Abstract
Bouveret syndrome is a proximal form of gallstone ileus where a large gallstone lodges in the pylorus or proximal duodenum, having passed through a bilioenteric fistula that has formed secondary to previous cholecystitis. We describe the laparoscopic extraction of a giant ‘Bouveret’ gallstone from the duodenum of an elderly man with morbid obesity.
Background
Gallstone related disease and bowel obstruction are both frequently encountered in emergency surgical practice; seldom does the former cause the latter, and extremely rarely in the foregut. Thus, this condition is rare, and therefore fascinating. Its minimally invasive surgical management is testament to advances in laparoscopic surgery and surgical innovation.
Case presentation
A 77-year-old retired man, an engineer, presented to the accident and emergency department with abdominal pain and profuse vomiting. Three days previously he had developed nausea and heartburn, which progressed into yellow and then dark brown vomiting. This was associated with constant upper abdominal pain that had migrated from left of the midline to the right upper and right lower quadrants. One initial loose stool had preceded 3 days of absolute constipation.
He had a background of hypertension, benign prostatic hyperplasia, and his body mass index of 43 and osteoarthritis significantly limited his mobility.
Examination was limited by his morbid obesity, but his vital signs were normal (pulse 78, blood pressure 130/74 mm Hg, apyrexial), and he only had mild tenderness in his right lower quadrant, with active bowel sounds and soft stool on digital rectal examination.
Investigations
The patient had a haemoglobin of 154 g/L (significantly higher than baseline owing to dehydration), leucocytosis of 17.6×109/L, but CRP of only 18 mg/L. While his creatinine was normal at 116 μmol/L, his urea was slightly elevated at 8.6 mmol/L. His amylase and liver function tests were within normal range apart from bilirubin of 33 μmol/L. Owing to pain and vomiting, he had a mixed alkalosis (pH 7.56, PaCO2 4.2, base excess 5.7 mmol/L, and lactate 1.8 mmol/L) on arterial blood gas analysis.
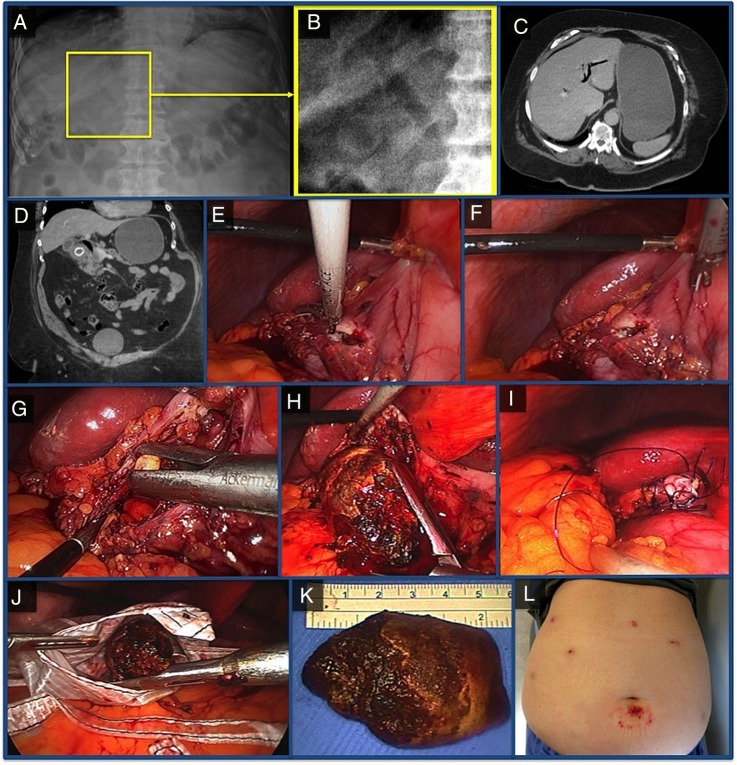
An erect chest radiograph did not show any significant abnormality and, initially, no abnormality of the abdominal radiograph was identified (figure 1A). Differential diagnoses recorded included gastritis, appendicitis and cholecystitis. However, the post take ward round noted the hyperbilirubinaemia, a recent transient phase of dark urine, and, in the right upper quadrant of the abdominal radiograph, pneumobilia and a circumscribed circular opaque lesion were identified (figure 1B). Gallstone ileus was therefore considered, and a CT of the abdomen and pelvis with intravenous contrast confirmed a large calcified gallstone within the second part of the duodenum (figure 1D), causing marked proximal dilation of the duodenum and stomach, associated with a significantly dilated air filled biliary tree (figure 1C).
Figure 1.
Pneumobilia and an opaque ovoid lesion were just visible on the abdominal radiograph (A and B). CT showed a distended stomach, pneumobilia and calcification within a large ectopic gallstone in the duodenum (C and D). Through a pyloroduodentomy (E and F), a small fragment (G), and then a 6 cm gallstone (H, J and K) was extracted. The enterotomy was closed with interrupted PDS (I). A laparoscopic approach had minimised abdominal wall trauma (L).
Treatment
The patient was treated with nasogastric decompression and intravenous crystalloid. Endoscopic extraction of the gallstone was predicted to be too difficult owing to its size, so the patient was taken to theatre for laparoscopic removal.
Five ports were used (2×12 and 3×5 mm), and the omentum was reflected off the liver and duodenum, to display a cholecystoduodenal fistula. The gastric antrum was opened longitudinally (figure 1E, F) with ultrasonic shears (harmonic) to reveal the main gallstone irretrievably positioned beyond the pylorus in the proximal duodenum. The enterotomy was therefore extended into a pyloroduodenotomy, enabling the stones to be extracted through the proximal duodenum (figure 1G, H). A transverse pyloroplasty, incorporating the cholecystoduodenal fistula, was fashioned with interrupted 3/0 PDS (absorbable monofilament) to close the pyloroduodenotomy (figure 1I). There were no visible air leaks following nasogastric insufflation underwater, so an omental patch was placed over the closure with 3/0 PDS. After extensive irrigation, and the insertion of 20Ch Robinson drains into the right subdiaphragmatic and subhepatic spaces, the gallstone was retrieved in a specimen retrieval bag (figure 1J). The wounds were closed with interrupted 2/0 vicryl and 3/0 biosyn.
Outcome and follow-up
Owing to the 6 h operation and high perioperative oxygen requirements, the patient remained intubated and ventilated overnight, but was extubated on postoperative day 1. A fluoroscopic water-soluble contrast meal study showed no leak on day 4, enabling the introduction of oral fluids. A postoperative ileus took several days to settle; therefore the nasogastric tube was only removed and food introduced on day 9. Total parenteral nutrition via PICC line was required until day 12. The subhepatic and subdiaphragmatic drains remained bile free and were removed sequentially on days 9 and 10.
The patient was discharged on day 15, and at outpatient review 2 weeks later, apart from a minor umbilical wound infection, he had made a full recovery with only minimal abdominal scarring (figure 1L).
Discussion
Gallstone ileus occurs when a gallstone of adequate size passes through a cholecystoduodenal fistula or a choledochoduodenal fistula, and impacts within the gastrointestinal tract, typically at the relatively narrow ileocaecal junction, causing distal small bowel obstruction. Bouveret syndrome is gallstone ileus within the duodenum, causing gastric outflow obstruction. It was first described in two patients by Léon Bouveret in 1896,1 and usually presents as epigastric colic, with nausea and vomiting,2 sometimes on a background of biliary symptoms. In a review of 128 cases identifiable within the literature (mostly case reports) in 2006, the mean age was 74, with a female:male ratio of 1.86.3 It is very rare: gallstones only cause about 1% of mechanical intestinal obstructions,4 and almost always obstruct more distally.
Abdominal radiographs of Bouveret syndrome sometimes feature Rigler's triad: pneumobilia (39%), an ectopic gallstone (38%) and a dilated stomach (23%).3 It is worth noting that the size of the offending gallstone is often underestimated if only the calcified portion is measured5; indeed, this patient's 6 cm diameter gallstone had a CT diameter of only 2.1 cm. While ultrasound may be partly diagnostic especially in slim patients, CT is the most useful easily obtainable investigation for establishing the location of the stone, the anatomy of the fistula and the integrity of the gallbladder. For the 20% of gallstones that are isoattenuating, and therefore not visible, conventional T2-weighted MRCP is helpful. One case report concluded some added value in performing gadolinium-based contrast enhanced MRCP.6
Bouveret syndrome can also be diagnosed endoscopically, though in the review of Cappell et al3, the obstructing stone was not visible in a third of cases due to being embedded within the mucosa and causing luminal distortion, and it was only possible to identify the fistula opening in 13% of oesophagogastroduodenoscopies. As an additional test, oral contrast studies may demonstrate a filling defect and the course of the fistula.7
Most cases present with one impacted stone, and its removal can be attempted with limited success endoscopically, often using mechanical, laser or extracorporeal shock wave lithotripsy,3 combined with snares, baskets, biliary balloons and grasping forceps. Most cases, especially for stones greater than 3 cm, therefore require surgery. Open surgical extraction via an enterotomy is the most straightforward procedure.8 Simultaneous cholecystectomy and fistula repair is often difficult, associated with a higher risk of complication,3 and is frequently unnecessary, resulting in many surgeons opting to perform this as a second operation only if the patient is symptomatic.
The successful laparoscopic removal of 4 and 5 cm duodenal gallstones has recently been described.9 10 If feasible, a minimally invasive approach is logical; the patients are frequently elderly and unfit, the mortality from gallstone ileus has been quoted at 30%11 and a laparotomy is often a big insult. With a laparoscopic approach it is essential to identify the location of all significantly sized gallstones pre-operatively on CT; ‘walking’ the small intestine to the ileocaecal valve with a pair of Johan laparoscopic forceps is prudent to exclude residual stones but not as sensitive as manual palpation.
Learning points.
Bouveret syndrome should be considered in any elderly patient with a presentation of foregut obstruction associated with pneumobilia, especially if there has been a history of untreated gallstone disease and no recent biliary surgery or endoscopic retrograde cholangiopancreatography.
The initial radiographic signs were subtle on plain films, but Sosman's well known maxim “You see only what you look for; you recognise only what you know” is particularly pertinent here.
This is the third report of laparoscopic extraction of a ‘Bouveret’ gallstone, but demonstrates for the first time, feasibility when both the patient and gallstone are ‘supersized’.
Regardless of surgical approach, it remains essential to examine the length of the small bowel, to ensure no other stones subsequently obstruct it.
Footnotes
Contributors: RCN, NP and KKS treated the patient. All authors were involved in discussion regarding the subject of the case report, together with the writing, literature review and final draft.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Bouveret L. Sténose du pylore adhérent a la vésicule. Rev Med (París) 1896;16:1–16. [Google Scholar]
- 2.Shah SK, Walker PA, Fischer UM et al. Bouveret syndrome. J Gastrointest Surg 2013;17:1720–1. 10.1007/s11605-013-2244-z [DOI] [PubMed] [Google Scholar]
- 3.Cappell MS, Davis M. Characterization of Bouveret's syndrome: a comprehensive review of 128 cases. Am J Gastroenterol 2006;101:2139–46. 10.1111/j.1572-0241.2006.00645.x [DOI] [PubMed] [Google Scholar]
- 4.Füzün M, Kaymak E, Harmancioğlu Ö et al. Principal causes of mechanical bowel obstruction in surgically treated adults in Western Turkey. Br J Surg 1991;78:202–3. 10.1002/bjs.1800780223 [DOI] [PubMed] [Google Scholar]
- 5.Gan S, Roy-Choudhury S, Agrawal S et al. More than meets the eye: subtle but important CT findings in Bouveret's syndrome. AJR Am J Roentgenol 2008;191:182–5. 10.2214/AJR.07.3418 [DOI] [PubMed] [Google Scholar]
- 6.Algin O, Ozmen E, Metin MR et al. Bouveret syndrome: evaluation with multidetector computed tomography and contrast-enhanced magnetic resonance cholangiopancreatography. Ulus Travma Acil Cerrahi Derg 2013;19:375–9. 10.5505/tjtes.2013.97254 [DOI] [PubMed] [Google Scholar]
- 7.Ariche A, Czeiger D, Gortzak Y et al. Gastric outlet obstruction by gallstone: Bouveret syndrome. Scand J Gastroenterol 2000;35:781–3. 10.1080/003655200750023480 [DOI] [PubMed] [Google Scholar]
- 8.Khan AZ, Escofet X, Miles WF et al. The Bouveret syndrome: an unusual complication of gallstone disease. J R Soc Promot Health 2002;122:125–6. 10.1177/146642400212200216 [DOI] [PubMed] [Google Scholar]
- 9.Yang D, Wang Z, Duan ZJ et al. Laparoscopic treatment of an upper gastrointestinal obstruction due to Bouveret's syndrome. World J Gastroenterol 2013;19:6943–6. 10.3748/wjg.v19.i40.6943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sica GS, Sileri P, Gaspari AL. Laparoscopic treatment of Bouveret's syndrome presenting as acute pancreatitis. JSLS 2005;9:472–5. [PMC free article] [PubMed] [Google Scholar]
- 11.Rodriguez-Sanjuan JC, Casado F, Fernandez MJ et al. Cholecystectomy and fistula closure versus enterolithotomy alone in gallstone ileus. Br J Surg 1997;84:634–7. 10.1002/bjs.1800840514 [DOI] [PubMed] [Google Scholar]