trial, women assigned to device-guided slow-paced respiration reported modest improvements in the frequency and severity of their hot flashes, but the paced respiration intervention was significantly less effective than a music-listening intervention in decreasing the frequency and severity of these symptoms..
Introduction
Over half of U.S. women experience hot flushes during the menopausal transition, and up to one third report symptoms 10 or more years after menopause [1, 2]. While estrogen therapy is effective in suppressing hot flushes, it is associated with an increased risk of endometrial cancer, and when combined with a progestin to prevent endometrial hyperplasia, it increases long-term risk of cardiovascular, cerebrovascular, and thromboembolic events [3, 4]. Other pharmacologic treatments such as antidepressants have modest effects on hot flushes, but also side effects that limit their acceptability [5–8]. As a result, there has been widespread interest in identifying non-pharmacologic treatments that are not only effective, but safe and well-tolerated [6, 7].
One non-pharmacologic treatment that has been widely recommended for hot flushes is slow-paced respiration, a behavioral relaxation technique that involves slowing the resting respiratory rate and prolonging expiration [9, 10]. In clinical studies, regular practice of slow-paced respiration has been shown to decrease sympathetic nervous system activity [11, 12] as well as improve management of chronic conditions such as hypertension associated with excess sympathetic tone [13–15]. Since abnormal adrenergic neurotransmission is also implicated in the etiology of hot flushes [16, 17], paced respiration has been recommended as a potentially effective hot flush treatment [9, 10], despite limited evidence from controlled trials [18–21].
We sought to estimate whether slow-paced respiration might provide an effective and generalizable treatment strategy for hot flushes, using a portable device that provides continuous guided-breathing support as well as objective, real-time feedback on adherence.
Materials and Methods
The Menopausal Treatment Using Relaxation Exercises (MaTURE) trial was a parallel group, partially-blinded, randomized trial of slow-paced respiration for treatment of hot flushes in perimenopausal and postmenopausal women. Participants were randomly allocated in equal proportions to use a commercially-available, portable guided-breathing device (ReSPERATE; Intercure, Ltd.) to practice slowing their respiratory rate to less than 10 breaths per minute for at least 15 minutes per day (paced respiration) for 12 weeks, or use an identical-appearing device programmed to play non-rhythmic music without guiding breathing (music-listening control). All participants provided informed consent prior to randomization, and all procedures were approved by the institutional review board of the University of California San Francisco (UCSF).
Participants were recruited from the general San Francisco Bay Area between January 2012 and December 2013 using community-based media efforts and recruitment fliers posted in clinic waiting rooms. Eligible participants were women aged 40 to 59 years who were perimenopausal or postmenopausal as defined by a history of bilateral oophorectomy, serum follicle-stimulating hormone levels of ≥30 mU per mL, or self-report of nine or fewer menstrual periods in the past year, and who documented an average of at least 4 hot flushes per 24 hours on a validated 7-day hot flush diary [22].
Women were excluded if they reported being pregnant or breastfeeding in the past year or using medications with known effects on hot flushes in the past 3 months. Other exclusion criteria included baseline respiratory rate <10 breaths per minute, chronic pulmonary disease, systolic blood pressure <100 mm Hg, or diastolic blood pressure <60 mm Hg. During a 7-day run-in period before randomization, candidates used a run-in device programmed to play relaxing music, and only those who used the device for ≥12 minutes per day on ≥6 days were eligible to continue.
Eligible women were randomized in equal ratios to one of the two intervention groups using a computer algorithm involving randomly permuted blocks of 2, 4, and 6. A programmer who had no direct contact with participants prepared a series of sequentially numbered, opaque envelopes containing randomization assignment, and study staff opened envelopes after confirming eligibility.
Participants randomized to paced respiration were instructed to use RESPeRATE, a portable, guided-breathing device, available without prescription, and approved by the U.S. Food and Drug Administration (FDA) for adjunctive treatment of hypertension. The device includes a belt-type respiration sensor that is placed around the chest over clothing, along with a small computerized box that generates musical tones transmitted through earphones. Using the sensor, the device first senses the user’s spontaneous respiratory rate and then begins to play musical tones synchronized to the user’s inspiration and expiration. The device then gradually lengthens the interval between the tones to guide the user in slowing respiration, while continuously monitoring the user’s breathing. For this study, devices were purchased by investigators and loaned to participants free of charge.
Participants randomized to the paced respiration group received brief in-person instruction (<15 minutes) from a research coordinator at the randomization visit. They were then asked to use the device to practice slow-paced respiration at home for a minimum of 15 minutes per day, consistent with recommended use for its FDA-approved indication of treatment of hypertension, for 12 weeks. Participants were encouraged to practice at approximately the same time each day to promote adherence. During practice sessions, participants were advised to sit quietly and avoid listening to other music, watching television, reading, sleeping, or other distracting activity.
A music-listening intervention was selected to control for participants’ time and attention in practicing paced respiration, as well as the general relaxing effect of sitting quietly during practice sessions. Participants assigned to music-listening were instructed to use a modified RESPeRATE device that was identical in appearance to the standard device, but did not actively guide their respiratory pattern; instead, the device was programmed to play a series of three non-rhythmic, relaxing melodies while monitoring the user’s spontaneous breathing rate. Music-listening participants received no instructions or encouragement to slow their respiratory rate. To minimize differential expectations of treatment success, participants were told that they were participating in a trial of two types of device-guided relaxation therapy, and that investigators did not know which intervention, if any, would prove to be effective in improving hot flushes.
Similar to participants in the paced respiration group, participants in the music-listening group received brief in-person instruction at the randomization visit and then used their devices for at least 15 minutes per day for 12 weeks. In both groups, women returned after 1 week to address any problems, and data from devices were downloaded at 1, 4, and 12 weeks to assess adherence to and quality of practice. Participants were also instructed to keep logs of the dates and times of practice.
The primary outcome of the trial was change in the average daily frequency of hot flushes over 12 weeks, measured using a 7-day diary validated and administered in multiple prior clinical trials of hot flushes [22]. Each participant was given a blank diary at the screening, 4-week, and 12-week visits and instructed to record each hot flush experienced over the next 7 days, as well as rate the severity of each hot flush as mild (scored as 1), moderate (2), or severe (3). Data were abstracted by an analyst who was blind to treatment assignment and had no contact with participants. Participants received $25 at baseline, $25 at 4 weeks, and $50 at 12 weeks upon return of completed diaries.
Secondary outcomes included change in the frequency of moderate-to-severe hot flushes and change in hot flush severity score, calculated by adding up the severity scores of all hot flushes documented in each 7-day diary period. Additional secondary outcomes included changes in other symptom and quality-of-life outcomes associated with hot flushes, measured by validated self-administered questionnaires measured over 12 weeks. Bothersomeness of hot flushes was assessed by the 10-item Hot Flash Related Daily Interference Scale (HFRDIS)[23]. Sleep disturbance was measured by the 7-item Insomnia Severity Index (ISI) [24]. Condition-specific quality of life was measured using the Menopause Quality of Life questionnaire (MENQOL), a 30-item questionnaire with vasomotor, physical, psychosocial, and sexual domains [25]. Depressive symptoms were measured using the 21-item Beck Depression Inventory-II (BDI-II) [26]. Cognitive anxiety (i.e., the mental component of anxiety associated with fear of future adverse events) was assessed using the 7-item anxiety subscale of the Hospital Anxiety and Depression Scale (HADS) [27], while somatic anxiety (i.e., believed to be related to autonomic physiological arousal response) was measured using the trait component of the 20-item Spielberger State Trait Anxiety Inventory (STAI) [28]. Perceived stress was assessed using the 10-item Cohen Perceived Stress Scale (PSS) [29]. All symptom and quality-of-life measures were administered at baseline, 4 weeks, and 12 weeks.
During practice sessions, both the standard and control devices automatically collected data on: a) the time and date they were used; b) duration of each practice session; c) average, minimum, and maximum respiratory rate; d) inspiratory to expiratory ratio; and e) data quality (i.e., percent time that breathing was detected by the sensor). Additionally, the standard devices monitored the amount of time the participant slowed respiration to <10 breaths per minute.
Safety was assessed by monitoring for adverse events at all follow-up telephone and in-person visits. A standardized question was used to prompt participants to report any negative changes in their health, which were recorded as adverse events on standardized forms.
Structured-item questionnaires were also used to assess demographic, clinical, and gynecologic history. Medication use was ascertained by direct review of medication bottles. Height, weight, blood pressure, and respiratory rate were measured.
Sample size was calculated under assumptions including: a) baseline frequency of hot flushes of ≥8 per day; b) mean reduction in frequency in the music-listening group of 2 hot flushes per day; c) standard deviation of the change of 4 hot flushes per day; and d) correlation between baseline and follow-up values of 0.5. A sample size of 120 (60 per group) was selected to provide approximately 85% power to detect a 25% difference between groups in change in frequency of any hot flushes in 2-sided tests with type-I error of 5%, allowing for loss-to-follow-up of 10%.
The primary analysis used linear mixed models with random intercepts and slopes to compare changes in daily hot flush frequency from baseline to 4 and 12 weeks, measured at each time point using the 7-day diary. We flexibly modeled the control group trajectory using a categorical variable for visit, then modeled the treatment effect using a time-by-treatment interaction, and adjusted for baseline value. For secondary outcomes, intervention effects were estimated using analysis of covariance models, adjusted for baseline scores. Approximate normality of the residuals was verified using density plots, and sensitivity to the slight departures we detected was ruled out using models with robust standard errors. Analyses were by intention to treat, according to treatment assignment, and without regard to adherence with use of the device. A sensitivity analysis was performed in which participants with missing outcomes data were excluded from models.
Results
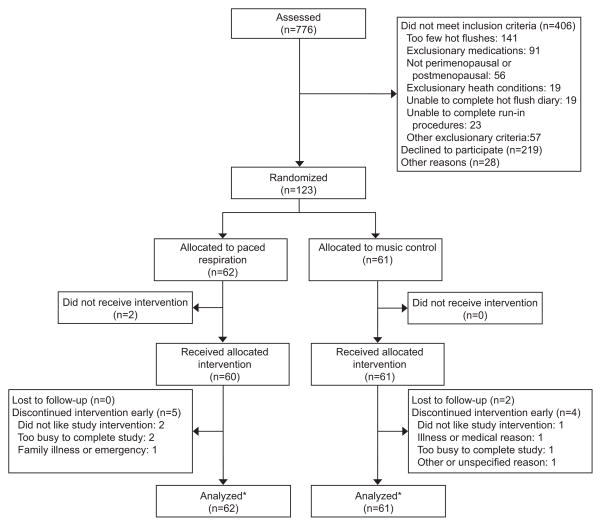
Of the 776 women assessed in any form, 123 were confirmed eligible and randomized, including 62 randomized to paced respiration and 61 to music-listening (Figure 1). Rates of early discontinuation and loss-to-follow-up did not differ between groups (P= 0.79).
Figure 1.
Recruitment, randomization, and retention in the Menopausal Treatment Using Relaxation Exercises trial. *Analysis included patients lost to follow-up and those who discontinued the intervention early.
Mean age was 53.4 (±3.4) years, and over 40% were racial or ethnic minorities (Table 1). Women reported an average of 8.5 (±3.5) hot flushes per day, including 5.4 (±3.5) moderate-to-severe hot flushes per day. Baseline characteristics did not differ significantly between groups.
Table 1.
Baseline Participant Characteristics, by Intervention Assignment
| Paced Respiration (N=62) | Music Listening (N=61) | P-value | |
|---|---|---|---|
| Demographic | |||
| Age (years) | 53.1 (±3.4) | 53.7 (± 3.4) | 0.27 |
| White or Caucasian | 38.0 (61.3%) | 34.0 (55.7%) | 0.53 |
| Black or African-American | 13.0 (21.0%) | 17.0 (27.9%) | 0.37 |
| Latina or Hispanic | 2.0 (3.2%) | 4.0 (6.6%) | 0.39 |
| Asian or Asian-American | 12.0 (19.4%) | 8.0 (13.1%) | 0.35 |
| Married or living as married | 42.0 (67.8) | 31.0 (50.8) | 0.06 |
| Gynecologic | |||
| Hysterectomy | 6.0 (9.7%) | 7.0 (11.5%) | 0.75 |
| Bilateral oophorectomy | 1.0 (1.6%) | 2.0 (3.3%) | 0.55 |
| Naturally postmenopausal* | 26.0 (48.1%) | 36.0 (62.1%) | 0.14 |
| ≥1 period in the past 12 months | 21.0 (38.9%) | 15.0 (25.9%) | 0.14 |
| Past use of estrogen therapy | 7.0 (11.3%) | 7.0 (11.5%) | 0.97 |
| Physical examination | |||
| Body mass index (kg per m2) | 26.6 (±4.7) | 26.4 (±6.2) | 0.86 |
| Systolic blood pressure (mmHg) | 122.3 (±19.7) | 120.0 (±16.1) | 0.48 |
| Diastolic blood pressure (mmHg) | 77.2 (±10.9) | 77.0 (±12.3) | 0.90 |
| Respiratory rate (breaths per minute) | 13.6 (±2.5) | 14.0 (±3.1) | 0.49 |
| Health-related habits | |||
| Current smoker | 4.0 (6.6%) | 8.0 (13.3%) | 0.21 |
| Alcohol ≥ 5 days per week | 8.0 (12.9) | 6.0 (9.8) | 0.59 |
| Hot flash frequency and severity* | |||
| Number of hot flushes per day | 8.6 (±3.7) | 8.4 (±3.3) | 0.88 |
| Moderate-to-severe hot flushes per day | 5.4 (±3.3) | 5.6 (±3.7) | 0.73 |
| Total hot flash severity scale score | 14.9 (±7.6) | 15.5 (±8.1) | 0.67 |
| Other symptoms and quality of life | |||
| Hot Flash Related Daily Interference Scale | 41.2 (±20.2) | 35.2 (±21.5) | 0.12 |
| The Menopause-Specific Quality of Life Questionnaire—Total | 4.2 (±1.2) | 3.8 (±1.3) | 0.10 |
| The Menopause-Specific Quality of Life Questionnaire-- Vasomotor Domain | 5.7 (±1.4) | 5.3 (±1.5) | 0.16 |
| Beck Depression Inventory II | 11.0 (±8.0) | 9.8 (±7.5) | 0.40 |
| Hospital Anxiety & Depression--Anxiety Subscale | 7.6 (±4.1) | 7.3 (±4.5) | 0.68 |
| Cohen Perceived Stress Scale | 16.8 (±6.6) | 16.3 (±8.3) | 0.72 |
| State-Trait Anxiety Inventory-- Trait Anxiety Subscale | 60.8 (±11.6) | 60.9 (±11.9) | 0.96 |
| Insomnia Severity Index | 12.1 (±6.4) | 11.7 ± (6.7) | 0.73 |
Data are number (percentage%) or as mean (± standard deviation) unless otherwise specified.
Defined as absence of menses for 12 months, without hysterectomy or bilateral oophorectomy
Hot flash frequency and severity scores were based on a 7-day symptom diary
After 12 weeks of follow-up, 91% (N=55) of women retained in the paced respiration group and 87% (N=52) retained in the music-listening group were confirmed to have completed at least 6 practice sessions per week (P=.98) (Table 2). In both groups, average practice time exceeded 15 minutes per day at 12 weeks (P=0.87).
Table 2.
Adherence to Practice of Assigned Intervention, by Intervention Assignment and Follow-up Time
| Paced Respiration (n=60) | Music Listening (n=61) | P-value | |
|---|---|---|---|
| Average minutes of practice per day— mean (±SD) | |||
| Week1 | 16.5 (±8.3) | 18.6 (±12.0) | 0.27 |
| Week4 | 15.9 (±5.5) | 17.1 (±10.9) | 0.45 |
| Week12 | 15.4 (±5.1) | 15.5 (±4.8) | 0.87 |
| Average days of practice per week— mean (±SD) | |||
| Week 1 | 6.38 (±0.9) | 6.41 (±1.1) | 0.32 |
| Week 4 | 6.06 (±1.3) | 6.36 (±0.6) | 0.36 |
| Week 12 | 6.37 (±0.6) | 6.28 (±0.7) | 0.64 |
Adherence to practice was assessed by review of data downloaded from RESPeRATE devices among participants who were confirmed to have received their assigned intervention. In the paced respiration group, adherence is reported for 58 women at week 1, 58 at week 4, and 55 at week 12. In the music-listening group, adherence is reported for 58 women at week 1, 57 at week 4, and 52 at week 12. For 7, 8, and 16 participants at the 1-week, 4-week, and 12-week visits, respectively, data could not be retrieved from devices due to computer malfunction or missing devices; assessment of adherence was therefore based on daily home practice diaries.
Within the paced respiration arm, mean respiratory rate during practice sessions decreased from 12.7 (±3.6) breaths per minute at baseline to 8.5 (±3.0) breaths per minute at 12 weeks. In contrast, average respiratory rate in the music-listening group was 13.3 (±3.8) breaths/minute at baseline and 13.6 (±4.4) breaths per minute at 12 weeks (P for between-group difference <0.001). Average expiratory breathing time increased in the paced respiration group from 3.2 (±1.2) seconds at baseline to 5.1 (±1.9) seconds at 12 weeks, whereas average expiratory time in the music-listening group was 3.0 (±1.1) seconds at baseline and 3.3 (±2.0) (P for between-group difference <0.001).
Participants randomized to paced respiration reported a 21% average decrease in frequency of any hot flushes after 12 weeks, compared to a decrease 35% decrease in the music-listening group (P=.048) (Table 3). Paced respiration was also associated with an average 19% decrease in frequency of moderate-to-severe hot flushes per day, compared to 44% decrease in frequency of moderate-to-severe hot flushes per day associated with music-listening (P=0.02). Total hot flush severity scores improved by an average of 3.0 points in the paced respiration versus 6.0 points in the music-listening group (P=.03). There was no evidence of an interaction between total amount of time of practice and treatment effects on frequency of hot flushes or total hot flush severity score (P for interaction >0.70 for all). Results from sensitivity analyses excluding participants without complete follow-up data did not differ substantially from the main models.
Table 3.
Changes in Average Hot Flash Frequency and Severity from Baseline to 12 Weeks, by Intervention Assignment
| Paced respiration (N = 62) | Music listening (N = 61) | Between-group difference in 12-week change | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 12-Week* | Change (95%CI) | Baseline | 12-Week* | Change (95%CI) | Diff. (95%CI) | P-value | |
| No. of hot flushes per day | 8.6 (±3.7) | 6.4 (±4.3) | −1.8 (−2.6 to − 0.9) | 8.4 (±3.3) | 5.1 (±3.2) | −3.0 (−3.8 to−2.1) | −1.2 (−2.4 to −0.0) | 0.048 |
| No. of moderate- to-severe hot flushes per day | 5.4 (±3.3) | 4.1 (±4.2) | −1.0 (−1.9 to − 0.2) | 5.6 (±3.7) | 2.6 (±2.4) | −2.4 (−3.2 to − 1.6) | −1.4 (−2.6 to −0.2) | 0.02 |
| Total hot flash severity score** | 14.9 (±7.6) | 11.2 (±9.8) | −3.0 (−4.9 to − 1.2) | 15.5 (±8.1) | 8.1 (±5.6) | −6.0 (−7.8 to − 4.1) | −2.9 (−5.4 to −.35) | 0.023 |
Data are mean (±SD), or as change (95%CI) unless otherwise specified. Linear mixed models with random intercepts and slopes were used to assess between-group changes in outcomes from baseline to 4 and 12 weeks.
12-week data are based on participants with 12 week hot flash diary data (46 and Paced respiration and 48 Music listening).
Total hot flash severity scores were calculated by adding the severity scores of all hot flushes reported over a 7-day period.
Over 12 weeks, paced respiration was associated with a 2.7 average decrease in ISI scores, compared to a decrease of 0.9 in the music-listening groups (P=.028) (Table 4). No significant differences in the intervention effects on other symptom or quality-of-life outcomes were detected.
Table 4.
Changes in Additional Symptom and Quality-of-Life Outcomes from Baseline to 12 Weeks, by Intervention Assignment
| Paced respiration (N = 62) | Music listening (N = 61) | Between-group difference in 12-week change | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 12-Week* | Change (95%CI) | Baseline | 12-Week* | Change (95%CI) | Diff. (95%CI) | P-value | |
| Hot Flash Daily Interference Scale | 41.2 (±20.2) | 26.5 (±21.9) | −13.6 (−18.7 to −8.5) | 35.2 (±21.5) | 20.0 (±17.7) | −15.1 (−20.0 to −10.1) | −1.5 (−8.6 to 5.7) | 0.69 |
| Menopause-Specific Quality of Life Questionnaire--Total | 4.2 (±1.2) | 3.2 (±1.1) | −0.9 (−1.1 to −0.7) | 3.8 (±1.3) | 3.0 (±1.1) | −0.8 (−1.0 to −0.6) | 0.1 (−0.2 to 0.5) | 0.49 |
| Menopause-Specific Quality of Life Questionnaire— Vasomotor Domain | 5.7 (±1.4) | 4.5 (±1.5) | −1.1 (−1.4 to −.7) | 5.3 (±1.5) | 4.3 (±1.9) | −1.0 (−1.4 to −0.7) | 0.0 (−0.5 to 0.6) | 0.92 |
| Beck Depression Inventory II | 11.0 (±8.0) | 7.7 (±8.8) | −3.1 (−4.1 to −2.0) | 9.8 (±7.5) | 6.5 (±6.0) | −2.6 (−3.6 to −1.5) | 0.5 (−1.0 to 2.0) | 0.52 |
| Hospital Anxiety & Depression--Anxiety Subscale | 7.6 (±4.1) | 6.8 (±4.5) | −.8 (−1.5 to −0.10) | 7.3 (±4.5) | 6.0 (±4.3) | −1.0 (−1.7 to −0.3) | −0.2 (−0.3 to 1.2) | 0.62 |
| Cohen Perceived Stress Scale | 16.8 (±6.6) | 14.5 (±7.4) | −2.0 (−3.2 to −0.7) | 16.3 (±8.3) | 14.1 (±7.0) | −1.4 (−3.0 to −0.2) | 0.6 (−1.1−2.3) | 0.51 |
| State-Trait Anxiety Inventory--Trait Anxiety | 39.2 (±11.6) 34.6 (±11.5) | −4.6 (−6.2 to −3.0) | 39.1 (±11.9) 35.6 (±11.8) | −2.5 (−4.1 to −0.9) | 2.1 (−0.2 to 4.3) | 0.07 | ||
| Insomnia Severity Index | 12.1 (±6.4) | 9.5 (±5.5) | −2.7 (−3.9 to −1.5) | 11.7 (±6.7) | 10.5 (±6.2) | −.9 (−2.0−0.3) | 1.9 (0.2 to 3.5) | 0.03 |
Data are mean (±SD) or change (95%CI) unless otherwise specified. Linear mixed models with random intercepts and slopes were used to assess between-group changes in outcomes from baseline to 4 and 12 weeks.
12-week data are based on those participants who completed 12-week measures (55 Paced respiration and 55 Music listening).
A total of 40 adverse events were reported in the paced respiration and 44 in the music listening group (P=.70). These included one woman who reported difficulty breathing and two who reported dizziness in the paced respiration group. No serious adverse events were reported.
Discussion
In this randomized trial, device-guided slow paced respiration was associated with a 21% decrease in the frequency of any hot flushes, compared to a 35% decrease in frequency associated with a music-listening intervention. These findings suggest that paced respiration may a less effective behavioral management strategy for menopausal hot flushes than listening to certain types of relaxation music, at least when taught using a portable guided-breathing device.
Our results provide intriguing new evidence that listening to relaxing music may be beneficial for women with hot flushes. Although the music-listening intervention was originally designed as a control for the paced respiration intervention, it was associated with an estimated 35% within-group decrease in any hot flush frequency and 44% decrease in moderate-to-severe hot flush frequency relative to baseline. This exceeds the magnitude of improvement associated with control interventions in trials of other treatments such as gabapentin, venlafaxine, and low-dose estrogen [30, 31]. Given that listening to relaxing music is easy, inexpensive, and associated with no known health risks, the moderate benefits of this strategy for reducing hot flushes may exceed the burdens. Nevertheless, the music-listening intervention used in this study featured a specific series of tonal non-rhythmic melodies, and findings may not be generalizable to other types of commercially-available music.
To date, several small trials have reported beneficial effects of paced respiration on hot flush frequency or severity [10, 18, 19]; however, those studies provided minimal between-group comparisons and also featured intensive expert- or laboratory-based training in paced respiration not available in the general community. In contrast, two recent trials in which women were taught to practice slow-paced respiration using a more generalizable audio-disc platform reported no significant benefits for hot flushes in comparison with either a rapid-breathing intervention or usual care controls, although adherence to home practice could not be objectively confirmed [20, 21].
One mechanism by which slow-paced respiration has been proposed to improve hot flushes is a reduction in excess sympathetic autonomic tone, which has been linked with hot flushes in observational research [13–15]. The potential beneficial effects of paced respiration may be mediated by other mechanisms, however, including an increased sense of relaxation, which may decrease the perceived burden of hot flushes. Of note, however, we did not detect significant differences in intervention effects on scores on anxiety or depression measures in this trial.
In contrast to its effects on hot flushes, the music-listening intervention was slightly less effective than paced respiration in improving insomnia symptoms as measured by ISI scores in our study. This was unexpected, given that hot flushes have the potential to wake women up from sleep, and hormonal treatments that are effective in reducing hot flushes are often effective in improving sleep quality [32]. In our study population, however, ISI scores were not strongly correlated with frequency of hot flushes, suggesting that hot flushes were not a major contributor to their insomnia.
This research benefits from involvement of an ethnically-diverse participant population, use of a rigorous time and attention control, high rates of retention and adherence, and objective confirmation of success in practicing paced respiration. Nevertheless, several limitations of this study should be noted. First, hot flushes were assessed by self-report diaries in the absence of any reliable objective method for monitoring these symptoms. Although diaries have been recommended by the FDA as an outcome measure in hot flush trials [33], they are subject to measurement error from inadequate recall of symptoms or backfilling of diaries. Second, while the vast majority of participants practiced their assigned interventions for the recommended minimum 15 minutes per day, only a minority practiced for more prolonged time periods or completed multiple practice session per day. Nevertheless, analyses did not detect any evidence that greater duration or frequency of practice was associated with more beneficial effects of paced respiration. Additionally, over a quarter of women who initially inquired about the study ultimately declined to enroll, which may decrease the generalizability of the findings.
Given the shortcomings of pharmacologic treatments for hot flushes, many women are interested in behavioral management strategies. Our results suggest that while women practicing paced respiration may perceive modest benefits for their hot flushes, paced respiration may be less effective in reducing the frequency and severity of hot flushes than listening to relaxing music, at least when taught using a portable guided-breathing device. Future research should be directed at confirming whether listening to relaxing music, as a potentially simple and inexpensive behavioral strategy, is in fact effective in alleviating hot flushes, as well as exploring mechanisms underlying treatment effects.
Acknowledgments
Funded by grant #5R01AT005491 from the National Center for Complementary and Alternative Medicine at the National Institutes of Health. Dr. Huang is further supported by a Paul B. Beeson Career Development Award in Aging Research from the National Institute on Aging (1K23AG038335). Ms. Jenny was supported by a Medical Student Training in Aging Research (MSTAR) award from the American Federation for Aging Research.
The RESPeRATE devices and data cables used in this study were purchased at the wholesale commercial price from Intercure, Ltd. Intercure Ltd. also provided the software used to download device data and re-program devices, but provided no other financial or material support for this research.
The MaTURE investigator team thanks Ann Chang, Lisa Abinanti, Traci Plaut, Caralisa Lascon, Anh Do, and Charlotte Palmer for their contributions to this research.
Footnotes
Presented at the Northern American Menopause Society Annual Meeting in National Harbor, Maryland, on October 16, 2014.
Clinical Trial Registration: Clinicaltrials.gov, www.clinicaltrials.gov, NCT01466998.
References
- 1.Freeman EW, Sammel MD, Sanders RJ. Risk of long-term hot flashes after natural menopause: evidence from the Penn Ovarian Aging Study cohort. Menopause. 2014 doi: 10.1097/GME.0000000000000196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang AJ, et al. Persistent hot flushes in older postmenopausal women. Archives of Internal Medicine. 2008;168(8):840–846. doi: 10.1001/archinte.168.8.840. [DOI] [PubMed] [Google Scholar]
- 3.Rossouw JE, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321–33. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- 4.Shumaker SA, et al. Estrogen plus progestin and the incidence of dementia and mild cognitive impairment in postmenopausal women: the Women’s Health Initiative Memory Study: a randomized controlled trial. JAMA. 2003;289:2651–62. doi: 10.1001/jama.289.20.2651. [DOI] [PubMed] [Google Scholar]
- 5.The 2012 hormone therapy position statement of: The North American Menopause Society. Menopause. 2012;19(3):257–71. doi: 10.1097/gme.0b013e31824b970a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nelson HD, et al. Nonhormonal therapies for menopausal hot flashes: systematic review and meta-analysis. JAMA. 2006;295(17):2057–71. doi: 10.1001/jama.295.17.2057. [DOI] [PubMed] [Google Scholar]
- 7.Rada G, et al. Non-hormonal interventions for hot flushes in women with a history of breast cancer. Cochrane Database Syst Rev. 2010;(9):CD004923. doi: 10.1002/14651858.CD004923.pub2. [DOI] [PubMed] [Google Scholar]
- 8.Freeman EW, et al. Efficacy of escitalopram for hot flashes in healthy menopausal women: a randomized controlled trial. Jama. 2011;305(3):267–74. doi: 10.1001/jama.2010.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Society, N.A.M. Menopause Practice: A Clinician’s Guide. 4. Mayfield Heights: North American Menopause Society; [Google Scholar]
- 10.Freedman RR. Hot flashes: behavioral treatments, mechanisms, and relation to sleep. Am J Med. 2005;118(Suppl 12B):124–30. doi: 10.1016/j.amjmed.2005.09.046. [DOI] [PubMed] [Google Scholar]
- 11.Clark ME, Hirschman R. Effects of paced respiration on anxiety reduction in a clinical population. Biofeedback Self Regul. 1990;15(3):273–84. doi: 10.1007/BF01011109. [DOI] [PubMed] [Google Scholar]
- 12.McCaul KD, Solomon S, Holmes DS. Effects of paced respiration and expectations on physiological and psychological responses to threat. J Pers Soc Psychol. 1979;37(4):564–71. doi: 10.1037//0022-3514.37.4.564. [DOI] [PubMed] [Google Scholar]
- 13.Narkiewicz K, et al. Sympathetic neural outflow and chemoreflex sensitivity are related to spontaneous breathing rate in normal men. Hypertension. 2006;47:51–5. doi: 10.1161/01.HYP.0000197613.47649.02. [DOI] [PubMed] [Google Scholar]
- 14.Raupach T, et al. Slow breathing reduces sympathoexcitation in COPD. Eur Respir J. 2008;2:387–92. doi: 10.1183/09031936.00109607. [DOI] [PubMed] [Google Scholar]
- 15.Joseph CN, et al. Slow breathing improves arterial baroreflex sensitivity and decreases blood pressure in essential hypertension. Hypertension. 2005;46:714–18. doi: 10.1161/01.HYP.0000179581.68566.7d. [DOI] [PubMed] [Google Scholar]
- 16.Freedman RR, Woodward S, Sabharwal SC. Alpha 2-adrenergic mechanism in menopausal hot flushes. Obstet Gynecol. 1990;76:573–8. [PubMed] [Google Scholar]
- 17.Freedman RR, Dinsay R. Clonidine raises the sweating threshold in symptomatic but not in asymptomatic postmenopausal women. Fertil Steril. 2000;74:20–3. doi: 10.1016/s0015-0282(00)00563-x. [DOI] [PubMed] [Google Scholar]
- 18.Freedman RR, Woodward S. Behavioral treatment of menopausal hot flushes: evaluation by ambulatory monitoring. Am J Obstet Gynecol. 1992;167(2):436–9. doi: 10.1016/s0002-9378(11)91425-2. [DOI] [PubMed] [Google Scholar]
- 19.Germaine LM, Freedman RR. Behavioral treatment of menopausal hot flashes: evaluation by objective methods. J Consult Clin Psychol. 1984;52(6):1072–9. doi: 10.1037//0022-006x.52.6.1072. [DOI] [PubMed] [Google Scholar]
- 20.Carpenter JS, et al. Paced respiration for vasomotor and other menopausal symptoms: a randomized, controlled trial. J Gen Intern Med. 2013;28(2):193–200. doi: 10.1007/s11606-012-2202-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sood R, et al. Paced breathing compared with usual breathing for hot flashes. Menopause. 2013;20(2):179–84. doi: 10.1097/gme.0b013e31826934b6. [DOI] [PubMed] [Google Scholar]
- 22.Sloan JA, et al. Methodologic lessons learned from hot flash studies. J Clin Oncol. 2001;19 (23):4280–90. doi: 10.1200/JCO.2001.19.23.4280. [DOI] [PubMed] [Google Scholar]
- 23.Carpenter JS. The Hot Flash Related Daily Interference Scale: a tool for assessing the impact of hot flashes on quality of life following breast cancer. Pain Symptom Management. 2001;22:979–89. doi: 10.1016/s0885-3924(01)00353-0. [DOI] [PubMed] [Google Scholar]
- 24.Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2000;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 25.Hilditch JR, et al. A menopause-specific quality of life questionnaire: development and psychometric properties. Maturitas. 1996;24:161–75. doi: 10.1016/s0378-5122(96)82006-8. [DOI] [PubMed] [Google Scholar]
- 26.Steer RA, Rissmiller DJ, Beck AT. Use of the Beck Depression Inventory-II with depressed geriatric inpatients. Behav Res Ther. 2000;38:311–8. doi: 10.1016/s0005-7967(99)00068-6. [DOI] [PubMed] [Google Scholar]
- 27.Herrmann C. International experiences with the Hospital Anxiety and Depression Scale--a review of validation data and clinical results. J Psychosom Res. 1997;42:17–41. doi: 10.1016/s0022-3999(96)00216-4. [DOI] [PubMed] [Google Scholar]
- 28.Barnes L, Harp D, Jung W. Reliability Generalization of Score son the Spielberger State-Trait Anxiety Inventory. Educational and Psychological Measurement. 2002;62(4):603–618. [Google Scholar]
- 29.Cohen S, Williamson G. Perceived stress in a probability sample of the United States. In: Sapacapam S, Oskamp S, editors. The social psychology of health: Claremont Symposium on applied psychology. Sage; Newbury Park, CA: 1988. [Google Scholar]
- 30.Butt DA, et al. Gabapentin for the treatment of menopausal hot flashes: a randomized controlled trial. Menopause. 2008;15(2):310–8. doi: 10.1097/gme.0b013e3180dca175. [DOI] [PubMed] [Google Scholar]
- 31.Joffe H, et al. Low-dose estradiol and the serotonin-norepinephrine reuptake inhibitor venlafaxine for vasomotor symptoms: a randomized clinical trial. JAMA Intern Med. 2014;174(7):1058–66. doi: 10.1001/jamainternmed.2014.1891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barnabei VM, et al. Menopausal symptoms in older women and the effects of treatment with hormone therapy. Obstet Gynecol. 2002;100(6):1209–18. doi: 10.1016/s0029-7844(02)02369-4. [DOI] [PubMed] [Google Scholar]
- 33.Food and Drug Administration. Guidance for Industry: Estrogen and Estrogen/Progestin Drug Products to Treat Vasomotor Symptoms and Vulvar and Vaginal Atrophy Symptoms. U.S. Department of Health and Human Services; Rockville: 2003. [Google Scholar]