Abstract
Introduction
Primary small bowel malignancy is unusual and accounts for 1–3% of all gastrointestinal tract neoplasms. Adenocarcinoma is one of the most common histologic types, but its frequency decreases with more distal locations. Its clinical presentation is nonspecific and is usually associated with advanced disease, which contributes to delayed diagnosis.
Presentation of case
A 66-year-old woman was admitted to the hospital with a 6-day history of progressively worsening abdominal pain localized in the right lower quadrant, nausea, and vomiting. Investigation revealed an inflammatory appendiceal tumor. The patient underwent surgery and an unexpected tumor involving the distal ileal segment and ileocecal appendix was found. Right radical hemicolectomy with en bloc resection of the distal ileum was performed. Histopathological examination revealed adenocarcinoma of the ileum.
Discussion
This rare entity is associated with a nonspecific clinical presentation that contributes to delayed diagnosis and treatment, and consequently to a worse prognosis. Approximately half of the cases are only diagnosed at surgery. Primary treatment consists of wide resection with locoregional lymphadenectomy. The role of adjuvant chemotherapy has yet to be determined.
Conclusion
This case demonstrates an unusual condition characterized by late and challenging diagnosis. We highlight the importance of an earlier diagnosis and optimal treatment for improved patient outcomes.
Keywords: Small bowel neoplasm, Small bowel adenocarcinoma, Adenocarcinoma of the ileum, Right hemicolectomy
Abbreviations: SBA, small bowel adenocarcinoma; CT, computed tomography; MRI, magnetic resonance imaging
Highlights
-
•
Small bowel adenocarcinoma is a rare tumor with a late and challenging diagnosis.
-
•
Primary treatment consists in wide resection with locoregional lymphadenectomy.
-
•
The role of adjuvant chemotherapy has yet to be determined.
-
•
It is crucial an earlier diagnosis and optimal treatment to improve the outcome.
1. Introduction
Primary small bowel malignancy is rare, accounting for 1–3% of all gastrointestinal tract neoplasms. The estimated annual incidence is 2.1 cases per 100,000 persons and is increasing [1,2]. Currently, the most common histologic type is carcinoid (44%), followed by adenocarcinoma (33%), lymphoma (15%), and sarcoma (8%) [2].
Adenocarcinoma of the small bowel (SBA) is an even more rare entity; it is most commonly located in the duodenum (57%), jejunum (29%), and ileum (10%) [3]. Crohn disease and celiac disease are the most important known risk factors, but other associations may exist [2–4].
Adenocarcinoma's clinical presentation lacks specificity, which contributes to an average delay of 6–10 months in diagnosis [2,4,5]. The most common clinical manifestations are nonspecific: abdominal pain, nausea, vomiting, bowel obstruction, occult GI bleeding, and weight loss [4,5].
Advances in imaging and endoscopy have improved the diagnosis of small bowel tumors. Diagnostic studies include upper gastrointestinal barium study (UGI), ultrasonography, computed tomography (CT) scan, magnetic resonance imaging (MRI), video capsule endoscopy, and double-balloon enteroscopy. However, in 30–60% of cases, the diagnosis is only established at surgery, particularly for distally located SBA [3,4,6,7].
Surgery is the primary treatment for locoregionally limited SBA. Wide resection with negative margins and regional lymphadenectomy with adequate lymph node evaluation appears to be the best management. This differs for proximal duodenal tumors, where pancreaticoduodenectomy should be performed, and distal ileal tumors, where right hemicolectomy is indicated [2,8]. The role of adjuvant chemotherapy is still unknown, and prospective studies are needed to address this issue. Some retrospective studies have shown improvement in disease-free survival with the use of adjuvant therapy [6,9,10].
2. Presentation of case
A 66-year-old Caucasian woman with a previous history of dyslipidemia was admitted to the emergency department with a 6-day history of progressively worsening abdominal pain localized in the right lower quadrant, nausea, and vomiting; the vomiting began one day before admission. Anorexia and unquantified weight loss were also present. She had no fever, changes in bowel habits, or urinary symptoms. Physical examination revealed that she was vigilant, oriented, afebrile, and hemodynamically stable. Her abdomen was non-distended, and she had right lower quadrant pain on superficial and deep palpation with tenderness but no guarding or rebound tenderness. Rectal and gynecologic examinations were unremarkable.
Laboratory testing showed no anemia (hemoglobin, 12.3 × 10 g/L) or leukocytosis (white blood cell count, 6.82 × 109/L with 83.9% neutrophils) but indicated elevated C-reactive protein (145.0 mg/L).
Abdominopelvic ultrasonography was complemented with non-contrast-enhanced pelvic CT scan (Fig. 1 and Fig. 2); a 4-cm right lower quadrant mass involving the ileocecal appendix and cecum was identified. Appendiceal wall thickening and periappendiceal fat stranding were evident. No intra-abdominal free fluid, extraluminal air, or fluid accumulation was observed.
Fig. 1.

CT scan image (axial view) showing appendiceal wall thickening.
Fig. 2.

CT scan image (axial view) showing periappendiceal fat stranding.
A diagnosis of inflammatory appendiceal tumor was made, and the patient underwent surgery. At laparotomy, a tumor involving the distal ileal segment and ileocecal appendix was present. The cecal wall was also thickened. There were multiple enlarged lymph nodes in the mesenteric root. No other visible lesions were identified. We performed a right radical hemicolectomy with en bloc resection of the last 70 cm of the ileum and a primary stapled ileocolic anastomosis (Fig. 3). No surgical complications were perceived, so the patient was discharged on the fifth postoperative day.
Fig. 3.
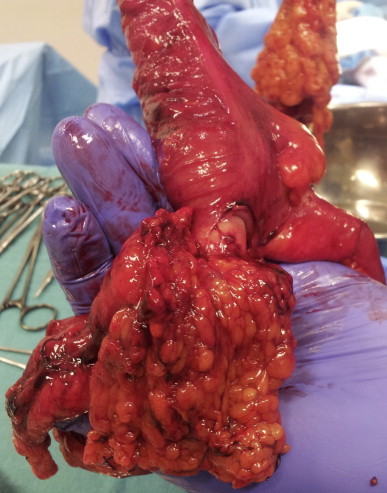
Resected specimen – right hemicolectomy with en bloc resection of distal ileum. Tumor involving ileal segment and ileocecal appendix is noticeable.
Histopathological examination revealed a well-differentiated adenocarcinoma of the ileum invading the mesenteric fat and ileocecal appendix; free surgical margins were achieved. No lymph node involvement was present. The tumor was pathologically staged as pT4pN0. Complete staging was performed and revealed no distant metastasis (M0): stage IIB disease [11].
After multidisciplinary consultation, adjuvant chemotherapy was elected. The patient completed 8 cycles of capecitabine with good tolerance. As of the ninth month of postoperative follow-up, there has been no evidence of recurrent disease.
3. Discussion
Adenocarcinoma of the ileum is a gastrointestinal tumor with a low incidence. Some risk factors are known (e.g., Crohn disease and celiac disease), but many others have only been postulated and are also associated with colorectal cancer. The clinical presentation is nonspecific, and the first symptoms are usually related to advanced disease. The most common symptoms – abdominal pain, nausea, and vomiting – are frequently present with the majority of intra-abdominal conditions. These factors contribute to delayed diagnosis and treatment, and consequently to a worse prognosis.
The most frequently used and reliable diagnostic exam is contrast-enhanced CT scan with appropriate IV and oral protocols, while non-contrast-enhanced CT scan has an inferior accuracy rate “[12].” Many other modalities have also been used. Endoscopic studies, such as double-balloon enteroscopy or video capsule endoscopy, are being increasingly used [13]. Nevertheless, approximately half of the cases are only diagnosed at surgery, mostly because of misdiagnosis.
Currently, the best treatment for this neoplasm is wide resection with lymphadenectomy. When the tumor is located in the distal ileum, a right radical hemicolectomy is preferred to ensure free surgical margins. The role of adjuvant chemotherapy has yet to be determined, especially with regard to the benefits by stage and the ideal therapeutic schema [9].
The outcomes from large studies have shown that, for patients with stage II to III disease who are treated with surgical resection, 5-year overall survival rates range from 27 to 52% [9,14]. These poor outcomes make early diagnosis even more important.
4. Conclusion
Adenocarcinoma of the distal ileum is uncommon and challenging to diagnose, as symptoms are usually late and nonspecific. Right lower quadrant pain is the most frequent symptom, which raises many other more likely conditions as differential diagnoses. CT scan is frequently used after common gastrointestinal disorders have been ruled out, and particularly in elderly patients where the risk of malignancy is higher. However, approximately half of the cases are only diagnosed during surgery. Wide resection with lymphadenectomy is the main treatment; right radical hemicolectomy is the most frequently chosen procedure. The role of adjuvant chemotherapy has not yet been determined. In general, patient outcomes are poor, and an earlier diagnosis is of the uttermost importance.
Ethical approval
None.
Funding
None.
Author contribution
Celso Nabais – Case report design, data analysis and wrote the paper.
Raquel Salústio; Franciso V Sousa; Eusébio Porto; Carlos Cardoso – Reviewed the paper, data analysis and provided expert advice regarding radiological examinations.
Caldeira Fradique – Reviewed the paper and data analysis.
Conflicts of interest
The authors declare, that there is no conflict of interest.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
References
- 1.Howlader N.N.A., Krapcho M., Garshell J., Miller D., Altekruse S.F., Kosary C.L., Yu M., Ruhl J., Tatalovich Z., Mariotto A., Lewis D.R., Chen H.S., Feuer E.J., Cronin K.A. National Cancer Institute; 1975-2011. SEER Cancer Statistics Review.www.seer.cancer.gov [03.11.2014]. Available from: [Google Scholar]
- 2.Shenoy S. Primary small-bowel malignancy: update in tumor biology, markers, and management strategies. J Gastrointest Cancer. 2014;45(4):421–430. doi: 10.1007/s12029-014-9658-z. [DOI] [PubMed] [Google Scholar]
- 3.Halfdanarson T.R., McWilliams R.R., Donohue J.H., Quevedo J.F. A single-institution experience with 491 cases of small bowel adenocarcinoma. Am J Surg. 2010;199(6):797–803. doi: 10.1016/j.amjsurg.2009.05.037. [DOI] [PubMed] [Google Scholar]
- 4.Dabaja B.S., Suki D., Pro B., Bonnen M., Ajani J. Adenocarcinoma of the small bowel: presentation, prognostic factors, and outcome of 217 patients. Cancer. 2004;101(3):518–526. doi: 10.1002/cncr.20404. [DOI] [PubMed] [Google Scholar]
- 5.Talamonti M.S., Goetz L.H., Rao S., Joehl R.J. Primary cancers of the small bowel: analysis of prognostic factors and results of surgical management. Arch Surg. 2002;137(5):564–570. doi: 10.1001/archsurg.137.5.564. discussion 570–561. [DOI] [PubMed] [Google Scholar]
- 6.Guo X., Mao Z., Su D., Jiang Z., Bai L. The clinical pathological features, diagnosis, treatment and prognosis of small intestine primary malignant tumors. Med Oncol. 2014;31(4):913. doi: 10.1007/s12032-014-0913-8. [DOI] [PubMed] [Google Scholar]
- 7.Chang H.K., Yu E., Kim J., Bae Y.K., Jang K.T., Jung E.S., Yoon G.S., Kim J.M., Oh Y.H., Bae H.I. Adenocarcinoma of the small intestine: a multi-institutional study of 197 surgically resected cases. Hum Pathol. 2010;41(8):1087–1096. doi: 10.1016/j.humpath.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 8.Agrawal S., McCarron E.C., Gibbs J.F., Nava H.R., Wilding G.E., Rajput A. Surgical management and outcome in primary adenocarcinoma of the small bowel. Ann Surg Oncol. 2007;14(8):2263–2269. doi: 10.1245/s10434-007-9428-2. [DOI] [PubMed] [Google Scholar]
- 9.Overman M.J., Kopetz S., Lin E., Abbruzzese J.L., Wolff R.A. Is there a role for adjuvant therapy in resected adenocarcinoma of the small intestine. Acta Oncol. 2010;49(4):474–479. doi: 10.3109/02841860903490051. [DOI] [PubMed] [Google Scholar]
- 10.Overman M.J. Recent advances in the management of adenocarcinoma of the small intestine. Gastrointest Cancer Res. 2009;3(3):90–96. [PMC free article] [PubMed] [Google Scholar]
- 11.Edge S., Byrd D.R., Compton C.C., Fritz A.G., Greene F.L., Trotti A. 7th ed. Springer; Boston: 2011. AJCC Cancer Staging Manual. [Google Scholar]
- 12.Horton K.M., Fishman E.K. The current status of multidetector row CT and three-dimensional imaging of the small bowel. Radiol Clin North Am. 2003;41(2):199–212. doi: 10.1016/s0033-8389(02)00121-5. [DOI] [PubMed] [Google Scholar]
- 13.Kulesza J., Meszka M., Rykala C., Pawlak J. Adenocarcinoma of the small bowel – a case report. Pol Przegl Chir. 2014;86(6):285–288. doi: 10.2478/pjs-2014-0050. [DOI] [PubMed] [Google Scholar]
- 14.Cao J., Zuo Y., Lv F., Chen Z., Li J. Primary small intestinal malignant tumors: survival analysis of 48 postoperative patients. J Clin Gastroenterol. 2008;42(2):167–173. doi: 10.1097/01.mcg.0000248014.78020.7a. [DOI] [PubMed] [Google Scholar]


