Abstract
Background
Visits to emergency departments (EDs) for dental complaints are on the rise, yet reliance on EDs for dental care is far from ideal. ED toothache visits represent opportunities to improve access to professional dental care.
Methods
This research focuses on 20–29 year-olds, who account for more ED toothache visits than other age groups. We analyzed publicly available ED visits data from the National Hospital Ambulatory Medical Care Survey (NHAMCS). We assessed trends in ED toothache visit rates compared with back pain and all-cause ED visits during the past decade. We used 2009–2010 NHAMCS to characterize the more recent magnitude, relative frequency, and independent risk factors for ED toothache visits. Statistical analyses accounted for the complex sampling design.
Results
The average annual increase in ED visit rates among 20–29 year-olds during 2001–2010 was 6.1% for toothache; 0.3% for back pain; and 0.8% for all-causes ED visits. In 2009–2010, 20–29 year-olds made an estimated 1.27 million ED visits for toothaches and accounted for 42% of all ED toothache visits. Toothache was the fifth most common reason for any ED visit and third most common for uninsured ED visits in 20–29 year-olds. Independent risk factors for ED toothache visits were being uninsured or Medicaid-insured.
Conclusions
Younger adults increasingly rely on EDs for toothaches—likely because of barriers to accessing professional dental care. Expanding dental coverage and access to affordable dental care could increase options for timely dental care and decrease ED use for dental complaints.
Keywords: Access to care, emergency services, emergency treatment, toothache
The emergency department (ED) is a well-known safety net for those who face barriers to other sources of health care. However, reliance on the ED as a dental care safety net is problematic for many reasons. EDs usually are not staffed or equipped to deliver dental care. Most treatment rendered in the EDs for toothache is only temporizing,1–3 which means that the symptom is likely to recur in the absence of subsequent professional dental care.4 Moreover, because ED visits for dental complaints are disproportionately made by the uninsured,1–3,5–7 the cost of such care is more likely to be shifted to insured patients and absorbed by individual EDs and hospitals4 rather than more widely distributed among dental and public health care systems
ED toothache visits are usually classified as nonurgent, potentially contributing to ED inefficiency. Yet, advocates point out that the uninsured seek ED care for nonurgent problems not because they want to, but because they have no other option.8 If pain from toothache interferes with ability to sleep, eat, or work; and dental care is not affordable or accessible, then individuals will seek care where ever they can get it, including in the ED. There are few upfront financial barriers to ED care. Unlike dental offices, hospitals must legally provide emergency care to anyone who needs it, regardless of ability to pay.9 Additionally, tax exempt hospitals (and their EDs) are obligated by the IRS to provide charity care, often in the form of discounted care for low-income patients10,11; such financial assistance may not be as readily available in private dental practices.
In 2012, we reported that ED dental visits had increased between 2001 and 2008, particularly among adults.6 Other investigators have documented similar findings.12–15 As a next step in our research agenda, we then asked whether certain age groups were disproportionately represented among ED visits for dental complaints, specifically toothache, and found that 20–29 year-olds (“younger adults”) had substantially more ED visits for toothaches than other age groups. Understanding national trends in ED toothache visits and the magnitude and characteristics of more recent ED toothache visits, particularly in this high-utilizer age group, is important because these visits reflect opportunities to improve access and utilization of professional dental care through patient education, health policy, and expansion of dental public health infrastructure.
Methods
Research goals
We relied on the National Hospital Ambulatory Medical Care Survey (NHAMCS),16 a nationally-representative sample of US ED visits, to address 3 research goals as they pertain to 20–29 year-olds:
Compare average annual change in ED visit rates for toothache relative to back pain and all-cause ED visits during years 2001 through 2010. We chose back pain as a comparator because, like toothache, it is subjective and often perceived as a nonurgent reason for seeking ED care.17 We were interested in whether a rise in ED toothache visits was the result of secular increases in ED use overall or for nonurgent reasons. If so, we would expect similar changes in toothache ED visit rates as in all-cause ED and/or back pain visit rates during this period.
Rank the frequency of ED toothache visits relative to other common reasons for seeking ED care in 2009–2010.
Characterize patient-, hospital- and visit-level variables associated with ED toothache visits in 2009–2010. Based on review of the literature about racial, income, insurance and geographic-based disparities in dental care access and oral health,18–24 we hypothesized a priori that an ED toothache visit would be more likely on adjusted multivariable analysis: in non-whites than whites, when Medicaid or uninsured was listed as payer compared with private insurance, in EDs in non-MSA (i.e., rural and micropolitan statistical areas—relative to MSA (metropolitan statistical area),25 and during-business-hours compared with after-business-hours.
Data
NHAMCS is a national probability sample of hospital ED visits conducted annually by the US National Center for Health Statistics (NCHS).16 The multistaged sample design includes geographic primary sampling units, hospitals within primary sampling units; and patient visits within emergency service areas. Sampled EDs are located in general and short-stay hospitals—exclusive of federal, military, and Veterans Affairs hospitals—in the 50 US states and District of Columbia. Within an ED, visits are systematically selected during a randomly assigned 4-week reporting period. Hospital or US Census Bureau staff complete a patient record form for each sampled visit by reviewing the medical record. Sampled data are extrapolated to population estimates using assigned patient visit weights, which account for probability of visit selection, nonresponse, and ratio of sampled hospitals to all hospitals in the US.16
For the first research goal, we used 2001 through 2010 NHAMCS data and the corresponding year of US Census Bureau population estimate26 to calculate the rate of ED visits in the US population for each of the 10 years. We characterized recent ED toothache visits—the focus of the second and third research goals—using the 2 most recently released years of NHAMCS data (2009 and 2010), which we combined in order to improve reliability of our estimates—a strategy recommended by the NCHS.27 To ensure validity of our results, all reported estimates are based on at least 30 unweighted records and relative standard errors (RSE) less than 30%.
The University of Washington considers that research using certain publicly available datasets, including NHAMCS, does not involve “human subjects” as defined by federal regulations. Thus, no IRB approval was required (http://www.washington.edu/research/hsd/docs/1125).
ED visits
From NHAMCS, we selected ED visits made by 20–29 year-olds during 2001 through 2010. These were compared with ED toothache visits in other age groups in descriptive analysis.
Measures
Outcomes
The outcomes for this study were derived from the variable: “reason for the visit,” which is coded according to a NCHS classification system.28 The primary outcome variable was an ED visit for toothache (reason-for-visit code=1500.1) as chief complaint.28 We were interested in the chief complaint rather than discharge diagnoses because our focus is on toothache as a potentially preventable reason for an ED visit. In addition, investigators have noted that chief complaint of toothache is more reliably present in ED records than dental diagnoses, and that assigned dental diagnoses tend to be nonspecific.2,29 For comparison with ED toothache visit trends, we extracted ED visits for chief complaints of back pain (comprised of “back pain, ache, soreness, discomfort,” code=1905.1 and “low back pain, ache, soreness, discomfort,” code=1910.1). We generated the most frequent chief complaint for ED visits in younger adults in order to rank these relative to toothache in 2009–2010.
Covariates
For the third research goal, we extracted 3 categories of covariates from 2009–2010 NHAMCS: patient-related, hospital-related and visit-related. Patient-related covariates included: patient gender, race (White, Black, and other—as imputed or recoded by NHAMCS), and medical payer (private, Medicaid, uninsured, other/unknown). (NHAMCS identifies only medical payer and not dental benefit status. To aid in interpretation of results, we estimated the degree that medical insurance status reflected having dental coverage among US 20–29 year-olds, by analyzing 2009–2010 Medical Expenditure Panel Survey (MEPS) data (see Supplemental Materials for additional details). We found that being uninsured for medical care was almost always accompanied by lack of dental benefits (99.5% were insured for both medical and dental care). The converse however is not true: only 56% of 20–29 year-olds with private medical insurance for the entire calendar year had coverage for dental care during the year. Patients with private medical insurance making visits to the ED may or may not have dental benefits; thus, we could be underestimating the protective effect of having private dental coverage on ED toothache visits.) Among hospital variables, we included: US region where the ED was located (Northeast, South, Midwest and West), and MSA status of the ED (MSA and non-MSA). The visit-related variable was time/day of visit (during business hours—Monday through Friday 0800–1700 vs. nights/weekends).
Statistical analysis
We used the survey capabilities in Stata 12.0 to conduct all analyses. To describe and compare relative trends—our first research goal, we calculated population-based ED visit rates for toothache, back pain, and all-causes for each year 2001–2010, by dividing the annual weighted number of ED visits made by 20–29 year-olds for toothache, back pain, and all-causes in a given year by the estimated annual US Census Bureau’s population of 20–29 year-olds in the corresponding year (ED visits/1000 US population of 20–29 year-olds).26 We then assessed average percent annual change in the rates of population-based ED visits during 2001–2010 using weighted linear regression analysis for each of the 3 ED visit types.
For Research Goal 2, we determined the weighted proportion of each leading reason for the ED visit in 20–29 year-olds in 2009–2010. We ranked the top reasons-for-visit among all payers and then stratified by payer. For Research Goal 3, we generated weighted proportions and corresponding 95% confidence intervals (CIs) to describe variables related to patients, hospitals, and visits among 20–29 year-olds with and without a chief complaint of toothache. We conducted multivariable logistic regression to test hypotheses, and we generated weighted adjusted odds ratios and 95% CIs. Based on literature review, we specified a priori that the model would include gender, race, payer, hospital region, MSA status, and whether the ED visit occurred during business hours or not. We did not impute any values or take special measures for missing values because these were minimal among our selected covariates.
RESULTS
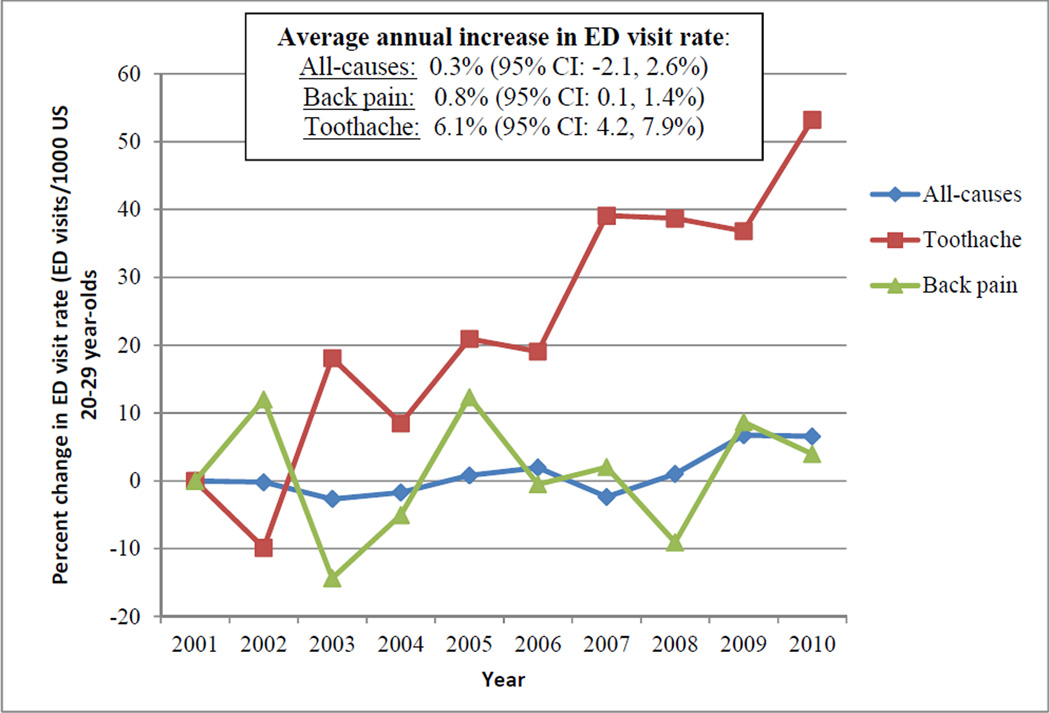
Relative to 2001, yearly population-based ED visit rates among 20–29 year-olds increased at a significantly higher rate for toothaches compared with back pain and all-causes (Figure 1): 6.1% (95% CI: 4.2, 7.9%) for toothache, 0.3% (95% CI: −2.1, 2.6%) for back pain, and 0.8% (95% CI: 0.1, 1.4%) for all-causes ED visits (census and weighted ED visit estimates for each year are tabulated in the Supplemental Materials). In 2009–2010, there were an estimated 3.02 million total visits made nationally to EDs for chief complaint of toothache (sample N=783), and 42% of these were made by 20–29 year-olds (sample N=317). In this age group, 2.8% of ED visits were for toothache—with lower odds for all other age categories (Figure 2). ED toothache visits by younger adults accounted for an estimated 1,271,000 visits nationally during 2009–2010 (95% CI: 1,039,000 & 1,504,000)—602,000 in 2009 and 669,000 visits in 2010. In 2009–2010, toothache was the fifth most common leading reason for an ED visit among all 20–29 year-olds. Toothache was ranked ninth for privately insured visits and fifth for Medicaid-insured visits, but, for uninsured ED visits, toothache was the third most common reason for an ED visit in this age group (Table 1).
Figure 1.
Percent change in rate of emergency department (ED) visit rates for toothache compared with all-causes and back pain among 20–29 year-olds from 2001 through 2010. NHAMCS, US. Between 2000 and 2010, ED toothache visits increased at a substantially higher rate than either all-cause or back pain ED visit among 20–29 year-olds.
Figure 2.
Weighted percentage of emergency department (ED) visits with toothache as leading reason-for-visit, by age category. Weighted odds ratio (OR) and 95% confidence interval (CI) of ED toothache visit by age category (20–29 year-olds are reference category). NHAMCS, US, 2009–2010. In 2009–2010, 20–29 year-olds had a statistically significantly higher odds of an ED toothache visit relative to other age groups.
Table 1.
Ranking of the Most Common Leading Reasons for ED Visits among 20–29 Year-olds: all ED visits and by payer. Weighted percentage and 95% confidence interval. NHAMCS, US, 2009–2010.
| ALL VISTS | PRIVATE INSURANCE (28.5%) |
UNINSURED (29.0%) |
MEDICAID (27.9%) |
||||
|---|---|---|---|---|---|---|---|
| 1. Abdominal Pain | 7.7% (7.0, 8.3) |
1. Abdominal pain |
7.9% (6.6, 9.1) |
1. Abdominal n |
6.8% (5.9, 7.8) |
1. Abdominal pain |
8.6% (7.2, 9.9) |
| 2. Back pain | 4.6 (4.2, 5.0) |
2. Back pain | 4.9 (4.1, 5.6) |
2. Back pain | 5.2 (4.3, 6.1) |
2. Back pain | 4.5 (3.3, 5.7) |
| 3. Headache | 3.6 (3.1, 4.1) |
3. Chest pain | 4.1 (3.0, 5.3) |
3. Toothache |
3.9 (3.1, 4.7) |
3. Headache | 3.7 (2.7, 4.6) |
| 4. Chest pain | 3.3 (2.8, 3.8) |
4. Headache | 3.1 (2.4, 3.9) |
4. Throat pain | 3.3 (2.3, 4.3) |
4. Chest pain | 3.6 (2.8, 4.3) |
| 5. Toothache |
2.8 (2.4, 3.2) |
5. Flank pain | 2.0 (1.4, 2.7) |
5. Headache | 3.2 (2.5, 3.9) |
5. Toothache |
3.1 (2.3, 3.9) |
| 6. Throat pain | 2.5 (2.1, 2.9) |
6. Fever… | 1.9 (1.3, 2.3) |
6. Chest Pain | 2.6 (1.9, 3.3) |
6. Throat pain | 2.3 (1.7, 3.0) |
| 9. Toothace |
1.4 (0.7, 2.1) |
||||||
In multivariable analysis, we found that being uninsured or being Medicaid-insured, relative to privately insured, was independently and positively associated with an ED visit for toothache compared with all other reasons for ED visits among 20–29 year-olds in 2009–2010 (Table 2)—confirming 1 out of 4 of our hypotheses. We did not find a statistically significant association with black race (N of sampled visits by non-white races was too small to include in the analysis), ED MSA status, or timing of visit on risk of ED toothache visit relative to another reason for an ED visit.
Table 2. Select Characteristics of ED Visits by 20–29 Year-olds for ED visits without and with toothache as leading complaint.
Weighted percentage, weighted adjusted odds ratio for toothache visit vs. another reason for ED visit, and 95% confidence intervals. NHAMCS, US, 2009–2010.
| ED VISITS FOR 20–29 YEAR-OLDS W/O TOOTHACHE |
ED VISITS FOR 20–29 YEAR-OLDS WITH TOOTHACHE |
WEIGHTED ADJUSTED ODDS RATIO |
|
|---|---|---|---|
|
PATIENT CHARACTERISTICS | |||
| GENDER | |||
| Female | 61.2% (95% CI 60.0, 62.4) | 59.6% (95% CI 52.4, 66.7) | 1.02 (95% CI 0.75, 1.38) vs. male |
| RACE | |||
| White | 71.1% (67.3, 74.8) | 74.0% (CI 67.8, 80.2) | Reference |
| Black | 25.0 (21.4, 28.7) | 24.2 (18.1, 30.2) | 0.89 (0.64, 1.24) |
| Other | 3.8 (2.7, 5.1) | N/A a | N/A a |
| PRIMARY PAYER | |||
| Private | 28.9% (27.1, 30.8) | 14.5% (8.5, 20.4) | Reference |
| Medicaid | 26.8 (24.9, 28.7) | 29.7 (22.5, 36.8) | 2.21 (1.30, 3.77) |
| Uninsured | 28.7 (26.4, 31.0) | 40.3 (33.8, 46.9) | 2.83 (1.73, 4.64) |
| Other/Unknown | 15.6 (13.6, 17.6) | 15.5 (9.9, 21.1) | 2.02 (1.04, 3.92) |
|
HOSPITAL CHARACTERISTICS | |||
| MSA STATUS OF ED | |||
| Non-MSA | 16.9% (7.8, 26.0) | 20.3% (8.6, 31.9) | 1.20 (0.82, 1.77) (vs. MSA) |
| US REGION OF ED | |||
| Northeast | 17.8% (15.1, 20.5) | 18.6% (12.3, 24.9) | Reference |
| Midwest | 22.8 (17.4, 28.2) | 24.7 (16.0, 33.4) | 0.98 (0.46, 1.60) |
| South | 41.4 (36.0, 46.8) | 39.9 (31.1, 48.7) | 0.90 (0.58, 1.39) |
| West | 17.1 (14.5, 21.3) | 16.7 (9.5, 23.8) | 1.00 (0.60, 1.66) |
|
VISIT CHARACTERISTICS | |||
| DAY/TIME OF VISIT | |||
| During business hours (0800–1700, Monday-Friday) | 37.2% (35.9, 38.6) | 35.7% (29.3, 42.2) | 0.96 (0.70, 1.31) vs. after business hours |
DISCUSSION
Among 20–29 year-olds, ED toothache visits rose, on average, 6.1% each year between 2001 and 2010, far outpacing yearly increases in back pain and all-cause ED visits. There are a number of possible explanations for why ED toothache rates grew to such a degree over 10 years, although the relatively stable rates of all-cause and ED back pain visits suggest that there are influences besides simple secular shifts that underlie this increase. It is likely that income- and employment-related factors, combined with economic stressors and decreasing public health resources for adult dental care in this decade, contributed to this trend. During the recent recession (December 2007–September 2010), higher unemployment rates meant fewer opportunities for employer-based dental benefits and less disposable income to pay for dental care.30 Under these influences, professional dental care visits made by adults declined substantially between 2001 and 2010, and to the greatest degree among poor adults.31 With more barriers to professional dental care, dental disease could advance unchecked until it manifests as a toothache or other complication. Toothache is similar to ambulatory care sensitive conditions32 (asthma is an example), in that lack of preventive care results in greater morbidity, cost, and societal burden.
Faced with budget shortfalls during the last decade, US states reduced public health funding for safety net dental clinics and eliminated or drastically reduced preventive and restorative dental benefits under adult Medicaid.33 Unlike the case for children, dental care is an optional state-level benefit for adults insured by Medicaid. Only 7 states maintained comprehensive dental benefits for adult Medicaid beneficiaries for all years between 2002 and 2010.34 There is precedent to support the association between decreased adult Medicaid dental funding and increased ED dental visits. In 1993, when the state of Maryland eliminated Medicaid reimbursement to dentists for treatment of adults with dental emergencies, the rate of dental visits to EDs by Medicaid recipients rose by 22%—an increase that occurred while ED visits by Medicaid recipients were otherwise decreasing.35 Similarly, after Massachusetts reduced Medicaid adult dental benefits in 2010, dental-related visits at a Boston safety net ED increased 14% by 2012.36
We also found that, in 2009–2010, the largest proportion of ED visits for toothache was made by 20–29 year-olds, accounting for 42% of such visits. Similar to our results, Jasek and coinvestigators reported that ED dental visits in New York during 2009–2011 were highest among 18–29 year-olds.29 Our research is the first to document that toothache is among the top reasons for younger adults to seek care in EDs. Specifically, toothache was the fifth most common chief complaint in EDs among 20–29 year-olds and the third most common for uninsured younger adults.
We posit a variety of reasons why younger adults disproportionately rely on the ED for toothache. Relative to adults 30 years and older, younger adults are poorer and less likely to have dental coverage. (In our analyses of 2009–2010 MEPS(see Supplemental Materials), 20–29 year-olds had the lowest proportion of all of the age categories with at least 1 dental visit (32.1%) and the second lowest proportion with dental benefits (33.7%) after 50+ year-olds. Second only to children, 18.3% of 20–29 year-olds were poor—defined as at/below 100% of the Federal Poverty Guideline or an annual income of less than or equal to $10,830 for a single adult in 2010 .) Our results indicate that, in this age group, being uninsured or Medicaid-insured were independent risk factors for ED toothache utilization, which supports the precept that financial barriers play a role in younger adults using the ED for toothache. Among 20–29 year-olds, being uninsured for medical care is essentially equivalent to being uninsured for dental care (see Supplemental Materials). Dental benefits under Medicaid are more variable, depending on state of residence. To qualify for adult Medicaid benefits during 2009–2010, the period for this study, typically required an income below the Federal Poverty Guideline and eligibility often was restricted to special groups, such as pregnant women or parents of dependent children.) Regardless of dental coverage, dental care can be costly. Nationally, 42% of dental expenses are paid out-of-pocket by consumers.33 Cost-sharing combined with a weak dental care safety net, in which demand outweighs supply,37 may pose insurmountable barriers to dental care for many young Americans,18, 19 regardless of the value they place on preventive dental care. Although EDs cannot turn away patients with emergency conditions (including pain and/or infection from toothache) for inability to pay,9 they are inadequately prepared to deliver dental care. On the other hand, dentists and other dental practitioners are uniquely able to provide preventive and restorative dental care needed to prevent toothache, but financial and other barriers may impede access. This is a conundrum deserving additional attention.
The ED toothache visit surge in the third decade of life may also result from missed opportunities for dental care during later adolescence. Only 30% of 16–18 year-old Medicaid enrollees received dental care in the previous year compared with 45% of children 6–11, and 38% 12–15 years old, according a 2008 US Government Accountability Office report.38 Untreated dental decay in later adolescence may become symptomatic—in the form of a toothache—a few years later, just at the point that younger adults have many fewer options for dental care because they have “aged out” of more generous pediatric dental coverage and resources. Dental care is a mandated benefit for low-income children on Medicaid under EPSDT39 (Early and Periodic Screening, Diagnosis, and Treatment legislation passed in 1967) and more recently, CHIPRA (the Children’s Health Insurance Program Reauthorization Act).40 However, in adulthood, dental care is an optional benefit under Medicaid, with most states substantially restricting eligibility criteria as well as limiting the scope of covered dental services.33
We did not find an association between time/day of the ED visit and the risk of an ED toothache visit. This implies that reasons behind ED toothache visits have less to do with finding a dentist who is open when a toothache occurs. ED MSA status and Black race were also not associated with higher risk of ED toothache visits in younger adults. Few studies have addressed ED MSA status as a predictor of ED dental visits. Okunseri and colleagues identified that Wisconsin Medicaid enrollees who lived in dental health professional shortage areas—a more specific variable than MSA—had a higher adjusted risk of an ED dental visit.41 With regards to race, prior studies have reported conflicting results about racial disparities in ED dental visits,2,6,13,41,42 but these studies did not generally focus on a specific age group and were often limited to smaller regions.
Certain limitations to this study bear mention. The quality of NHAMCS data may vary because it is abstracted on the hospital level.27,43 Some variables in NHAMCS contain missing values, were not recorded, or were imputed. However, the main conclusions drawn in this paper were based on variables with few or no missing values. Another limitation to NHAMCS is that data are collected at the visit level; and thus, we do not know if individual patients were represented more than once within a 4-week data collection period in an ED. Also inherent to secondary analysis is the limited number of available variables; this leaves some unanswered questions about ED visits for toothaches among young adults but generates hypotheses for future research.
Conclusions
Results of this research suggest the need to reconsider how a dental care delivery and payment model can better meet the oral health needs of adults, particularly in the 20- to 29-year-old range. Toothaches are among the top reasons for younger adults to seek care in EDs, which essentially forces integration of dental care into medical care, albeit in a less than optimal way. The time has come to view dental disease in the same way that we do other preventable medical problems—deserving of equitable funding, accessible care, and monitoring to ensure disparities are being addressed and are diminishing. To that end, ED toothache visits represents a potential quality indicator for system-level barriers to dental care access or utilization within a region or population.29
Finding solutions to the increasingly common nature of ED toothache visits will be complicated and require short and long term considerations. Redirecting ED patients with toothaches to a source of definitive dental care does not address the underlying missed opportunities for preventive and restorative dental care, but it is an essential step to alleviate ongoing reliance on EDs. Strengthening the dental care safety net is also imperative, and ideally, will be facilitated by expanded funding under the Affordable Care Act (ACA) for community health centers beginning in 2014.44 Borrowing from the medical insurance provisions under the ACA, maintaining dental coverage from childhood through younger adulthood, either from one’s parents or Medicaid, could provide a bridge to employment-based dental coverage. Likewise, encouraging regular preventive dental care and oral hygiene throughout adolescence may help maintain these practices and a relationship with a dental home into young adulthood as well.
Finally, although expansion of Medicaid under the ACA has increased the number of adults who are eligible for Medicaid, there remains no requirement that states cover dental care for adults enrolled in Medicaid. Furthermore, under the original ACA legislation, oral health care was designated an “essential health benefit” only for children.45 It is unclear why dental care would be considered essential during childhood but not adulthood. Dental disease, like other chronic diseases, has its substantive origins in childhood, but caries and periodontal disease continue to occur and advance during adulthood, ultimately affecting more than 90% of adults.46 Regular preventive dental care and timely restorative care are important throughout the lifespan, not just during the first 18 years.
Supplementary Material
Acknowledgments
Dr. McKinney and Ms. Rue were supported by grant 2KL2 TR000421-06 from the National Center for Advancing Translational Sciences, National Institutes of Health while participating in this research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure. None of the authors reported any disclosures.
Contributor Information
Charlotte W. Lewis, Department of Pediatrics, Division of General Pediatrics, School of Dentistry, University of Washington, Box 354920, Seattle, WA, 98195. cwlewis@u.washington.edu.
Christy M. McKinney, Department of Oral Health Sciences, School of Dentistry, University of Washington, Seattle, WA..
Helen H. Lee, Department of Pediatric Anesthesiology and Pain Medicine, Seattle Children’s Hospital. Seattle, WA.
Molly L. Melbye, Department of Oral Health Sciences, School of Dentistry, University of Washington, Seattle, WA; Neighborcare Health. Seattle, WA.
Tessa C. Rue, Department of Biostatistics, University of Washington, Seattle, WA..
References
- 1.Hocker MB, Villani JJ, Borawski JB, et al. Dental visits to a North Carolina emergency department: a painful problem. N C Med J. 2012;73(5):346–351. [PubMed] [Google Scholar]
- 2.Lewis C, Lynch H, Johnston B. Dental complaints in emergency departments: a national perspective. Ann Emerg Med. 2003;42(1):93–99. doi: 10.1067/mem.2003.234. [DOI] [PubMed] [Google Scholar]
- 3.McCormick AP, Abubaker AO, Laskin DM, Gonzales MS, Garland S. Reducing the burden of dental patients on the busy hospital emergency department. J Oral Maxillofac Surg. 2013;71(3):475–478. doi: 10.1016/j.joms.2012.08.023. [DOI] [PubMed] [Google Scholar]
- 4.Davis EE, Deinard AS, Maiga EW. Doctor, my tooth hurts: the costs of incomplete dental care in the emergency room. J Public Health Dent. 2010;70(3):205–210. doi: 10.1111/j.1752-7325.2010.00166.x. [DOI] [PubMed] [Google Scholar]
- 5.Allareddy V, Rampa S, Lee MK, Allareddy V, Nalliah RP. Hospital-based emergency department visits involving dental conditions: profile and predictors of poor outcomes and resource utilization. J Am Dent Assoc. 2014;145(4):331–337. doi: 10.14219/jada.2014.7. [DOI] [PubMed] [Google Scholar]
- 6.Lee HH, Lewis CW, Saltzman B, Starks H. Visiting the emergency department for dental problems: trends in utilization, 2001 to 2008. Am J Public Health. 2012;102(11):e77–e83. doi: 10.2105/AJPH.2012.300965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nalliah RP, Allareddy V, Elangovan S, Karimbux N, Allareddy V. Hospital based emergency department visits attributed to dental caries in the United States in 2006. J Evid Based Dent Pract. 2010;10(4):212–222. doi: 10.1016/j.jebdp.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 8.Gonzalez-Morganti K, Bauhoff S, Blanchard JC, et al. The Evolving Role of Emergency Departments in the United States. Santa Monica, CA: RAND Corporation; 2013. [PMC free article] [PubMed] [Google Scholar]
- 9.Emergency Medical Treatment & Labor Act (EMTALA) [Accessed November 28, 2014];Centers for Medicare and Medicaid Services. https://www.cms.gov/Regulations-and-Guidance/Legislation/EMTALA/index.html?redirect=/EMTALA.
- 10. [Accessed November 28, 2014];Instructions for Form 1023 (Rev June 2006). Application for Recognition of Exemption Under Section 501(c)(3) of the Internal Revenue Code. http://www.irs.gov/pub/irs-prior/i1023--2006.pdf.
- 11. [Accessed November 28, 2014];New Requirements for 501(c)(3) Hospitals Under the Affordable Care Act. Internal Revenue Service, United States Treasury. http://www.irs.gov/Charities-&-Non-Profits/Charitable-Organizations/New-Requirements-for-501(c)(3)-Hospitals-Under-the-Affordable-Care-Act.
- 12.Anderson L, Cherala S, Traore E, Martin NR. Utilization of Hospital Emergency Departments for non-traumatic dental care in New Hampshire, 2001–2008. J Community Health. 2011;36(4):513–516. doi: 10.1007/s10900-010-9335-5. [DOI] [PubMed] [Google Scholar]
- 13.Hong L, Ahmed A, McCunniff M, et al. Secular trends in hospital emergency department visits for dental care in Kansas City, Missouri, 2001–2006. Public Health Rep. 2011;126(2):210–219. doi: 10.1177/003335491112600212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pajewski NM, Okunseri C. Patterns of dental service utilization following nontraumatic dental condition visits to the emergency department in Wisconsin Medicaid. J Public Health Dent. 2014;74(1):34–41. doi: 10.1111/j.1752-7325.2012.00364.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wall T. Recent trends in dental emergency department visits in the United States, 1997/1998 to 2007/2008. J Public Health Dent. 2012;72(3):216–220. doi: 10.1111/j.1752-7325.2012.00339.x. [DOI] [PubMed] [Google Scholar]
- 16.National Hospital Ambulatory Medical Care Survey (NHAMCS) and National Ambulatory Medical Care Survey (NAMCS) [Accessed November 28, 2014];Centers for Disease Control and Prevention, National Center for Health Statistics. www.cdc.gov/nchs/ahcd.htm.
- 17.Friedman BW, Chilstrom M, Bijur PE, Gallagher EJ. Diagnostic testing and treatment of low back pain in United States emergency departments: a national perspective. Spine (Phila Pa 1976) 2010;35(24):E1406–E1411. doi: 10.1097/BRS.0b013e3181d952a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.(IOM) Institute of Medicine and (NRC) National Research Council. Improving Access to Oral Health Care for Vulnerable and Underserved Populations. Washington, DC: The National Academies Press; 2011. [Google Scholar]
- 19.Oral Health in America: A Report of the Surgeon General. National Institute of Dental and Craniofacial Research, National Institutes of Health. Rockville, MD: U.S. Department of Health and Human Services; 2000. [Google Scholar]
- 20.2012 National Healthcare Disparities Report: Chapter 7. Efficiency. Rockville, MD: Agency for Healthcare Research and Quality; [Accessed November 28, 2014]. Published May 2013. http://www.ahrq.gov/research/findings/nhqrdr/nhdr12/chap7.html. [Google Scholar]
- 21.Lewis C, Mouradian W, Slayton R, Williams A. Dental insurance and its impact on preventive dental care visits for U.S. children. J Am Dent Assoc. 2007;138(3):369–380. doi: 10.14219/jada.archive.2007.0170. [DOI] [PubMed] [Google Scholar]
- 22.Okunseri C, Bajorunaite R, Abena A, et al. Racial/ethnic disparities in the acceptance of Medicaid patients in dental practices. J Public Health Dent. 2008;68(3):149–153. doi: 10.1111/j.1752-7325.2007.00079.x. [DOI] [PubMed] [Google Scholar]
- 23.Skillman SM, Doescher MP, Mouradian WE, Brunson DK. The challenge to delivering oral health services in rural America. J Public Health Dent. 2010;70(Suppl 1):S49–S57. doi: 10.1111/j.1752-7325.2010.00178.x. [DOI] [PubMed] [Google Scholar]
- 24.Vargas CM, Dye BA, Hayes K. Oral health care utilization by US rural residents, National Health Interview Survey 1999. J Public Health Dent. 2003;63(3):150–157. doi: 10.1111/j.1752-7325.2003.tb03493.x. [DOI] [PubMed] [Google Scholar]
- 25. [Assessed November 28, 2014];Metropolitan and Micropolitan Statistical Areas. United States Census Bureau. http://www.census.gov/population/metro/
- 26.Minnesota Population Center and State Health Access Data Assistance Center, Integrated Health Interview Series: Version 5.0. Minneapolis: University of Minnesota; 2012. [Google Scholar]
- 27.McCaig LF, Burt CW, Schappert SM, et al. NHAMCS: does it hold up to scrutiny? Ann Emerg Med. 2013;62(5):549–551. doi: 10.1016/j.annemergmed.2013.04.028. [DOI] [PubMed] [Google Scholar]
- 28. [Accessed November 28, 2014];2010 NHAMCS Micro-data File Documentation. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHAMCS/.
- 29.Jasek JP, Hosseinipour N, Rubin T, Lall R. Using syndromic emergency department data to augment oral health surveillance. Online J Public Health Inform. 2013;5(1):e112. [Google Scholar]
- 30. [Accessed November 28, 2014];Understanding the Economy: Unemployment among Young Workers. A Report by The U.S. Congress Joint Economic Committee. Published May 2010. http://www.jec.senate.gov/public/?a=Files.Serve&File_id=adaef80b-d1f3-479c-97e7-727f4c0d9ce6.
- 31.Vujicic M, Nasseh K, Wall T. Research Brief. Health Policy Resources Center. Chicago, IL: American Dental Association; 2013. Feb, Dental Care Utilization Declined for Adults, Increased for Children during the Past Decade in the United States. [Google Scholar]
- 32. [Accessed November 28, 2014];Ambulatory care sensitive conditions. National Quality Measure Clearinghouse AHRQ. http://www.qualitymeasures.ahrq.gov/content.aspx?id=47604.
- 33.Licata R, Paradise J. Oral Health and Low-Income Nonelderly Adults: A Review of Coverage and Access. Policy Brief. [Accessed November 28, 2014];Kaiser Family Foundation’s Commission on Medicaid and the Uninsured. Published June 2012 http://kaiserfamilyfoundation.files.wordpress.com/2013/01/7798-02.pdf.
- 34.Myers J. [Accessed November 28, 2014];The Rundown: How Have Medicaid Dental Benefits Changed in Your State? PBS; aired Nov 17, 2011. http://www.pbs.org/newshour/rundown/how-have-medicaid-dental-benefitschanged-in-your-state-1/. [Google Scholar]
- 35.Cohen LA, Manski RJ, Hooper FJ. Does the elimination of Medicaid reimbursement affect the frequency of emergency department dental visits? J Am Dent Assoc. 1996;127(5):605–609. doi: 10.14219/jada.archive.1996.0272. [DOI] [PubMed] [Google Scholar]
- 36.Neely M, Jones JA, Rich S, Gutierrez LS, Mehra P. Effects of cuts in Medicaid on dental-related visits and costs at a safety-net hospital. Am J Public Health. 2014;104(6):e13–e16. doi: 10.2105/AJPH.2014.301903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bailit H, Beazoglou T, Demby N, et al. Dental safety net: current capacity and potential for expansion. Journal of the American Dental Association. 2006;137(6):807–815. doi: 10.14219/jada.archive.2006.0294. [DOI] [PubMed] [Google Scholar]
- 38.United States Government Accountability Office. Extent of Dental Disease in Children Has Not Decreased and Millions Are Estimated to Have Untreated Tooth Decay. GAO-08-1121. Washington, DC: 2008. Sep, [Google Scholar]
- 39.EPSDT Overview. EPSDT Program Background. [Accessed November 28, 2014];US Department of Health and Human Services. Health Resources and Services Administration. Maternal and Child Health. http://mchb.hrsa.gov/epsdt/overview.html.
- 40. [Accessed November 28, 2014];CHIP Benefits. Medicaid.gov. http://www.medicaid.gov/chip/benefits/chip-benefits.html.
- 41.Okunseri C, Pajewski NM, Brousseau DC, et al. Racial and ethnic disparities in nontraumatic dental-condition visits to emergency departments and physician offices: a study of the Wisconsin Medicaid program. J Am Dent Assoc. 2008;139(12):1657–1666. doi: 10.14219/jada.archive.2008.0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Okunseri C, Pajewski NM, Jackson S, Szabo A. Wisconsin Medicaid enrollees' recurrent use of emergency departments and physicians' offices for treatment of nontraumatic dental conditions. J Am Dent Assoc. 2011;142(5):540–550. doi: 10.14219/jada.archive.2011.0224. [DOI] [PubMed] [Google Scholar]
- 43.Cooper RJ. NHAMCS: does it hold up to scrutiny? Ann Emerg Med. 2012;60(6):722–725. doi: 10.1016/j.annemergmed.2012.10.013. [DOI] [PubMed] [Google Scholar]
- 44.Health Centers and the Affordable Care Act. [Accessed November 28, 2014];Department of Health and Human Services. Health Resources and Services Administration. The Bureau of Primary Health Care. http://bphc.hrsa.gov/about/healthcenterfactsheet.pdf.
- 45. [Accessed November 28 2014];Patient Protection and Affordable Care Act Pub. L. No 111-148, 124 Stat. 119 (March 23(2010). S 1302: Essential Health Benefits Requirements. http://www.gpo.gov/fdsys/pkg/BILLS 111hr3590enr/pdf/BILLS-111hr3590enr.pdf.
- 46.Beltran-Aguilar ED, Barker LK, Canto MT, et al. Surveillance for dental caries, dental sealants, tooth retention, edentulism, and enamel fluorosis--United States, 1988–1994 and 1999–2002. MMWR Surveill Summ. 2005;54(3):1–43. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.