Abstract
Objective
To elucidate etiological factors of heterotopic ossification (HO) by evaluating retrospectively if HO is a unique finding following cervical total disc replacement (CTDR) or a finding observable following an anterior cervical interbody fusion (ACIF).
Methods
The authors had selected 87 patients who underwent anterior cervical surgery (TDR or ACIF), and could be followed up more than 24 months. A cervical TDR was performed using a Bryan disc or a ProDisc-C and an ACIF using a stand-alone cage or fibular allograft with a plate and screws system. The presence of HO was determined by observing plain radiography at the last follow up. The relation between HO occurrence and specific preoperative radio-logical findings (osteophyte and calcification of posterior longitudinal ligament (PLL)) at the index level was investigated.
Results
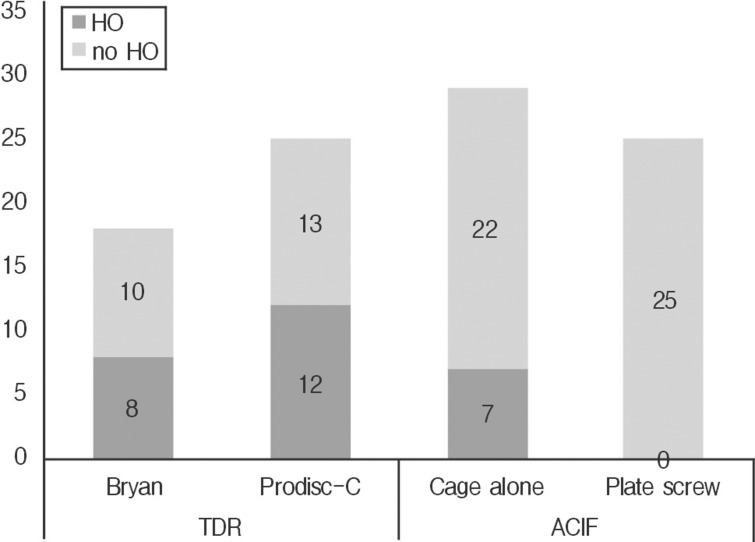
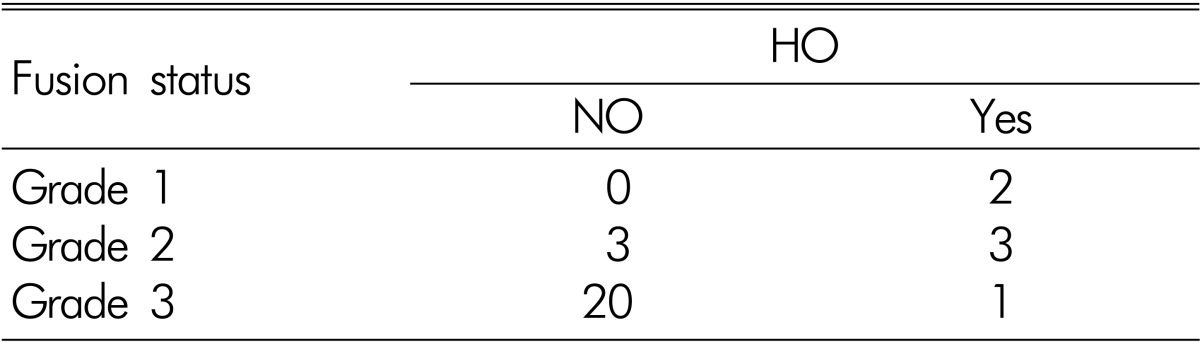
Cervical TDR was performed in 40 patients (43 levels) and ACIF in 47 patients (54 levels). At the final radiographs, HO was demonstrated at 27 levels (TDR-Bryan; 8/18, TDR-Prodisc-C; 12/25, ACIF-cage alone; 7/29, and ACIF-plate screw; 0/25). Mean ROM at the last follow-up of each TDR subgroup were 7.8±4.7° in Bryan, 3.89±1.77° in Prodisc-C, and it did not correlated with the incidence of HO. Fusion status of ACIF groups was observed as 2 case of grade 1, 6 of grade 2, and 21 of grade 3 in cage alone subgroup, and no case of grade 1, 4 of grade 2, and 21 of grade 3 in plate screw subgroup. Fusion status in ACIF-cage alone subgroup was significantly related to the HO incidence. The preoperative osteophyte at the operated level observed in 27 levels, and HO was demonstrated in 12 levels (TDR-Bryan; 3/5, TDR-Prodisc-C; 2/3, ACIF-cage alone; 7/11, and ACIF-plate screw; 0/8). Preoperative PLL calcification at the operated level was observed 22 levels, and HO was defined at 14 levels (TDR-Bryan; 5/5, TDR-Prodisc-C; 4/5, ACIF-cage alone; 5/7, and ACIF-plate screw; 0/5). The evidence of preoperative osteophyte and PLL calcification showed statistically significant relations to the occurrence of HO.
Conclusion
HO was observed in both TDR and ACIF groups. HO was more frequently occurred in TDR group regardless of prosthesis type. In ACIF group, only cage alone subgroup showed HO, with relation to fusion status. Preoperative calcification of longitudinal ligaments and osteophyte were strongly related to the occurrence of HO.
Keywords: Degenerative cervical spine disease, Cervical arthroplasty, Heterotopic ossification, Bryan disc, Prodisc-C, Cervical athrodesis
INTRODUCTION
The definition of heterotopic ossification (HO) is the formation of ectopic bone outside the skeletal system where bone formation does not occur normally. With rising the various kinds of spinal motion preserving surgeries, spinal surgeons are also getting concerned with HO. Mc-Afee et al., firstly described and classified HO following lumbar total disc replacement (TDR)10). According to their report, the incidence of HO after lumbar TDR had ranged from 1.4% to 15.2%. Following cervical TDR, the incidence of HO reported has shown a wide range from 7% to 56%7, 15,19,20,21).
Although the precise causal factors of HO are still unclear, mesenchymal cells originating from bone or muscle to osteoblasts would play a major role12). During the surgery, the manipulations of bone and muscle may provide an opportunity for mesenchymal cells to spread into wellvascularized surrounding soft tissue. Thus, during cervical TDR, trauma to the longus colli and the remaining bone debris following bone works may predispose inevitable ectopic bone formation. However, if this hypothesis is applicable, there would be a same risk of HO occurrence in other kinds of anterior cervical surgeries. All anterior cervical surgeries with standard approach require similar manipulation of soft tissues and bone work, thus they has a same possibility to be caught in the HO.
This retrospective study is performed to observe the incidence of HO in different kinds of anterior cervical surgeries; TDR and anterior cervical interbody fusion using stand-alone cage or fibular allograft with a plate and screws system, and to identify etiological factors of HO in relation to the clinical and radiological findings.
MATERIALS AND METHODS
1. Patients
For the present study, the authors had gathered the records of 108 patients who underwent anterior cervical surgery for degenerative cervical spine diseases between April 2004 and October 2007. Among them, 87 patients could be followed up more than 24 months were enrolled. Other 21 patients were lost during follow-up by several reasons such as changing contact addresses, death, or pregnancy.
The surgeries consisted with cervical TDR using Bryan disc (Medtronic Sofamor Danek) or Prodisc-C(Synthes Spine) and anterior cervical interbody fusion (ACIF) using a RABEA (Signus Medical) stand-alone cage or fibular allograft with a plate and screws using Atlantis system(Medtronic Sofamor Danek). All operations were performed by a single senior surgeon (C.K.P.). According to each surgical procedure, the enrolled patients were classified into 4 groups; 'TDR-Bryan', 'TDR-Prodisc-C', 'ACIF-cage alone', and 'ACIF-plate screws group'. The cases of hybrid surgery which combined with TDR and arthrodesis were excluded in the present study.
2. Assessment
All radiological assessments were performed by observing plain cervical radiography. Images obtained at the preoperative were compared with those of the last follow up.
Flexion-extension segmental range of motion (ROM) was measured at all affected levels. ROM was determined from differences between flexion and extension angles. This measurement was performed on digital radiograph images displayed on a PACS (Picture Achieve and Communication System) terminal (Marosis 2003, Marotech, Seoul), and angles were measured using a program in PACS. In ACIF groups, the degree of bone fusion state was classified from grade 1 to 3, based on the findings of dynamic lateral X-ray (Table 1).
Table 1. The degree of fusion state based on dynamic X-ray of each arthrodesis method.

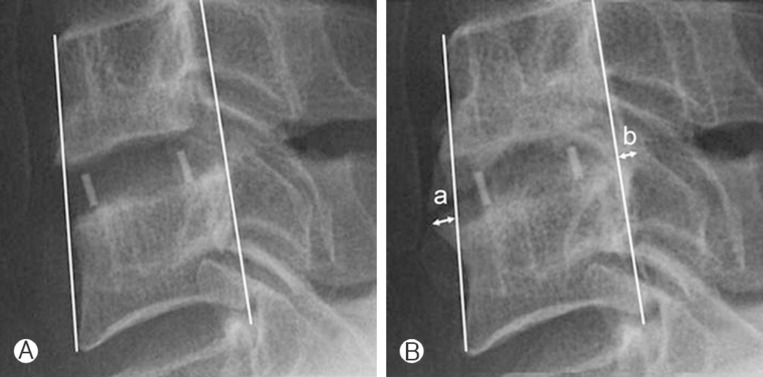
Other specific radiological findings at the preoperative images including posterior longitudinal ligament (PLL) calcification or osteophyte at the operated level were also evaluated. The presence of HO was determined and classified using McAfee classification system10) in TDR groups. In ACIF groups, if there was more than 1mm of any bone formation from the outmost border of vertebral body at last follow-up AP or lateral plain X-ray comparing to immediate postoperative images, this bone formation was determined as HO(Fig. 1).
Fig. 1. Plain lateral radiographs showing how HO in ACIF group is determined in the lateral plane. If there is more than 1mm of bone formation (width of 'a' or 'b') from the anterior or posterior outmost border of vertebral body on the last follow-up image (B) comparing to immediate post-operative one (A), this bone formation is defined as HO.
The radiological assessments were performed twice by 2 independent observers. Inter- and intraobserver reliabilities of all radiological data were greater than a correlation of 0.80.
3. Statistics
Comparing occurrence rate of HO between the subgroups was done using t-test. The presence of HO was statistically was verified in relation to the parameters of the present study. The relation to segmental ROM in TDR groups and fusion grade in ACIF groups was evaluated using a Spearman's rank correlation coefficient. The correlation with the presence of preoperative specific radiological findings was assessed using Chi-square test. Numerical results were averaged. All numerical findings were expressed as means ±SDs. Statistical verification was determined using PASW Statistics 18 (version 18.0.0; SPSS Inc., USA). A P-value at 0.05 was set as statistical significance
RESULTS
Cervical TDR was performed in 40 patients, and ACIF was done in 47 patients. There were 10 cases of two level surgeries, thus total levels operated was 97. The demographic data of the patients of each subgroup were listed on Table 1.
Mean ROMs at the last follow-up of each TDR subgroup were 7.8±4.7° in Bryan, 3.89±1.77° in Prodisc-C. Fusion status of ACIF groups was observed as 2 case of grade 1, 6 of grade 2, and 21 of grade 3 in cage alone subgroup (grade 1; 6.9%, grade 2; 20.7%, and grade 3; 72.4%) and no case of grade 1, 4 of grade 2, and 21 of grade 3 in plate screw subgroup (grade 2; 16.0%, and grade 3; 84.0%).
Among total 97 levels operated, HO was demonstrated at 27 levels. The occurrence of HO in each group was showed on Fig. 2. TDR-Bryan group showed 44.4% of HO occurrence and TDR-Prodisc-C group did 48.0%, and there was no significant difference between two subgroups (p>0.05). In ACIF group, ACIF-cage alone subgroup only presented 24.1% of HO. There was no case presented HO in plate screw subgroup.
Fig. 2. Bar graphs showing the occurrence of HO in each group.
The preoperative osteophyte at the operated level observed in 27 levels (TDR-Bryan; 5, TDR-Prodisc-C; 3, ACIF-cage alone; 11, ACIF-plate screw; 8). Among those 27 levels, HO was demonstrated in 14 levels (TDR-Bryan; 3 (60.0%), TDR-Prodisc-C; 2 (66.7%), ACIF-cage alone; 7 (63.6%), ACIF-plate screw; 0).
Preoperative PLL calcification at the operated level was observed 22 levels (TDR-Bryan; 5, TDR-Prodisc-C; 5, ACIF-cage alone; 7, ACIF-plate screw; 5). HO was defined at 9 levels in TDR group (TDR-Bryan; 5 (100%), TDR-Prodisc-C; 4 (90 %), and 5 levels in ACIF group ACIF-cage alone; 5 (71.4%), ACIF-plate screw; 0).
The statistical verification between clinical variables of the present study and the occurrence of HO was listed on Table 3. The grade of fusion status, the evidence of preoperative osteophyte and PLL calcification were significantly related to the occurrence of HO. The final ROMs at the operated segment in TDR group did not correlate with the occurrence of HO. HO occurrence in relation to fusion status in ACIF-cage alone subgroup was listed on Table 4.
Table 3. Relations between clinical variables and heterotopic ossification.

Table 4. HO occurrence in relation to fusion status in ACIF-cage alone subgroup.
DISCUSSION
In cervical TDR, HO has been considered as one of the major problems. Although the clinical significance of HO is not proved, it should diminish the motion at the index segment over time.
The precise etiology of HO is still unclear, but traumatic, neurogenic, and genetic factors are considered as major possible causes2,11). Among them, traumatic HO would follow fractures, severe burns, or operation procedures, and it is conceived that the differentiation of mesenchymal cells originating from skeletal system to osteoblasts plays a major role12). Mesenchymal cells releasing form the damaged muscle or bone may spread into surrounding soft tissue, evolve into osteoblast by stimulation of bone inducing agents such as BMP (bone morphogenetic protein)3,5,13) or prostaglandin-E21,9,18), and finally lead inevitable bone formation.
HO following cervical TDR has been considered to occur by traumatic cause. Thus, several intraoperative situations, such as bleeding at the keel cut site, rough soft-tissue dissection, and the remained bone dust following bone works are proposed as possible causal factors15,21). However, these are not unique circumstances of cervical TDR only. All anterior cervical surgeries with standard approach require manipulation of soft tissues and bone to various degree. If we accepted the proposed pathogenesis of traumatic HO, there would be a possibility of that HO could occur after all kinds of anterior cervical spine surgeries.
In the present study, TDR group showed high incidence rate of HO in two subgroups (Bryan: 44%, Prodisc-C: 48%). ACIF group which was operated with a stand-alone cage also showed 24.1% of HO occurrence rate, despite of no case presented HO in plate screw subgroup. Although the incidence is different, the present results indicate that HO is not a special event of TDR surgery. The occurrence rate of HO between two TDR subgroups is similar, but between the ACIF subgroups, there was a significant difference. An ACIF with standalone cage is a little simpler procedure than an ACIF with plate and screw fixation. Thus, the incidence of HO in cage alone group should be lower than plate screw subgroup according to the hypothesis of traumatic HO. However, the present study showed the opposite results which cage alone subgroup presented higher incidence.
In ACIF, it could be a debated issue whether the bone formation from the outmost border of vertebral body at the operated level is real HO or not. It could be concerned as one of fusion processes or a finding related to pseudoarthrosis. However, a typical fusion process in ACIF using an interbody cage would be more conducted inside of a cage rather than near the outmost vertebral body. In the present study, most of the case in ACIF group which was determined as HO showed the obvious bone formation in near outmost vertebral body than inside a cage. Pseudoathrosis means fusion failure. The remaining motion due to failed fusion could make a similar situation with an unsuccessful motion preserving surgery. Thus, we believe that bone formation near outmost vertebral body is real HO.
Many clinicians have emphasized that prevention of HO strongly depend on the degree of manipulation of soft tissue or bone during the procedure. Intraoperatively, therefore, careful dissection of soft-tissue, and meticulous hemostasis and cleaning operation field after bone works have been recommended to decrease incidence rate of HO. Yang et al.21), reported only 6.7% of HO occurrence rate after cervical TDR with Bryan disc at a minimum of 24 months follow-up. They described that their best attempt at cleaning the operative site with normal saline and limiting retraction of cervical muscles would be effective in prevention of HO. However, practically most spine surgeons routinely have tried to minimize soft tissue injury and clean the field during the operation. And there have been much more reports to note the high incidence of HO following cervical TDR. Thus, we believe that there could be other factors affecting the occurrence rate of HO except for manipulation degree of soft tissue or bone.
The biomechanical studies in the cervical spine have revealed that fixations with stand-alone cage provide less stiffness than the plated method. Shimamoto et al.16), performed in vitro biomechanical investigation of the immediate stability in cervical reconstruction. They compared three different reconstruction methods; stand-alone cage (RABEA cage), tricortical autograft only, and additional locking plate and screws system by observing three-dimensional segmental range of motion at the operated segment. In flexion/extension, standalone cage group showed a significantly higher range of motion than did the other groups, and even than did intact spine. Hart et al.6), have conducted in vitro biomechanical comparison of a single threaded cylindrical interbody cage versus a plated fusion construct. They also observed that the specimens implanted with a cage showed significantly greater initial ROM and significantly less initial stiffness than in plated specimens. Cage specimens also failed at a significantly lower load than plated specimens. This low biomechanical property of standalone cage would affect fusion success rate. In the present study, cage alone subgroup showed low fusion rate (grade 1; 6.9%, grade 2; 20.7%, and grade 3; 72.4%) compared to plate screw subgroup (grade 2; 16.0%, and grade 3; 84.0%). Song et al.17), reported similar results with the present study. In their study, ACIF performed with plate and screw fixation had better fusion rate and faster fusion time than ACIF with stand-alone cage. These above results mean that a fixation with standalone cage has more remaining motion postoperative immediately and over time compared to the plate screw group.
Following the present results, it seems that there is the remained motion after surgery, HO could occur. It could be supposed that a biomechanical stress related to motion is strongly related to developing HO. It has been well known that repetitive dynamic loads on bone may trigger bone remodeling. Thus, we suggested that a mechanical stimulation by constant dynamic load from the postoperative remaining motion regardless type of surgery is one of causal factors of HO. In the present study, the final ROMs at the operated segment in TDR subgroups was significantly different according to prosthesis type. However, both TDR subgroups showed the similar incidence of HO. It suggested that occurrence rate of HO depends on whether the motion is remaining or not, not proportional the amount of motion remained.
Moreover, HO would be a normal defense mechanism of human body against non-physiologic motion. In physiologic situation, unacceptable motion of skeletal system could be eliminated by surrounding bone formation. If this hypothesis is received, the high incidence of HO in the most artificial discs popularly used indicates that the prostheses do not provide physiologic motion as like as normal disc. If prosthesis does not function as much as normal disc does, HO could be remained as an unavoidable problem, regardless of how much handles soft tissue or bone during an operation. In such case, prosthesis which provides normal physiologic motion would be only solution to prevent HO.
Preoperative osteophyte and PLL calcifications have been regar ded as a risk factor of HO4,14,15). We also studied whether these preoperative constitutional factors affect postoperative occurrence of HO. In the present results, preoperative osteophyte and PLL calcifications were strongly correlated with postoperative development of HO.
Preserving motion is the most important goal of TDR surgery. Thus, occurrence of HO has been seriously emphasized because of its relationship with loss of motion. Leung et al.8), reported a strong association between the occurrence of HO and the loss of mobility of the operated segment of cervical TDR which is fatal to the effectiveness of TDR. To develop ideal prosthesis which could maintains motion in a long term, more effort to understand normal kinematics of disc would be needed.
CONCLUSION
In the present study, HO was observed in both TDR groups, and there was no difference of occurrence rate between two prosthesis types. In ACIF group, cage alone subgroup showed higher incidence of HO than the rigidly fixed plate screw subgroup. The results herald that not only iatrogenic factor such as postoperative biomechanical stress but constitutional properties such as preoperative calcification of longitudinal ligaments and osteophyte also play important role in the process of HO formation.
Table 2. Demographic date of the patients.
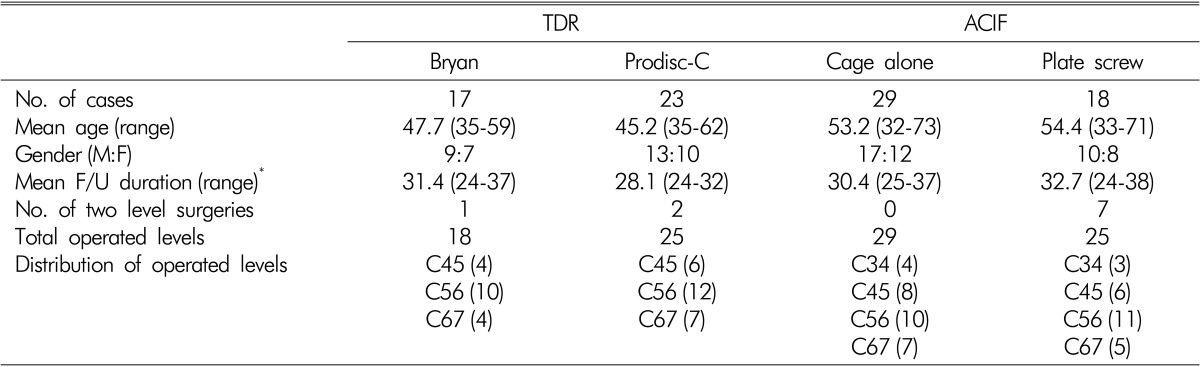
*Months
References
- 1.Ahrengart L, Lindgren U, Reinholt FP. Comparative study of the effects of radiation, indomethacin, prednisolone, and ethane-1-hydroxy-1, 1-diphosphonate (EHDP) in the prevention of ectopic bone formation. Clin Orthop Relat Res. 1988:265–273. [PubMed] [Google Scholar]
- 2.Balboni TA, Gobezie R, Mamon HJ. Heterotopic ossification: Pathophysiology, clinical features, and the role of radiotherapy for prophylaxis. Int J Radiat Oncol Biol Phys. 2006;65:1289–1299. doi: 10.1016/j.ijrobp.2006.03.053. [DOI] [PubMed] [Google Scholar]
- 3.Brooker AF, Bowerman JW, Robinson RA, Riley LH., Jr Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629–1632. [PubMed] [Google Scholar]
- 4.Eggli S, Woo A. Risk factors for heterotopic ossification in total hip arthroplasty. Arch Orthop Trauma Surg. 2001;121:531–535. doi: 10.1007/s004020100287. [DOI] [PubMed] [Google Scholar]
- 5.Hannallah D, Peng H, Young B, Usas A, Gearhart B, Huard J. Retroviral delivery of Noggin inhibits the formation of heterotopic ossification induced by BMP-4, demineralized bone matrix, and trauma in an animal model. J Bone Joint Surg Am. 2004;86-A:80–91. doi: 10.2106/00004623-200401000-00013. [DOI] [PubMed] [Google Scholar]
- 6.Hart R, Gillard J, Prem S, Shea M, Kitchel S. Comparison of stiffness and failure load of two cervical spine fixation techniques in an in vitro human model. J Spinal Disord Tech. 2005;18(Suppl):S115–S118. doi: 10.1097/01.bsd.0000132288.65702.6e. [DOI] [PubMed] [Google Scholar]
- 7.Hrabalek L, Vaverka M, Houdek M. [Cervical disc arthroplasty (Prodisc-C): analysis of 3 to 4-year follow up results] Rozhl Chir. 2009;88:634–641. [PubMed] [Google Scholar]
- 8.Leung C, Casey AT, Goffin J, Kehr P, Liebig K, Lind B, et al. Clinical significance of heterotopic ossification in cervical disc replacement: a prospective multicenter clinical trial. Neurosurgery. 2005;57:759–763. doi: 10.1093/neurosurgery/57.4.759. discussion 759-763. [DOI] [PubMed] [Google Scholar]
- 9.Matta JM, Siebenrock KA. Does indomethacin reduce heterotopic bone formation after operations for acetabular fractures? A prospective randomised study. J Bone Joint Surg Br. 1997;79:959–963. doi: 10.1302/0301-620x.79b6.6889. [DOI] [PubMed] [Google Scholar]
- 10.McAfee PC, Cunningham BW, Devine J, Williams E, Yu-Yahiro J. Classification of heterotopic ossification (HO) in artificial disk replacement. J Spinal Disord Tech. 2003;16:384–389. doi: 10.1097/00024720-200308000-00010. [DOI] [PubMed] [Google Scholar]
- 11.McCarthy EF, Sundaram M. Heterotopic ossification: a review. Skeletal Radiol. 2005;34:609–619. doi: 10.1007/s00256-005-0958-z. [DOI] [PubMed] [Google Scholar]
- 12.Naraghi FF, DeCoster TA, Moneim MS, Miller RA, Rivero D. Heterotopic ossification. Orthopedics. 1996;19:145–151. doi: 10.3928/0147-7447-19960201-10. [DOI] [PubMed] [Google Scholar]
- 13.Reddi AH. Bone morphogenetic proteins, bone marrow stromal cells, and mesenchymal stem cells. Maureen Owen revisited. Clin Orthop Relat Res. 1995:115–119. [PubMed] [Google Scholar]
- 14.Ritter MA, Vaughan RB. Ectopic ossification after total hip arthroplasty. Predisposing factors, frequency, and effect on results. J Bone Joint Surg Am. 1977;59:345–351. [PubMed] [Google Scholar]
- 15.Ryu KS, Park CK, Jun SC, Huh HY. Radiological changes of the operated and adjacent segments following cervical arthroplasty after a minimum 24-month follow-up: comparison between the Bryan and Prodisc-C devices. J Neurosurg Spine. 2010;13:299–307. doi: 10.3171/2010.3.SPINE09445. [DOI] [PubMed] [Google Scholar]
- 16.Shimamoto N, Cunningham BW, Dmitriev AE, Minami A, McAfee PC. Biomechanical evaluation of stand-alone interbody fusion cages in the cervical spine. Spine (Phila Pa 1976) 2001;26:E432–E436. doi: 10.1097/00007632-200110010-00008. [DOI] [PubMed] [Google Scholar]
- 17.Song KJ, Taghavi CE, Lee KB, Song JH, Eun JP. The efficacy of plate construct augmentation versus cage alone in anterior cervical fusion. Spine (Phila Pa 1976) 2009;34:2886–2892. doi: 10.1097/BRS.0b013e3181b64f2c. [DOI] [PubMed] [Google Scholar]
- 18.Spencer RF. The effect of head injury on fracture healing. A quantitative assessment. J Bone Joint Surg Br. 1987;69:525–528. doi: 10.1302/0301-620X.69B4.3611151. [DOI] [PubMed] [Google Scholar]
- 19.Tortolani PJ, Cunningham BW, Eng M, McAfee PC, Holsapple GA, Adams KA. Prevalence of heterotopic ossification following total disc replacement. A prospective, randomized study of two hundred and seventy-six patients. J Bone Joint Surg Am. 2007;89:82–88. doi: 10.2106/JBJS.F.00432. [DOI] [PubMed] [Google Scholar]
- 20.Walraevens J, Demaerel P, Suetens P, Van Calenbergh F, van Loon J, Vander Sloten J, et al. Longitudinal prospective long-term radiographic follow-up after treatment of single-level cervical disk disease with the Bryan Cervical Disc. Neurosurgery. 2010;67:679–687. doi: 10.1227/01.NEU.0000377039.89725.F3. discussion 687. [DOI] [PubMed] [Google Scholar]
- 21.Yang YC, Nie L, Cheng L, Hou Y. Clinical and radiographic reports following cervical arthroplasty: a 24-month follow-up. Int Orthop. 2009;33:1037–1042. doi: 10.1007/s00264-008-0571-6. [DOI] [PMC free article] [PubMed] [Google Scholar]