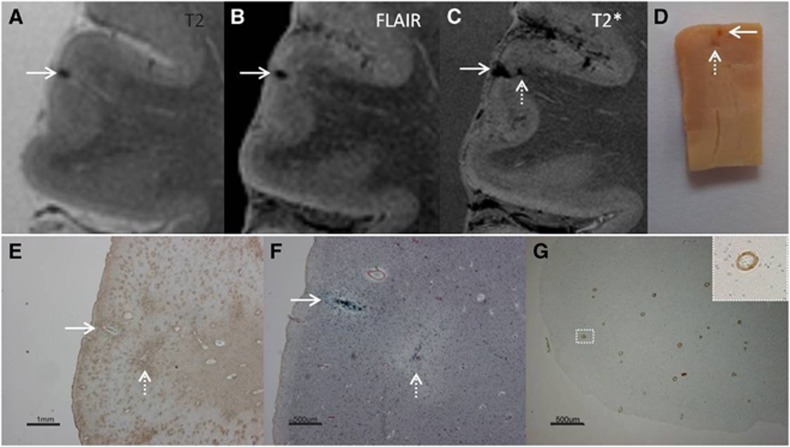
Figure 3.
Intracortical chronic gliotic microinfarct with hemorrhagic components (indicated by arrow), identified on magnetic resonance imaging (MRI), in postmortem brain of a 78-year-old male with moderate Alzheimer pathology (Braak & Braak (BB) IV), Lewy body dementia (B V), and severe cerebral amyloid angiopathy (CAA). The intracortical gliotic microinfarct with hemorrhagic components appeared hypointense on T2 (A), FLAIR (B), and T2* (C) where it was enlarged due to the so-called ‘blooming effect'. This microinfarct was already visible on gross pathology (D, arrow). On Hematoxylin & Eosin (HE) the microinfarct was identified as a region of tissue pallor, with neuronal death, gliosis, and accompanied by hemosiderin-containing macrophages (not shown here). The adjacent sections were positive for GFAP (E), CD68 (not depicted here), and iron (F). We did not observe any collapsed or ruptured vessels in the close proximity of the lesion. An additional microinfarct (indicated by broken arrow) was visible in the same section. This microinfarct was seen on gross pathology, but on MRI it could retrospectively only be matched to a hypointense lesion on T2* (broken arrow). This particular case showed severe CAA, as confirmed by Aβ immunohistochemistry (G; inset is enlargement from area indicated with white square). FLAIR, fluid-attenuated inversion recovery; GFAP, glial fibrillary acidic protein.