Abstract
We present an unusual case of a 32-year-old man with haemophilia A, who sustained massive, haemodynamically significant intra-abdominal bleeding from a perforated gallbladder wall and from the greater omentum as a complication of acute ulcerophlegmonous and haemorrhagic cholecystitis. Recombinant coagulation factor VIII was given and an emergency laparotomy was performed, with open cholecystectomy and haemostasis. Coagulation factor VIII was given for a further 2 weeks postoperatively, and the patient was discharged in good condition. In most published cases of haemorrhagic cholecystitis, the haemoperitoneum arises via transhepatic perforation; in this case, there was a free rupture into the peritoneal cavity. Patients with coagulopathies may have severe haemorrhagic complications and therefore need interdisciplinary management before, during and after surgery. Replacement therapy with factor concentrates should be initiated at once, and early surgery for gallbladder disease should be considered.
Background
Gallbladder perforation occurs in 2–15% of cases of acute cholecystitis1 2 and carries a mortality rate of up to 42%.1 Ideally, the diagnosis should be made early and the surgical treatment should follow at once, but preoperative diagnosis is difficult.1 Intra-abdominal bleeding due to gallbladder perforation is rare and has been reported in no more than a few case reports. Bleeding in such cases is reported to arise from transhepatic perforation and avulsion of the gallbladder, with ensuing bleeding from the liver bed.3 4
We present the case of a man with severe haemophilia A, who sustained massive, haemodynamically relevant intra-abdominal bleeding from a perforation of the gallbladder wall due to acute cholecystitis, with free rupture into the peritoneal cavity.
Case presentation
A 32-year-old man with severe haemophilia A (coagulation factor VIII <1%) was admitted to the emergency room with progressively severe colicky abdominal pain in the right upper quadrant of 9 days’ duration. In the 48 h prior to admission, the pain had begun to spread into his back and the rest of the abdomen. He had vomited once. He had no other symptoms. Oral antibiotic treatment had already been started 5 days earlier by his general practitioner.
Investigations
The clinical examination revealed evidence of peritoneal irritation in the upper right quadrant and a positive Murphy's sign.
The relevant laboratory findings included: C reactive protein 131 mg/L, leucocyte count 19×109/L, aspartate aminotransferase 108 U/L, alanine transaminase 98 U/L, total bilirubin 30 µmol/L, alkaline phosphatase 95 U/L, γ-glutamyl transpeptidase 75 U/L and haemoglobin 114 g/L.
Abdominal ultrasonography revealed hydrops of the gallbladder with a large amount of sludge and a thickened gallbladder wall, consistent with acute cholecystitis.
Treatment
We continued therapy with intravenous antibiotics and planned laparoscopic cholecystectomy for the next morning, when the necessary staff and all other resources would be available. In view of the high risk of intraoperative bleeding, the team consciously prepared for early, immediate and, if necessary, pre-emptive conversion to an open cholecystectomy.
A few hours after admission, the patient developed signs of hypovolaemia, with hypotension, tachycardia, pallor and nausea. His abdomen was more tender and his haemoglobin level was now 114 g/L. An emergency CT scan revealed massive haemorrhage throughout the peritoneal cavity with a jet of contrast agent in the area of the gallbladder (figure 1).
Figure 1.
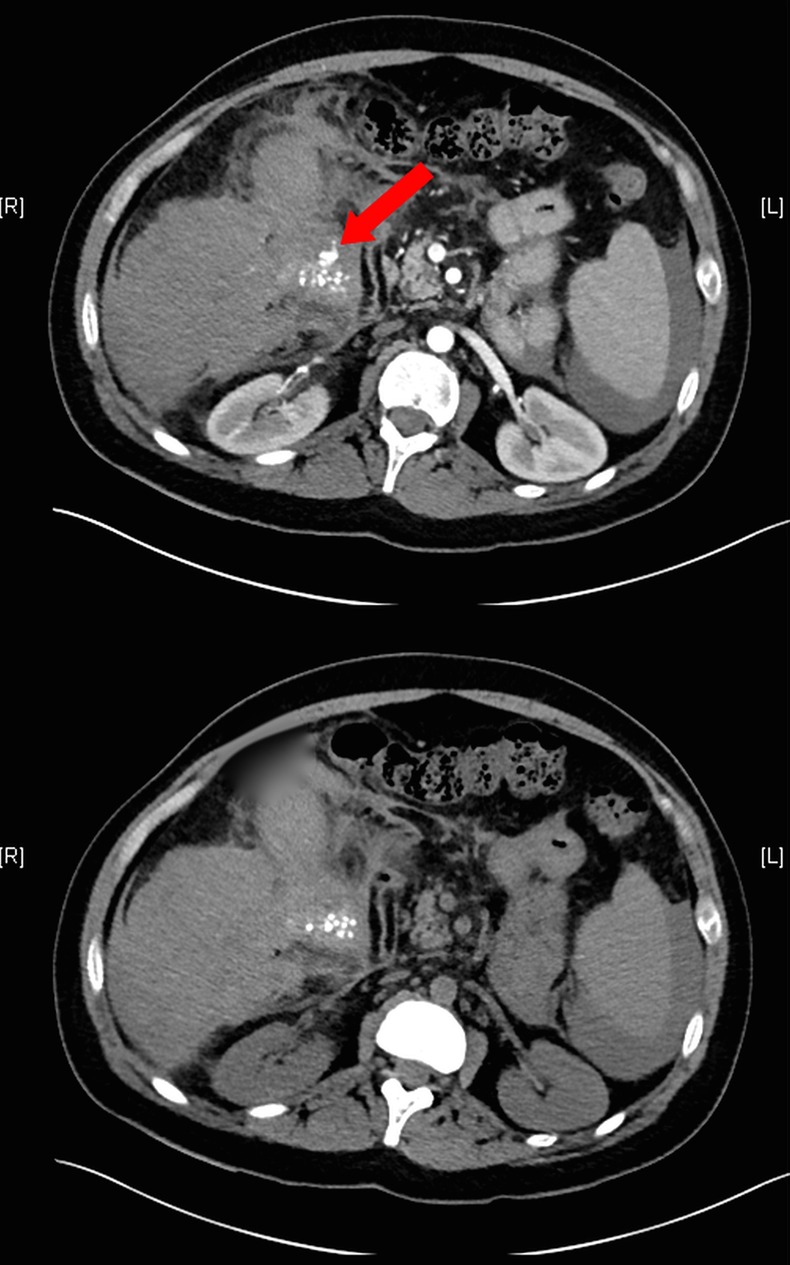
The upper figure with contrast agent shows a contrast jet (arrow), compared to the lower one without contrast agent.
Arterial embolisation was considered. Although an on-call interventional radiologist was available at night, a significant delay to the start of the procedure was expected. Owing to the fact that the patient became increasingly haemodynamically unstable, surgery was the only immediately available option. Therefore, the option of embolisation was abandoned. Emergency replacement therapy with a recombinant factor VIII concentrate (Kogenate SF) was given at once and the patient was stabilised with fluids and taken to emergency laparotomy. Two litres of blood were evacuated from the peritoneal cavity and a 2 cm hole was seen in the gallbladder near the infundibulum, with active bleeding from the perforated gallbladder wall and the greater omentum, which had apparently been eroded by the prolonged inflammatory process. Small gallbladder concrements were identified and removed from the peritoneal cavity. An open cholecystectomy was performed, with haemostasis on the eroded greater omentum and extensive intra-abdominal lavage. Repetitive substitution with factor VIII concentrate was planned for the acute postoperative period, with factor VIII target levels of 80–100% (peak) and >40% (trough). In this patient, the elimination half-life of exogenous factor VIII was 6 hours, which is shorter than usual; therefore, a continuous intravenous replacement therapy with Kogenate SF (8′000 IE/24 h) was given for the first 3 days after surgery and then switched to a bolus regimen, initially three times a day and finally twice a day for a total of 14 days. Dosing intensity was chosen according to trough levels of factor VIII and the clinical outcome, as described above. The patient recovered without any further haemorrhage and was discharged in good condition.
Histological examination revealed acute ulcerous, phlegmonous and partially haemorrhagic cholecystitis.
Discussion
Derici et al1 attributed gallbladder perforation to ischaemia and necrosis secondary to inflammation. Perforations are usually located at the fundus, which is the part of the gallbladder that is most distant from the organ's blood supply.
Perforations that are not located at the fundus are often be covered by the greater omentum, as in our case, where the perforation was near the infundibulum.
We presume that the perforated gallbladder in our case was initially covered by omentum and its vessels were then gradually eroded by prolonged inflammation. This would explain why bleeding arose not only from the gallbladder, but also from the greater omentum. Bleeding from two sites at once in the setting of a severe coagulopathy led to a massive intra-abdominal haemorrhage; in this case, the covered location of the perforation was of no help to the patient.
Haemorrhagic cholecystitis is a rare complication of acute cholecystitis that can arise in the presence or absence of cholelithiasis. Haemorrhage cholecystitis in combination with gallbladder perforation can cause severe morbidity, as in our case.3 In most of the previously published cases, haemoperitoneum was due to transhepatic perforation; in our case, there was a free rupture into the peritoneal cavity, with bleeding from the gallbladder wall .
Tavernaraki et al suggest that perforation in cases of haemorrhagic cholecystitis is due to elevated intraluminal pressure in the presence of predisposing factors such as a bleeding diathesis, trauma, malignancy5 or anticoagulation therapy,6 which cause bleeding inside the gallbladder.
Transarterial embolisation of the bleeding is a relevant option in patients with increased operating risk coagulopathy as the risks of a surgical intervention, but its availability, especially at night, might be limited. Therefore, surgery often remains the only immediately available therapy,7 as our case has demonstrated.
The timing, duration and intensity of substitution with factor VIII concentrates are the same for emergency and elective interventions. They depend on the extent of the intervention and the risk of bleeding. Owing to the higher risk of conversion to laparotomy, substitution management the next day would have been on par with the laparoscopic surgery.
Learning points.
Acute cholecystitis is associated with a perforation rate of up to 15%. If the patient also has a coagulopathy, the treating team must be aware of the high risk of intra-abdominal bleeding.
Immediate initiation of adequate replacement therapy with coagulation factors is crucial and potentially life-saving.
Early surgery should be considered.
Interdisciplinary management by surgeons, haematologists and anaesthesiologists is mandatory before, during and after surgery.
Footnotes
Acknowledgement: We thank Ethan Taub for proof reading the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Derici H, Kara C, Bozdag AD et al. Diagnosis and treatment of gallbladder perforation. World J Gastroentero 2006;12:7832–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stefanidis D, Sirinek KR, Bingener J. Gallbladder perforation: risk factors and outcome. J Surg Res 2006;131:204–8. 10.1016/j.jss.2005.11.580 [DOI] [PubMed] [Google Scholar]
- 3.Tavernaraki K, Sykara A, Tavernaraki E et al. Massive intraperitoneal bleeding due to hemorrhagic cholecystitis and gallbladder rupture: CT findings. Abdom Imaging 2011;36:565–8. 10.1007/s00261-010-9672-y [DOI] [PubMed] [Google Scholar]
- 4.Nural MS, Bakan S, Bayrak IK et al. A rare complication of acute cholecystitis: transhepatic perforation associated with massive intraperitoneal haemorrhage. Emerg Radiol 2007;14:439–41. 10.1007/s10140-007-0621-1 [DOI] [PubMed] [Google Scholar]
- 5.Parekh J, Corvera CU. Haemorrhagic cholecystitis. Arch Surg 2010;145:202–4. 10.1001/archsurg.2009.265 [DOI] [PubMed] [Google Scholar]
- 6.Chen YY, Yi CH, Chen CL et al. Haemorrhagic cholecystitis after anticoagulation therapy. Am J Med Sci 2010;340:338–9. 10.1097/MAJ.0b013e3181e9563e [DOI] [PubMed] [Google Scholar]
- 7.Köhler G, Koch OO, Antoniou SA et al. Relevance of surgery after embolization of gastrointestinal and abdominal haemorrhage. World J Surg 2014;38:2258–66. 10.1007/s00268-014-2570-7 [DOI] [PubMed] [Google Scholar]


