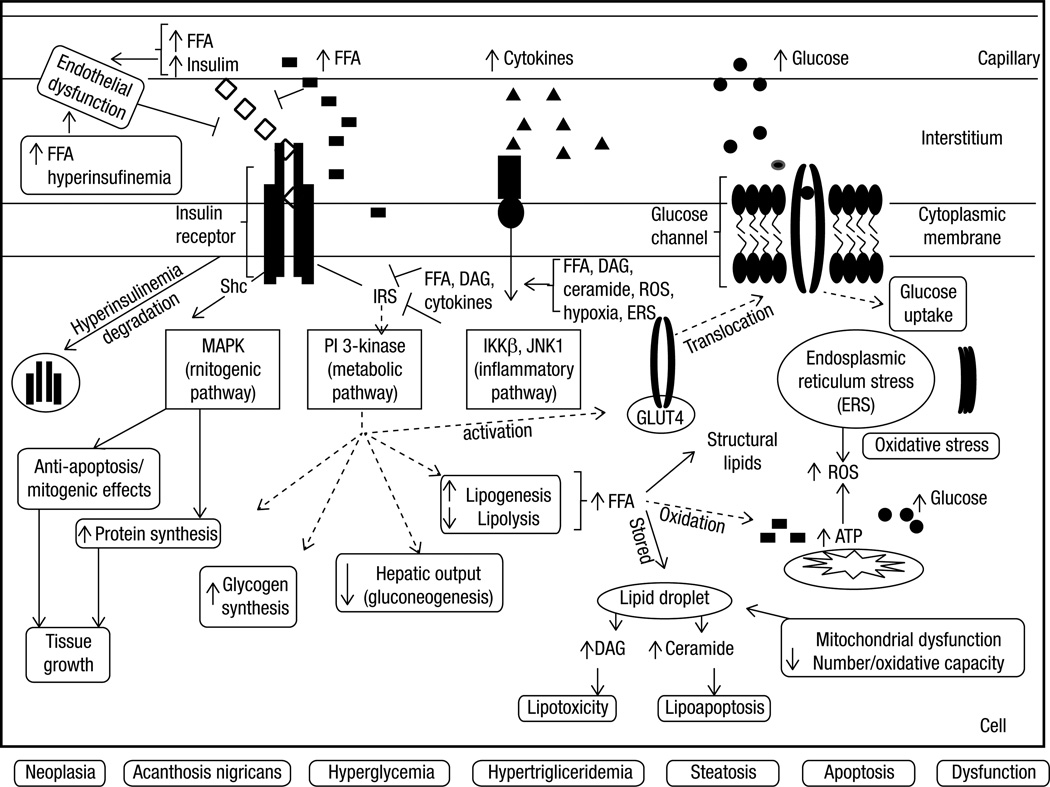
Figure 3. Summary of the main putative molecular mechanisms involved in the development of insulin resistance associated with obesity in a hypothetical cell (e.g. hepatocyte, myocyte, adipocyte).
Insulin resistance associated with obesity, especially central, occurs due to pre-receptor, receptor and/or post-receptor impairments, mainly secondary to elevated FFA, hyperinsulinemia and increased cytokines. Insulin access to the interstitial space (pre-receptor impairment) may be induced by the excess of FFA and their metabolites as well by endothelial dysfunction secondary to increased circulating insulin. Hyperinsulinemia, secondary to the decrease of FFA-induced insulin clearance and the increase of insulin secretion, causes downregulation of insulin receptors (receptor impairment). In addition, insulin receptor downstream signaling (post-receptor impairment) is inhibited by FFA and cytokines. Increased intracellular FFA also contribute to excessive production of ATP, oxidative stress and mitochondrial dysfunction, production of reactive oxidative species, endoplasmic reticulum stress and lipid storage and accumulation of non-oxidative toxic derivatives (dyacylgycerol and ceramide). The aforementioned factors also activate inflammation pathways. Independently of the upstream or downstream level of the insulin receptor impairment, insulin resistance occurs by the inhibition of the phosphorylation of the insulin receptor substrates (IRS-1 or 2) and the subsequent inhibition of PI3K pathway, responsible for metabolic effects. Consequently to this inhibition occurs 1) decrease in the activation of GLUT-4 which impairs glucose uptake; 2) increase of glucose production by the liver (either by inhibiting glucogenesis and/or promoting glycogenolysis) and 3) increase of de novo lipogenesis, storage of lipid (lipid droplets) and toxic derivatives. On the other hand, the insulin receptor substrate, Shc, is spared from inhibition by FFA or cytokines and is stimulated by hyperinsulinemia. Consequently, MAPK pathway (mitogenic) is activated leading to anti-apoptotic and proliferation effects, culminating with tissue growth. Metabolic and non-metabolic consequences of IR and ectopic accumulation of fat are: hyperglycemia, hypertriglyceridemia, acanthosis nigricans, neoplasias, steatosis, cell growth or apoptosis or cell dysfunction.
FFA: free fatty acids; IRS: insulin receptor substrates; MAPK: mitogen-activated protein kinase; PI3K: phosphoinositide 3-kinase; DAG: dyacylgycerol; ROS: reactive oxidative species; ERS: endoplasmic reticulum stress, AN: acanthosis nigricans.