Abstract
Recent trends of population aging and globalization have required an increasing number of individuals to act as long distance caregivers (LDCs) to aging family members. Information technology solutions may ease the burden placed on LDCs by providing remote monitoring, easier access to information and enhanced communication. While some technology tools have been introduced, the information and technology needs of LDCs in particular are not well understood. Consequently, a needs assessment was performed by using video conferencing software to conduct semi-structured interviews with 10 LDCs. Interviews were enriched through the use of stimulus materials that included the demonstration of a prototype LDC health management web/mobile app. Responses were recorded, transcribed and then analyzed. Subjects indicated that information regarding medication regimens and adherence, calendaring, and cognitive health were most needed. Participants also described needs for video calling, activity data regarding sleep and physical exercise, asynchronous communication, photo sharing, journaling, access to online health resources, real-time monitoring, an overall summary of health, and feedback/suggestions to help them improve as caregivers. In addition, all respondents estimated their usage of a LDC health management website would be at least once per week, with half indicating a desire to access the website from a smartphone. These findings are being used to inform the design of a LDC health management website to promote the meaningful involvement of distant family members in the care of older adults.
Introduction
2011 marked a critical milestone for Americans; the first set of baby boomers reached the age of retirement. For the first time in the United States’ history, the number of adults age 65 and older exceeded the number of children under the age of 5. By 2014, the percentage of the population age 65 and older will reach an all-time high of 14%; double the proportion that was seen in the 1940’s 1. As this process of population aging unfolds, the problems associated with caring for unprecedented numbers of older adults become increasingly apparent. Unparalleled demand will be placed not only upon the US healthcare system, but also, upon the millions of family members, friends, and neighbors that provide unpaid care to elderly loved ones. These individuals, often referred to as informal caregivers2, form “the backbone for much of the care that is received by older adults in the United States”3. In an increasingly global society, geographic separation presents a significant challenge to many as they strive to provide care from afar. Challenges such as inadequate methods of communication, living in different time zones, and lack of familiarity with a loved one’s surroundings may all combine to prevent a long distance loved one from providing care4. Such separation often increases the burdens of time, cost, and emotional strain upon the caregiver5. In the last few years, it has been suggested 6,7 that internet technologies have matured insomuch that they may prove to be viable options for providing support to long distance caregivers (LDCs). Such an approach however, remains understudied.
Some early research has focused on identifying information needs of caregivers for individuals with dementia 8,9, while others have focused on providing appropriate information regarding how to care for other specific illnesses/conditions10,11. One promising study, conducted by the National Alliance of Caregiving and United Healthcare 12, investigated caregivers ranking of various health IT tools to support them in their care. This study, measured perceived benefits and barriers of 12 technologies for both in-home and out-of-home caregivers. Systems that allowed for personal health record tracking, caregiving coordination and medication support had high levels of perceived benefits and lower levels of perceived barriers. We suggest that these and other caregiving tools may be especially useful in the context of a smart home in which older adults are monitored using unobtrusive sensors to track various health metrics.
Recently, work13, has been undertaken to provide a better understanding of the prevalence of technology use by out-of-home caregivers in the United States. Current estimates indicate that about one third of out-of-home caregivers use health IT in their caregiving activities. An interesting contrast is found however, in that even among “technology nonusers”, over 70% of LDCs expressed an interest in using technology in their caregiving responsibilities. The incongruence between interest to use health IT tools and actual usage may be explained by barriers such as perceived cost, potential resistance by the care recipient12, and a lack of user-centered focus in the design and implementation of current LDC systems13.
In the interest of promoting higher levels of usage and utility, we resolved to use a user-centered-design approach to assess information needs and discern important usability principles in the design and development of health IT tools for LDCs. The research outlined below is innovative, due to the fact that no studies have specifically looked at the information needs and technology preferences of LDCs by providing caregivers an opportunity to openly discuss their needs and preferences. Furthermore, our study is unique in that we are investigating information needs in the context of a smart home, containing multiple sensors that provide important data streams about activity, cognition, and physiologic parameters. Investigating LDC needs from this perspective provides us with additional information that will enable us to better understand the emerging needs of caregivers living in an increasingly “electronic” world.
Methods
Due to the exploratory nature of this research, qualitative methods were chosen. Since our subject recruitment pool contained individuals throughout the United States, we chose to conduct semi-structured interviews via Skype as the primary method of data collection. We chose Skype over a traditional telephone as we felt that the face-to-face interaction would help subjects to feel more at ease when talking to an unfamiliar person. The use of Skype also helped us to detect any visual cues that may not have been as apparent via a phone call and allowed us to visually present questions and stimulus materials to subjects as we spoke with them. Skype also served as an ideal platform for data collection due to the fact that all communications are encrypted using robust encryption algorithms.
Prototype Development
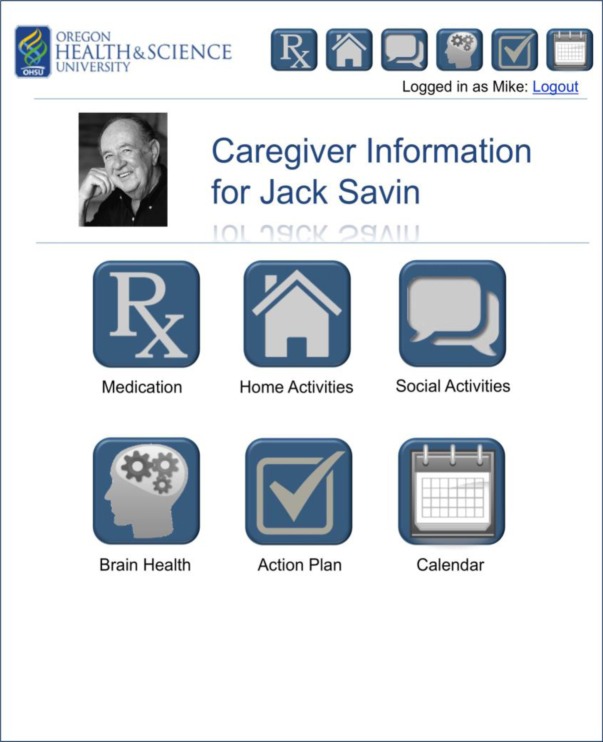
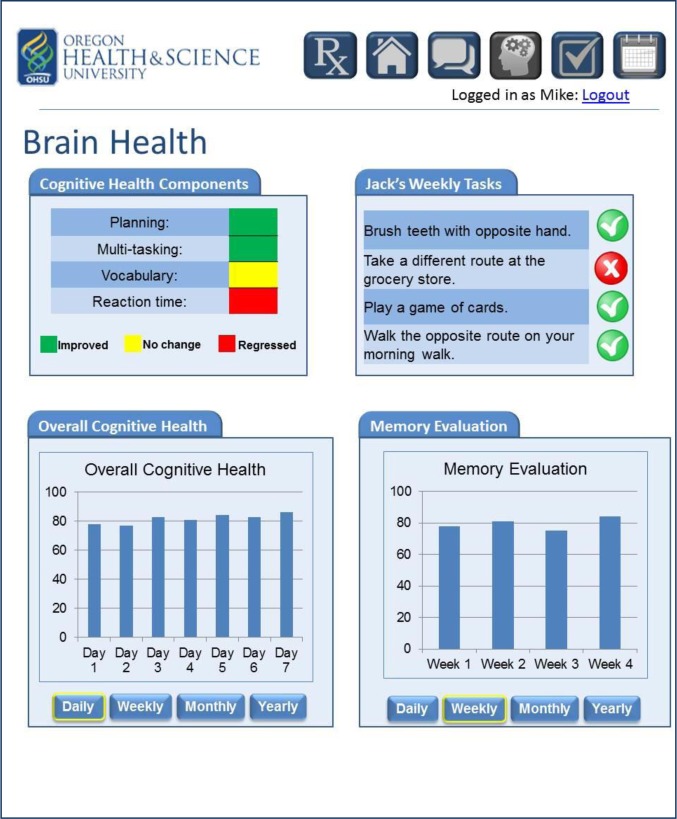
In keeping with other qualitative research,14,15 we elected to develop basic prototypes of a caregiver web (shown in Figures 1 & 2) and mobile app as stimulus materials to facilitate and further enrich our discussions. This approach was chosen due to the limited availability of remote caregiving systems and the anticipated lack of familiarity with the types of data that may be collected in a smart home environment. In an attempt to intelligently develop an initial prototype that delivered an optimal user experience, we drew upon the following four data sources for guidance:
Well established usability principles from the human computer interaction literature
Scientific articles that specifically described caregiving systems/prototypes
Existing commercial systems designed to be used by caregivers
Usability experts within our institution
Figure 1:
Screen shot showing splash page from prototype caregiver web app
Figure 2:
Screen shot showing the brain health page from prototype caregiver web app
Based upon our review of the literature and existing systems, we begun development of an initial mockup using Microsoft PowerPoint. During this process, usability experts within our institution were also consulted. To provide caregivers with a better understanding of system functions, we opted to make parts of the mockup interactive. This was accomplished using transitions and animations within the PowerPoint slideshow and allowed us to demonstrate behaviors and actions when we clicked on various elements within the user interface.
Interview Guide Development
Careful thought and attention was given to development of an interview guide16. Our guide was developed with the primary goal of facilitating open conversation with the caregivers in our study. As such, we elected to start by asking very broad, open-ended questions which were then followed up with more focused questions and probes when greater clarification was needed. Great care was taken to ensure that questions would be easily understood and would not lead study participants towards a specific idea or thought, but rather to allow them to express their own thoughts freely. Due to the fact that interviews were conducted via Skype, we also elected to display each question on the participants’ screens as they were asked. This allowed each subject to both hear each question audibly as well as see the questions visually. It was our hope that doing so would help to ensure that each question was better understood and would allow respondents to re-read the question as they formulated their response.
After an initial draft of the interview guide was completed, two scholars were asked to review each question for simplicity, readability and neutrality and to suggest changes when necessary. As a final step in development, the interview guide was then used to conduct two mock interviews. This process not only allowed for minor changes to the guide but also helped the research team to practice interviewing techniques before the start of formal data collection.
Study Setting
A network of older adults living in smart homes throughout the Portland, Oregon region has been established as part of our existing cognitive health coaching platform17. Older adults that participate in this health coaching platform are continuously monitored using various health tracking sensors. Areas of study include:
Medication adherence and reminding - measured by a camera embedded pillbox
Socialization - measured by phone, Skype and email monitors
Sleep quality - measured using mattress pressure sensors
Cognitive health - measured by cognitive computer games
Because the socialization module encourages the use of the telephone, email and Skype video calling, each older adult in the socialization intervention had previously chosen a remote partner with whom they would regularly communicate. These individuals in turn agreed to provide remote support to the older adults in our project. All remote partners lived in a location different than the older adult and were generally a close friend or family member. A group of 11 subjects was recruited from within this pool of remote partners as participants in our needs assessment.
Data Collection
Each participant was contacted initially via telephone and then later interviewed for approximately 45 minutes. Due to geographic separation between the subjects and the researchers and as all enrolled LDCs were familiar users of the Skype video conferencing software, interviews were conducted remotely through the use of this system. Initially, a short introduction was given in which the purpose of the study and each subject’s role was clearly explained. An emphasis was placed on the fact that subjects could ask questions or make suggestions at any time. Next, subjects were asked to introduce themselves and to describe some of the challenges that they had encountered as they strived to provide care from a distance. Respondents were then asked which types of information are most important to them as caregivers. Next, subjects were asked to identify ways in which technology might serve to ease some of the burdens encountered by LDCs.
After respondents answered these questions, stimulus materials including sample screen-shots for web and smartphone based health management were displayed using Skype’s screen sharing feature. These materials enriched discussion and provided subjects with a real world example of ways in which technology could help them to provide care. In particular, subjects were shown a prototype website in which sensor data regarding medication adherence, socialization, calendaring, sleep quality, and cognitive health was presented using easily understood language and graphics. Tips and suggestions for how to help the older adult were also displayed. After presenting the prototype, discussion was facilitated by the presentation of thoughtful questions designed to promote feedback about key areas of interest (e.g. estimates regarding level of usage, importance of mobile devices, design recommendations). Finally, each subject was asked for any additional comments or suggestions regarding site design and types of information available. Each interview was recorded, transcribed, and subsequently analyzed by grouping similar thoughts and concepts into appropriate themes and ideas. The findings of our needs assessment will then be used to inform the development of version 2.0 of our prototype. This new and improved prototype will then be used in a usability study investigating the way that real world users interact with the proposed application.
Results
Of the 11 subjects that were initially recruited, 10 individuals were successfully contacted and interviewed, with one participant unable to proceed due to lack of a sufficiently reliable internet connection. Of these 10 individuals, 6 were female and 4 were male.
Desired Functionality
Subjects in our study reported that LDCs desire 14 different basic functions: video calling, calendaring, medication tracking, cognitive health tracking, sleep tracking, physical exercise tracking, access to medical records, asynchronous communication, photo sharing, journaling, online health resources, real-time monitoring, an overall summary of wellness, and guidance/feedback regarding the care they provide. These 14 functions are described in Table 1.
Table 1:
Fourteen Basic Functions for Long Distance Caregiving
| Video Calling | Nearly all of the individuals interviewed spoke about the benefits of using videoconferencing software such as Skype to communicate with the older adult under their care. Four individuals spoke of the value of nonverbal communication that is not available over a regular telephone call. The participants’ thoughts regarding this matter are well summarized by the comment “Now, instead of hearing how she’s doing, I can see how she’s doing. It’s one thing to tell someone how you’re doing but it’s a little harder to look at someone and tell them that you’re feeling good when you’re not.” In addition, one interviewee talked about the benefits of being able to show objects over video rather than simply describing them. Some frustration was expressed that this was only a valuable form of communication when there were not technological barriers such as unreliable internet connections, audio dropouts or pixelated video. |
| Calendaring | Six individuals indicated that a shared calendar would be useful to them in their caregiving responsibilities. Respondents were especially interested in being able to view upcoming doctors’ appointments and any planned trips or outings. One person commented that “to [her] the calendar would not be at all useful because digital calendars are cumbersome”. Another commented that “it might take a bit of switching going from a paper calendar to an electronic one but I think I can convince my mom to switch”. The comment was also made that it would be useful for older adults to see a very high level version of the caregiver’s calendar so that the older adults could be reminded of times that the LDC would not be available and the care recipient would know to contact somebody else if a concern arose. The idea that the calendar could be used to coordinate care by multiple LDCs was also mentioned. This would allow multiple individuals to share the responsibilities of caregiving rather than a single individual being expected to carry the burden for the majority of care. |
| Medication Tracking | Four individuals indicated that information regarding medication adherence was very important to them. In addition, the importance of knowing the older adult’s medication list and regimen was also mentioned. Respondents made comments such as “medications are a big concern” and “if you’re not taking your medication, everything else would fall apart”. One individual, however, said that medication information was the least important of all the types of information presented. He commented that this was due to the fact that using images obtained from a camera embedded inside a pill box did not really indicate if the medication had actually been taken. In his words “they could take it out of the box but then not really take it”. |
| Cognitive Health Tracking | Four interviewees suggested that data regarding cognitive health was very important to them. Two of these individuals indicated that this information would be especially interesting to them if it could be presented over a long period of time allowing the caregiver to track any problems. In the words of one subject, “as he gets older, I especially worry about his brain and memory”. |
| Sleep Tracking | Three respondents spoke of the importance of knowing if and when an older adult was experiencing difficulty sleeping. Each of them expressed concern that inadequate sleep can then lead a large number to other problems/concerns. One interviewee described the utility of a system that would automatically alert her after her loved one had experienced multiple consecutive nights of poor sleep so that she could call and check on the older adult and then intervene if necessary. |
| Physical Exercise Tracking | The importance of knowing whether or not an older adult is regularly exercising was also mentioned. Caregivers wanted to know that the older adult in their care was able to regularly exercise. Along with this information need one caregiver also mentioned the importance of knowing certain metrics of physical ability such as strength and balance. |
| Medical Records Access | Two LDCs asked about the possibility of being able to access the older adult’s medical information and test results. They expressed a desire to be more informed and involved in the older adult’s medical care because ”sometimes if we don’t go with him/her, then his/her story doesn’t make sense”. |
| Asynchronous Communication | Many of the LDC’s interviewed spoke about the need and value that comes from asynchronous communication. Whether this communication was via e-mail, text message, instant message etc. seemed to be less important than the ability to communicate asynchronously. This was important to |
| Asynchronous Communication (continued) | them because it allowed them to communicate with the older adults without having to worry about the time of day (e.g. too early, too late, while the older adult was busy). One respondent also said that this form of communication allowed the care recipient to communicate with him without worrying about disrupting him at work. |
| Photo Sharing | The ability to share photographs was mentioned in a few different interviews as an important form of communication. Two LDCs spoke about the value of being able to send pictures back and forth. These individuals mentioned that seeing pictures helped to bridge the gap between caregiver and care recipient and made them feel more involved in each other’s lives. |
| Journaling | Two caregivers spoke about some sort of electronic caregiving journal that would allow for note taking and could be used to keep track of items that may not be included within the caregiving application. One suggested that the journal could be tied to a calendar so that reminders could also be integrated within the journaling feature. |
| Online Health Resources | Multiple caregivers talked about the importance of being able to access reliable health information electronically. Caregivers described medical websites as an important resource that they could use to research a specific condition or illness and then share the pertinent information with the older adult. |
| Real-time Monitor | The need for a real-time indication of an older adults status was described throughout our conversations with LDCs. Caregivers were especially interested to know if an older adult had fallen or was in immediate need of help. Conversely, caregivers also wanted to know when the older adult was doing well and no intervention was needed on their part. One caregiver talked about a system that could not only communicate when their help was needed but also “how badly [the care recipient] needed help”. |
| Summary Metric of Overall Wellness | While many caregivers saw the value in providing data regarding individual items (e.g. medication, sleep, etc.) they also expressed a need for a summary metric that could be an overall indicator of wellness. This would allow caregivers the ability to look at a single graph and see a general trend of wellness over time. |
| Feedback/Guidance | Over half of the respondents talked about the importance of providing guidance and feedback. Not only is it important to provide monitoring data to caregivers, but it is essential to also provide suggestions of what they as the caregiver can do to provide better care and encourage healthy behaviors by the older adult. One caregiver also spoke about the importance of providing encouragement to caregivers when they logged into the system and tried to play a more active role. |
| Other Suggestions | Some respondents also suggested other types of information that would be useful to them as long distance caregivers. One caregiver suggested the inclusion of “information about hobbies and interests”. He went on to suggest a page in which the older adult could share pictures and information regarding hobbies with the caregiver. Another caregiver was interested in the possibility of including information regarding diet through the use of a “smart refrigerator to track if she needs milk and that sort of thing”. One final suggestion was the ability to send an alert to the older adult. He commented that “Dad hasn’t been drinking enough water lately. It would be really nice if there was some way to remind him with a beep or something.” |
Design Implications
In addition to describing desired functions of an LDC web/mobile app, study participants also shared insights that have important design implications for those seeking to develop such a system. These design implications concern usage patterns, device preferences, data sharing preferences, and the presentation of longitudinal tracking data, described further in Table 2.
Table 2:
Design Implications for a Mobile/Web App for Long Distance Caregivers.
| Usage Patterns | Every individual interviewed expressed optimism about their usage of the proposed system and felt that they would use it on a fairly regular basis. All participants indicated that they would likely use the system at least once per week with three participants indicating that they thought they would use the system “a couple times per week” and two respondents suggesting that they would use the system on a daily basis. Two individuals indicated that they would be much more willing to use the system regularly if “the system had the ability to alert me when there was something that needed my immediate attention”. Some LDCs estimated that their usage would be heavily tied to the health of the older adult under their care. They suggest that when the older adult was healthy they would be less likely to have any concerns and would not use the system as regularly. In contrast, they felt they would use the system much more frequently when the older adult’s help was concerning to them. While not as valuable as actual usage data, these expected usage patterns provide valuable information regarding the overall flow and design of a caregiver website. Such high frequency of usage would suggest the need to design a dashboard that would allow the caregiver to quickly check an older adults condition without the need to click on each individual category. Also, as noted by two of our participants, an intelligent alerting system that drew the caregiver’s attention to potentially worrisome data would be ideal. If alerts are to be used however, the authors urge that a great deal of care be taken so as to not inundate caregivers with false alarms as this is likely to lead to alert fatigue. |
| Device Preferences | Of our sample, half of the respondents indicated that they would be likely to access the LDC website from a smartphone. This closely mirrors smartphone adoption data for the US population during the time that the interviews were performed. As such, we expect an increasing proportion of caregivers to request smartphone compatibility for a caregiver website. Of those that desired smartphone compatibility, many talked of the convenience and importance of having access to the system while traveling either to/from work or while on vacation. These participants described use cases in which a smartphone would be used while on the go but a traditional PC would still be the preferred choice if available (i.e. when at home). Such usage in which both a smartphone and a traditional PC are used interchangeably requires a consistent look and feel, as well as similar functionalities and feature sets regardless of which device is used to access the site. In addition, due to respondents reporting high levels of expected usage, a mobile app is recommended in lieu of a smartphone compatible website. Such an approach allows caregivers to view historical data even when no data connection is available and allows for more sophisticated alerts to be displayed when necessary. Identified barriers to using a smartphone to access the LDC website were a small screen and relatively high costs of ownership and usage. However, we expect these concerns to fade somewhat as smartphone manufacturers/providers continue to shift towards larger screen sizes and lower cost devices/services. |
| Data Sharing Preferences | A few caregivers expressed concern that due to the sensitive nature of health data, their older adult may not be willing to share all of the different types of information with them. Though this was not confirmed by discussing data sharing preferences with older adults in our study, we suggest that any such system provides a way in which older adults are able to control the visibility of the data collected. It was also suggested that older adults may be more willing to share monitoring data if the system is implemented before they are facing serious health challenges. In the words of one subject “It might be better to start them when they don’t need it because if you start too late then they may not want to do it. I guess it’s one of those things that if they sense that they aren’t doing well then they will resist that.” As such, we recommend the early implementation of health monitoring systems as a possible way to mitigate this challenge. Such an approach also has the added benefit of collecting longitudinal data while an individual is still healthy so that there is a greater likelihood of early detection when problems arise. |
| Longitudinal Tracking | Caregivers reacted favorably to the idea that longitudinal data could be presented in a meaningful way. They recognized the value of being able to look at data over different periods of time to identify potential areas of concern. As one subject put it “looking by week or month that data is very useful. What I keep trying to get in my head is the progression …seems like this is a great tool to know their decline”. While we agree that there is likely value in providing longitudinal data to caregivers, we also expressed concern about the possibility of either misinterpretation or over interpretation of these data. Contributing to this is the fact that many data streams from current smart home environments are fairly noisy. These concerns may be mitigated somewhat through the use of data smoothing algorithms and clear indications to the caregiver when specific scores are vastly different from an individual’s baseline. |
| Caregiving Terminology | Very few individuals that we interviewed identified themselves as either a long distance caregiver or a caregiver in general. Many individuals expressed that they thought of a caregiver playing a more hands-on role that was not possible from a distance and instead viewed themselves as a helper, friend or family member. While we feel that it would be healthy to help redefine the lay definition of what constitutes a caregiver, we also recognize a need to properly frame any communication with LDCs in language that they understand and can relate to. |
Overall Impressions
The overall reaction from caregivers was very positive with many making comments such as “I think this is a great idea” and “This is going to be really helpful for people like me”. Though individuals suggested the improvements detailed above, none of the participants thought that building a web site/app for LDCs was a generally bad idea. In addition to the expected benefits of being able to ease the burden of providing care and improve involvement of LDCs, a few other benefits were suggested. One caregiver remarked that the system would “help [her] not feel so guilty for living so far away”. It was also suggested that such a system would help older adults because “having us involved helps her to feel loved and valued”. Even when an older adult already lives near family members, one individual suggested that “I can help my mom and uncle by alleviating some of their stress. If there’s something going on I can let them know and have them go visit her”. At the conclusion of one of the interviews, one caregiver became emotional as he spoke of the privilege of being able to care for his aging parents as they “experience this amazing process of the end of life” and suggested that a LDC website would allow him to do that more effectively.
Discussion
After conducting qualitative semi-structured interviews with 10 subjects, we identified 14 different functions that LDCs desire (video calling, calendaring, medication tracking, cognitive health tracking, sleep tracking, physical exercise tracking, access to medical records, asynchronous communication, photo sharing, journaling, online health resources, real-time monitoring, an overall summary of wellness, and guidance/feedback regarding the care they provide). We also identified 4 important design implications concerning LDC usage patterns, device preferences, data sharing preferences, and the presentation of longitudinal tracking data. Overall, we found that participants reacted very positively to the proposed system.
These results are concordant with previous studies that have investigated the role of technological solutions for caregivers. Our findings are similar to those of The National Alliance for Caregiving (NAC)12 who also identified health record tracking, medication support tools, caregiving coordination tools, interactive systems for physical, mental and leisure activities, a symptom monitor and transmitter, a video phone system and a caregiving decision support tool as some of the most important tools for caregivers. Though described by our respondents using different terminology, many of the desired features identified in our study are functionally very similar. One feature listed in the NAC that was not reported by our study is the need for caregiver training simulations. While it is possible that this feature is also desired by LDCs, we note that the NAC study involved both long distance and in-home caregivers and this feature in particular may be more important to individuals serving as traditional “hands-on” caregivers. We also identified some desired features that have not been suggested previously and identified design implications that we believe are important for those looking to develop successful LDC systems.
During the planning of this study, there was some concern that presenting the prototype to interview participants may bias our findings. We expected that we might lead interviewees to talk about the information needs that we anticipated them to have rather than actual information needs. We were surprised to find that while some participants did not speak of some types of information until prompted, at least one participant spoke of each type of information need before the prototype was presented to them. This leads us to believe that our approach was indeed appropriate and the prototype served as a probe to elicit deeper understanding rather than serving to bias our respondents. This is reaffirmed by the high level of agreement between our study and previous work.
The overwhelmingly positive reaction towards our prototype system also follows trends found by other researchers13. Our results however, indicate an even higher level of acceptance with 100% of subjects expressing enthusiasm for an LDC system. While somewhat explained by the limitations listed below, we also suggest that such high levels of enthusiasm are the result of high levels of caregiver burden, with many caregivers desperately looking for assistance as they struggle to provide for loved ones.
Limitations
While we feel that the findings of this study are indeed useful, our choice of methodology and sample population created some important limitations that should be considered. These include:
Small Sample/Lack of Diversity - Though not as important due to our use of qualitative methods, our sample size was still very small (N = 10) and had limited inclusion of ethnic minorities. Also, the LDCs in our study only provided care to older adults that had displayed little to no cognitive impairment
Pro-technology - Study participants were drawn from a pool of technology using seniors and LDCs and are likely more receptive to new technologies than the general population.
Hesitant to criticize - Study participants may have been unwilling to provide a critical analysis of our prototype for fear of offending members of the research team.
Unable to Discern Needs - It is unclear if subjects are entirely aware of their own needs. As with many needs assessments, there is concern that individuals are unable to identify specific needs, choosing instead to be content with their currently available toolset. This may be especially true when discussing a new technology that subjects have not had the opportunity to use in the real world. During our interviews, this was evident when individuals responded that they were not sure whether or not they would need a particular type of information.
As such, we stress the importance of conducting future research to address these limitations by investigating what other information needs are required by other caregiving populations and by trying to answer our research questions with complementary methodologies.
Despite these limitations, many valuable themes emerged that we hope will prove useful as we strive to provide LDCs with new information technology tools. It was very encouraging to find that all 10 individuals interviewed suggested that building a LDC web/mobile app would be accepted positively. Equally encouraging were indications that the proposed application may be used on a regular basis. However, perceived usefulness and usage may not be accurate indicators of actual system usage and utility.
While this study has identified information types that are likely to be useful and valuable to individuals providing care from afar, the best methods for presenting these data to caregivers warrants further exploration. In addition, while the ability to access an older adult’s medical information and test results has been suggested as a useful feature, limitations regarding privacy of medical data may prove to be substantial hurdles.
Future Research
The work described here is the initial step in a larger effort to better understand the role that heath IT can play in assisting caregivers. Our future research will use these findings to improve our existing prototype. As shown in Figure 3, these improvements, along with making the prototype fully interactive will allow us to enter an iterative usability testing and development phase during which users will be asked to use our prototype to perform various tasks. This iterative cycle of development will then allow us to create a final caregiver web/mobile app that is both useful and user-friendly. This out will then be evaluated by means of an intervention study. Both quantitative and qualitative methods will be used to determine the impact that our caregiver application makes in the real world. These data will then be synthesized into design recommendations and lessons learned for future researchers interested in the field of technology enhanced caregiving.
Figure 3:
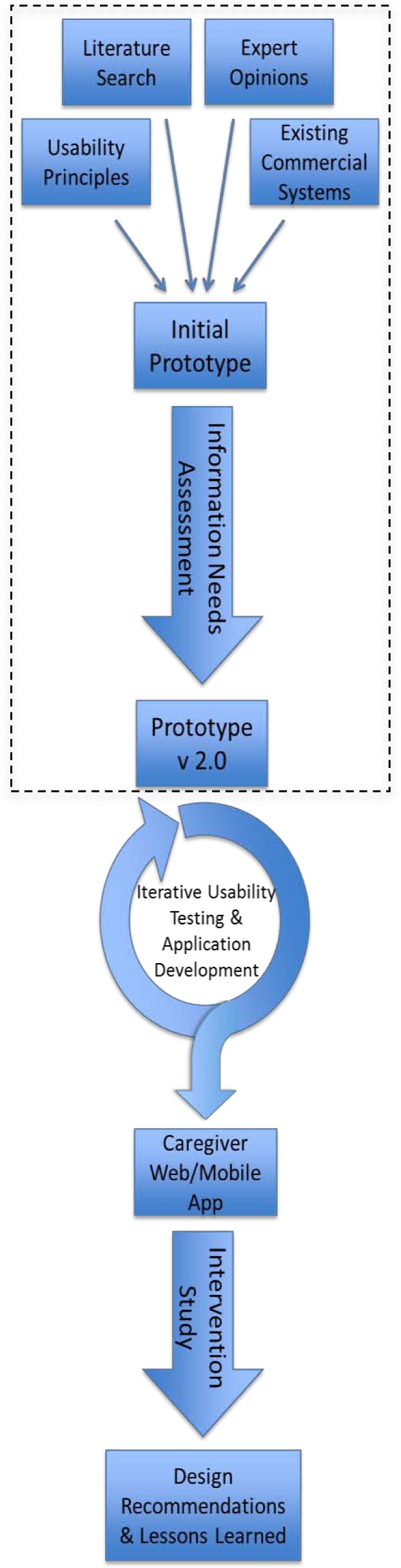
Long term research plan for development and evaluation LDC web/mobile app (dashed box designates work described in this paper)
Conclusion
The information needs of long distance caregivers are extensive and may vary somewhat depending upon the health problems of the care recipient. LDCs described needs for video calling, calendaring, data regarding medication, sleep, physical exercise and cognitive health, asynchronous communication, photo sharing, journaling, access to online health resources, real-time monitoring, an overall summary of health, and feedback/suggestions to help them improve as caregivers. We feel confident that we have obtained sufficient preliminary data to justify the continued development of a long distance caregiver application with the final goal of conducting a field trial of such a system in the real world.
References
- 1.Administration on Aging: Department of Health & Human Services Projected Future Growth of the Older Population [Internet] Administration on Aging. [cited 2014 Jan 15]. Available from: http://www.aoa.gov/aoaroot/aging_statistics/future_growth/future_growth.aspx.
- 2.Donelan K, Hill CA, Hoffman C, Scoles K, Feldman PH, Levine C, et al. Challenged To Care: Informal Caregivers In A Changing Health System. Health Aff (Millwood) 2002 Jul 1;21(4):222–31. doi: 10.1377/hlthaff.21.4.222. [DOI] [PubMed] [Google Scholar]
- 3.Retooling for an Aging America: Building the Health Care Workforce - Institute of Medicine[Internet] [cited 2012 Nov 13]. Available from: http://www.iom.edu/Reports/2008/Retooling-for-an-Aging-America-Building-the-Health-Care-Workforce.aspx.
- 4.Mazanec P, Daly BJ, Ferrell BR, Prince-Paul M. Lack of Communication and Control: Experiences of Distance Caregivers of Parents With Advanced Cancer. Oncol Nurs Forum. 2011 May;38(3):307–13. doi: 10.1188/11.ONF.307-313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bevan JL, Sparks L. Communication in the context of long-distance family caregiving: An integrated review and practical applications. Patient Educ Couns. 2011 Oct;85(1):26–30. doi: 10.1016/j.pec.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 6.Benefield LE, Beck C. Reducing the distance in distance-caregiving by technology innovation. Clin Interv Aging. 2007 Jun;2(2):267–72. [PMC free article] [PubMed] [Google Scholar]
- 7.Rosland A-M, Heisler M, Janevic MR, Connell CM, Langa KM, Kerr EA, et al. Current and potential support for chronic disease management in the United States: the perspective of family and friends of chronically ill adults. Fam Syst Health J Collab Fam Healthc. 2013 Jun;31(2):119–31. doi: 10.1037/a0031535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Czaja SJ, Rubert MP. Telecommunications Technology as an Aid to Family Caregivers of Persons With Dementia. Psychosom Med. 2002;64(3):469–76. doi: 10.1097/00006842-200205000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Topo P. Technology Studies to Meet the Needs of People With Dementia and Their Caregivers. J Appl Gerontol. 2009;28(1):5–37. [Google Scholar]
- 10.Koenig KN, Steiner V, Pierce LL. Information Needs of Family Caregivers of Persons With Cognitive Versus Physical Deficits. Gerontol Geriatr Educ. 2011;32(4):396–413. doi: 10.1080/02701960.2011.611713. [DOI] [PubMed] [Google Scholar]
- 11.Washington KT, Meadows SE, Elliott SG, Koopman RJ. Information needs of informal caregivers of older adults with chronic health conditions. Patient Educ Couns. 2011;83(1):37–44. doi: 10.1016/j.pec.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 12.National Alliance for Caregiving; e-Connected Family Caregiver: Bringing Caregiving into the 21st Century; 2011. [Google Scholar]
- 13.Zulman DM, Piette JD, Jenchura EC, Asch SM, Rosland AM. Facilitating Out-of-Home Caregiving Through Health Information Technology: Survey of Informal Caregivers’ Current Practices, Interests, and Perceived Barriers. J Med Internet Res [Internet] 2013 Jul 10;15(7) doi: 10.2196/jmir.2472. cited 2014 Mar 11. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3713893/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jimison HB, Sher PP, Appleyard R, LeVernois Y. The Use of Multimedia in the Informed Consent Process. J Am Med Inform Assoc. 1998 May 1;5(3):245–56. doi: 10.1136/jamia.1998.0050245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Crilly N, Blackwell AF, Clarkson PJ. Graphic elicitation: using research diagrams as interview stimuli. Qual Res. 2006;6(3):341–66. [Google Scholar]
- 16.Boyce C, Neale P. Conducting in-depth interviews: A guide for designing and conducting in-depth interviews for evaluation input. 2006.
- 17.Jimison HB, Pavel M. Integrating computer-based health coaching into elder home care; Technology and aging: Selected papers from the 2007 International Conference on Technology and Aging; 2008. pp. 122–9. [Google Scholar]