Abstract
Hydatid disease of the bone is a very rare manifestation of the disease, and is often associated with debilitating symptoms. We present a rare case of skeletal hydatidosis in a 56-year-old man who had been misdiagnosed for many years. Massive involvement of the pelvic bones and soft tissues was evident. An extended hemipelvectomy was performed in order to achieve resection of the affected segments with a clear surgical margin. The patient recovered uneventfully and there are no signs of recurrence of the disease.
Background
The case is very illustrative and has high educational value. First, it highlights a very rare manifestation of a disease, and demonstrates that diagnosis of certain infectious diseases can be missed or delayed in non-endemic regions. This is, to our opinion, a very important challenge for physicians in Western countries who have to face a steadily increasing number of patients from other parts of the world. Diagnostic challenges and errors are clearly depicted in our case. Furthermore, it shows that errors in decision-making during treatment and delays in referral of the patient to a specialised centre can have serious adverse effects. Finally, it presents a novel surgical treatment for this neglected form of the disease.
Case presentation
A 56-year-old man from Turkey, who had been living in Sweden for many years, was referred to our centre because of intractable pain in the pelvis and left hip. The patient had no associated comorbidities apart from being cachectic and confined to a wheel-chair. He had been treated since the middle 1980s for a suspected tuberculosis infection of the left hip, although the diagnosis had not been verified by culture or PCR. Plain X-ray revealed cystic lesions in the pelvis, and deformation of the acetabulum and the hip. The patient had total hip replacement with a conventional cemented arthroplasty in 2004. Biopsies and cultures were taken during the operation, and were negative for active tuberculosis. The patient thus discontinued tuberculostatic treatment. No significant improvement was noted after the operation, and the diagnosis of echinococcosis was set based on radiographic findings collected when the patient sought a medical facility in an endemic country. On his return to Sweden, the diagnosis was verified with serological tests (Western blot and ELISA) as well as during a review of the pathology reports. The patient began antiparasitic therapy (albendazole and praziquantel). Owing to progressive symptoms from the left hip and superimposed infection of the prosthesis, he underwent removal of the components and excision arthroplasty in 2007. Later the same year, soft-tissue revision was carried out because of extensive fistula formation. No parasites could be detected in the biopsies. The patient was offered a hemipelvectomy due to severe pain, but he refused it. He subsequently developed chronic fistulas for which he sought medical help several times, and minor revisions were carried out.
Investigations
The actual CT scans were revised and showed an extensive infiltration of the retroperitoneal space reaching the left kidney. The whole left hemipelvis and almost half of the sacrum were involved. In the thigh, the cysts almost reached the knee and there was a pathological fracture of the femur (figure 1).
Figure 1.

CT scan of the patient showing the extensive invasion of the pelvis, retroperitoneal tissue and proximal femur, by the parasite. Multilocular cyst formation is observed, reaching to the lower kidney pole (open arrow) along with a pathological fracture of the proximal femur (solid arrow).
Differential diagnosis
The differential diagnosis in this occasion is tuberculosis. In similar settings, where cystic lesions of the soft tissues and skeletal involvement occur, the physician has to rule out bacterial infections (osteomyelitis and abscesses) as well as necrotic tumours that erode the bone.
Treatment
An extended hemipelvectomy was performed, whereupon the colon, spleen, urinary bladder and the left kidney had to be mobilised in order to allow en bloc resection of the specimen (figure 2). Dissection through the lateral part of the second to fifth lumbar vertebrae was performed to ensure a clear surgical margin. The large defect was reconstructed using a musculocutaneous flap from the gluteal site. A superficial infection of the surgical site was successfully treated with antibiotics and drainage of the area. The pathology report revealed no viable parasites.
Figure 2.
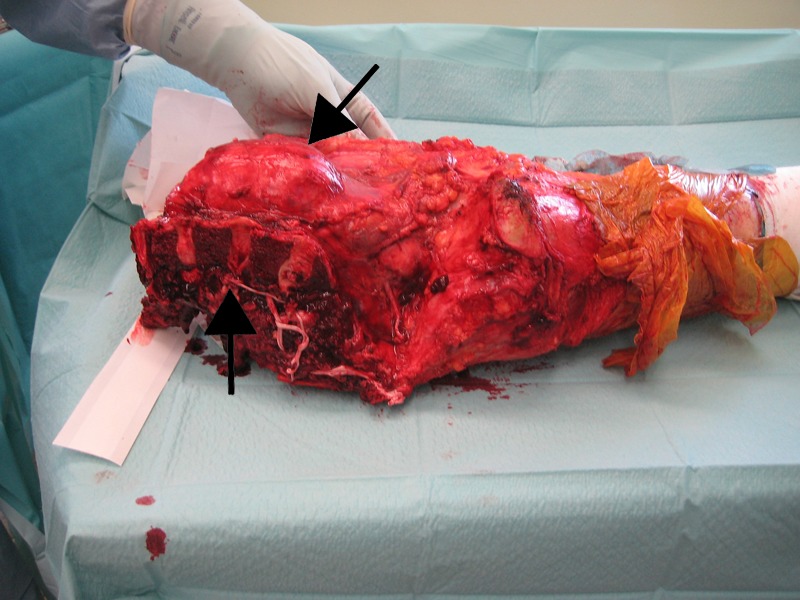
Peroperative photograph of the specimen showing the osteotomy through the lower lumbar vertebrae (open arrow). A cyst protruding in the retroperitoneal space is also obvious (solid arrow).
Outcome and follow-up
The recovery of the patient was uneventful. A year after the operation, the patient developed a secondary Staphylococcus aureus infection of the surgical site, localised in the paravertebral area, and required prolonged treatment with antibiotics. He recovered and is currently confined to a wheel chair, but has only intermittent pain. There are no signs of recurrence of the disease.
Discussion
Although rare, bone hydatidosis is a debilitating disease, often presenting with severe pain, functional impairment and pathological fractures.1 2 The progression of the lesions is slow and the initiation of symptoms can be delayed for many years, typically presenting in adulthood. In regions where disease prevalence is low, correct diagnosis can be delayed for years and this can have serious implications for the patient, as our case clearly demonstrates. Chronic infections of the bone, such as tuberculosis, as well as benign and malignant tumours, are considered in the differential diagnosis. Patients can be misdiagnosed even in endemic regions.3 Clearly, in Western countries where clinical suspicion is very low, this risk is even higher, especially taking into consideration the increasing immigration from endemic areas. Several immunological diagnostic tests have low sensitivity in extrahepatic hydatidosis. Radiology is helpful to set diagnosis, and CT has been suggested as the most appropriate imaging modality for bone lesions. Serology also gives valuable clues, but biopsy remains the cornerstone for diagnosis.
It appears that the parasite has a predilection for the vertebrae, pelvis and proximal femur, where it often forms multicystic lesions. Histologically, these lesions differ from visceral cysts, as they lack a fibrous capsule. Instead, they are characterised by osteolytic destruction of the bone.1 To our knowledge, cysts of this magnitude are extremely rare.4 5 In their review of bone echinococcosis where 721 cases were included, Steinmetz et al2 report that lesions range between 1 and 20 cm, with a median diameter of 5.5 cm.
Treatment is mainly surgical, with an aim to have a clear surgical margin in order to avoid recurrence of the disease, as is followed in many cases of oncological surgery for malignant tumours. There is a consensus that intralesional procedures imply a very high risk for local recurrence.6 However, most patients refuse amputation and are subject to less radical surgery, such as debridement, which is often combined with the use of local adjuvants such as hypertonic saline, formalin, phenol and polymethylmethacrylate.2 7 Osteosynthesis of pathological fractures and reconstruction with prosthesis has been described, when limb-sparing surgery is chosen.2 3 8 Collectively, amputation has been used in less than 1% of bone hydatidosis, mainly because the majority of patients present with limited disease. Hemipelvectomy has also been reported in the management of extensive pelvic involvement.9 This is, to the best of our knowledge, the first case of extended hemipelvectomy comprising of partial resection of the lower lumbar vertebrae due to the massive infiltration of the pelvic girdle and retroperitoneal space by giant parasite cysts.
Medical therapy is often used as an adjunct to surgery, given preoperatively as well as for a sufficient time after the operation, but is generally considered to have a secondary role in treatment. Therapeutic recommendations have not been established for bone echinococcosis, whereas there are international guidelines for visceral hydatid disease.10 11 Albendazole has been suggested as the drug of choice due to the high plasma levels. This class of drug is also well tolerated, even when administration is prolonged for many years.7
Taking into account the fact that late remissions can occur, we recognise that our case report has a short follow-up time.12 However, in a meta-analysis of all published cases of bone echinococcosis, the only variable associated with local recurrence was distant organ involvement, which was absent in our patient.2 Similarly, the remission rates that have been described are very much like the ones reported for bacterial osteomyelitis, corroborating the evidence for parasite eradication.
In conclusion, we report a rare case of massive pelvic girdle hydatidosis with involvement of the femur and retroperitoneal space that was managed successfully with an extended hemipelvectomy. The case illustrates also the diagnostic dilemmas and pitfalls encountered, especially in areas where the disease is not endemic, and stresses the need for radical surgery in order to achieve eradication of the parasite.
Learning points.
Think in terms of endemic diseases at the region of origin when treating patients.
Consult appropriate medical providers when confronting a diagnostic or treatment dilemma, in order to avoid delays in diagnosis or erroneous therapy, which in turn can have serious consequences for the patient.
Skeletal echinococcosis is extremely rare and very difficult to treat. Radical resection of the lesions should be the goal even in cases of extensive bone and soft-tissue involvement.
Footnotes
Contributors: PT was responsible for data collection and preparation of the manuscript. OB reviewed the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Bracanovic D, Djuric M, Sopta J et al. Skeletal manifestations of hydatid disease in Serbia: demographic distribution, site involvement, radiological findings, and complications. Korean J Parasitol 2013;51:453–9. 10.3347/kjp.2013.51.4.453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Steinmetz S, Racloz G, Stern R et al. Treatment challenges associated with bone echinococcosis. J Antimicrob Chemother 2014;69:821–6. 10.1093/jac/dkt429 [DOI] [PubMed] [Google Scholar]
- 3.Liang Q, Wen H, Yunus A et al. Treatment experiences of pelvic bone hydatidosis. Int J Infect Dis 2014;18:57–61. 10.1016/j.ijid.2013.09.010 [DOI] [PubMed] [Google Scholar]
- 4.Kapoor SK, Kataria H, Patra SR et al. Multi-organ hydatidosis with extensive involvement of the hemi-pelvis and ipsilateral femur. Parasitol Int 2013;62:82–5. 10.1016/j.parint.2012.08.006 [DOI] [PubMed] [Google Scholar]
- 5.Siwach R, Singh R, Kadian VK et al. Extensive hydatidosis of the femur and pelvis with pathological fracture: a case report. Int J Infect Dis 2009;13:e480–2. 10.1016/j.ijid.2008.12.017 [DOI] [PubMed] [Google Scholar]
- 6.Papanikolaou A. Osseous hydatid disease. Trans R Soc Trop Med Hyg 2008;102:233–8. 10.1016/j.trstmh.2007.09.012 [DOI] [PubMed] [Google Scholar]
- 7.Brunetti E, Junghanss T. Update on cystic hydatid disease. Curr Opin Infect Dis 2009;22:497–502. 10.1097/QCO.0b013e328330331c [DOI] [PubMed] [Google Scholar]
- 8.Wirbel RJ, Schulte M, Maier B et al. Megaprosthetic replacement of the pelvis: function in 17 cases. Acta Orthop Scand 1999;70:348–52. 10.3109/17453679908997823 [DOI] [PubMed] [Google Scholar]
- 9.De Cristofaro R, Ruggieri P, Biagini R et al. Case report 629: Osseous hydatidosis. Skeletal Radiol 1990;19:461–4. 10.1007/BF00241807 [DOI] [PubMed] [Google Scholar]
- 10.Kern P. Medical treatment of echinococcosis under the guidance of Good Clinical Practice (GCP/ICH). Parasitol Int 2006;55(Suppl):S273–82. 10.1016/j.parint.2005.11.040 [DOI] [PubMed] [Google Scholar]
- 11.[No authors listed] Guidelines for treatment of cystic and alveolar echinococcosis in humans. WHO Informal Working Group on Echinococcosis. Bull World Health Organ 1996;74:231–42. [PMC free article] [PubMed] [Google Scholar]
- 12.Pelegri C, Gaertner E, Bernard E et al. Recurrence of femoral echinococcosis 5 years after a primary surgical procedure. Orthop Traumatol Surg Res 2010;96:94–6. 10.1016/j.otsr.2009.10.014 [DOI] [PubMed] [Google Scholar]


