Abstract
Thyroid carcinoma presenting as a hyperfunctioning thyroid nodule is rare. A further complexity is added when interpretation of the histopathology itself is not straightforward. We describe a case of a 16-year-old girl presenting with clinical and biochemical evidence of thyrotoxicosis, and a 4 cm thyroid mass. An ultrasound and thyroid uptake scan demonstrated a toxic adenoma. Owing to the nodule size, fine needle aspiration of the thyroid adenoma was performed, which showed findings consistent with toxic adenoma. However, in view of the size of the nodule, a hemithyroidectomy was performed. Histological examination of the thyroid revealed a follicular variant of papillary carcinoma of the thyroid, and the patient underwent completion thyroidectomy. We report on the case and briefly review the available literature relating to the diagnostic challenge of this presentation.
Background
Thyroid carcinoma presenting as a hyperfunctioning thyroid nodule is rare. Radionuclide imaging of thyroid hot nodules usually suggest a benign lesion with 1–10.3% of cases being malignant.1 Diagnosis is often not straight forward with uncertainty arising both with fine needle aspiration, where malignant tissue and adenoma can occur simultaneously,2 and histopathology, where rare subtypes require specialist expertise to make the diagnosis.3 We describe the case of a 16-year-old girl presenting with symptoms of thyrotoxicosis and a 4 cm thyroid mass as a result of a follicular variant of papillary carcinoma of the thyroid, a rare subtype of papillary carcinoma.3
Case presentation
A 16-year-old girl presented to the outpatient endocrinology clinic with a thyroid mass. The patient described symptoms of weight loss, tremor, frequent bowel movement and hair loss. She also described feeling tearful and anxious. She had previously been fit and well, with no history of irradiation to the head or neck. On examination, her blood pressure measured 136/80 mm Hg and heart rate 80 bpm. A mass measuring approximately 4 cm in diameter was detected on palpation of her thyroid gland. Thyroid function tests were performed, which showed a thyroid stimulating hormone (TSH) <0.03 MU/L (normal range 0.53–3.59 mU/L), free T4 39.4 pmol/L (12–20.6 pmol/L) and free T3 14.3 pmol/L (3.5–7.7 pmol/L), TSH receptor antibodies were negative. The patient was started on carbimazole and further investigations requested.
Ultrasound imaging revealed a hyperechoic and hypervascular nodule measuring 4 cm by 2.5 cm in the left lobe of the thyroid, with no pathological lymphadenopathy in the neck. In view of the size of the mass, fine needle aspiration was performed. Cytological analysis described a group of epithelial cells with mild nuclear enlargement, prominent nuclear overlapping and microfollicular structures. This appearance raised the possibility of differentiated thyroid epithelial neoplasm but was not diagnostic. An iodine-123 thyroid isotope scan was performed, which showed marked asymmetrical uptake. Within the left lobe of the thyroid there was a substantial soft tissue nodule that measured 2.6 cm. The remainder of the gland showed physiological suppression with no discernible uptake in the right lobe and the remainder of the left lobe. The conclusion was that this was in keeping with a solitary toxic nodule (figure 1). However, clinical concern was raised in view of the size of the thyroid mass and the atypical cytological findings. Following a multidisciplinary team discussion it was agreed the patient should undergo a left hemithyroidectomy. Perioperative findings were consistent with a left thyroid nodule without any evidence of lymphadenopathy. The left lobe of the thyroid measured 4×3×2.5 cm and weighed 14 g. There were no signs of local invasion. Initial histopathology confirmed a follicular adenoma, however, repeat histological examination of the thyroid demonstrated circumscribed, differentiated neoplasm of thyroid follicular cell origin, composed of closely packed follicles, some of which were enlarged with intraluminal blunt papillae. The nuclei were enlarged with evidence of nuclear membrane irregularity and grooves, and occasional intranuclear pseudoinclusions were also demonstrated. These findings were in keeping with the diagnosis of follicular variant papillary thyroid carcinoma.
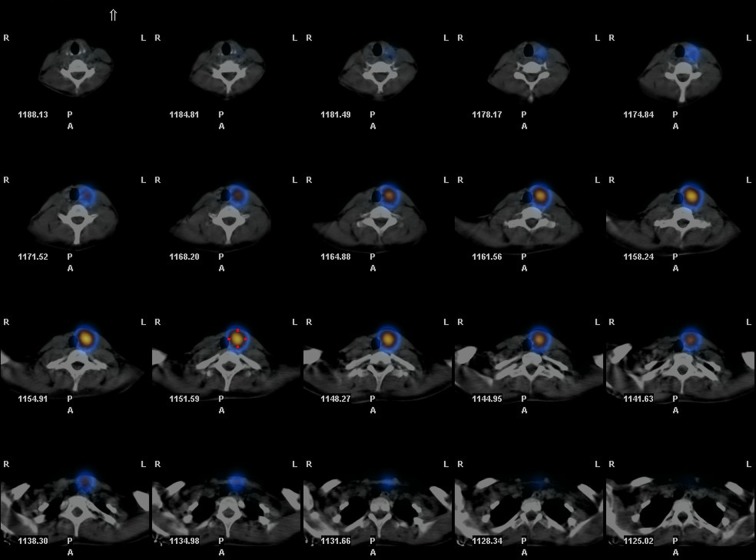
Figure 1.
(Iodine-123 thyroid isotope scan showing increased uptake at the site of the thyroid nodule with suppression of uptake elsewhere).
Outcome and follow-up
The patient underwent radio-iodine ablation after completion thyroidectomy, and is currently well and under active follow-up.
Discussion
Radionuclide imaging of thyroid hot nodules usually suggests a benign lesion with 1–10.3% of cases being reported as malignant.1 The exact incidence is difficult to quantify, one reason for this is the variability in how hot nodules are defined. Where malignancy is present it may coexist with hyperfunctioning tissue in the same gland but at different sites. In one study published in 2008, of 17 patients found to have malignancy in solitary autonomous adenoma, the tumour was actually outside the adenoma in seven cases. Furthermore, all of the seven were papillary thyroid carcinoma, with one of these having the follicular variant subtype.2 We found only two case reports of hyperfunctioning follicular variant papillary thyroid carcinoma.4 5
Despite the rarity of this presentation, our case highlights the importance of carefully evaluating a thyroid nodule in order to determine whether it is malignant. In the case described, there were three areas of uncertainty: the fine needle biopsy, the radionuclide scan and the histopathology.
Fine needle aspiration has a higher false negative rate as the size of the nodule increases.6 As such, the American Thyroid Association recommends patients with nodules greater than 4 cm who have indeterminate cytology should undergo total thyroidectomy as the first line of treatment. Radionuclide scanning would therefore be unnecessary and, as in the case described, a potentially misleading result avoided.
Follicular variant of papillary thyroid carcinoma is found in 9–22.5% of patients with papillary thyroid carcinoma.3 It is characterised by follicular architecture with nuclear features of papillary carcinoma. The nuclear features can be subtle, and histological interpretation is prone to intraobserver variation and, as such, can be mistaken for follicular adenoma. Post total thyroidectomy, due to the potential for metastatic spread, an iodine-123 whole body scan should be performed to detect for residual disease, and regular ultrasound imaging of the neck performed to monitor for pathological lymphadenopathy.
Learning points.
Up to 10% of hyperfunctioning ‘hot’ thyroid nodules have been reported as malignant.
Thorough investigation of thyroid adenomas should be routinely carried out with awareness of the limitations of radionuclide scanning and fine needle aspiration.
The diagnosis of rare subtypes in thyroid cancer require expert analysis of the histopathology, as in this case, to ensure accurate and timely diagnosis and treatment.
The follicular variant of papillary thyroid carcinoma is believed to behave in a clinical manner similar to classical papillary cancer and follows a similar indolent course, although a few cases could be aggressive. Hence there is a need for thorough evaluation of thyroid to exclude malignancy even in a clinical setting of hyperthyroidism.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kim JH, Na GJ, Kim KW et al. . Papillary thyroid carcinoma manifesting as an autonomously functioning thyroid nodule. Endocrinol Metab 2012;27: 59–62. 10.3803/EnM.2012.27.1.59 [DOI] [Google Scholar]
- 2.Pazaitou-Panayiotou K, Perros P, Boudina M et al. . Mortality from the thyroid cancer in patients with hyperthyroidism: the Theagenion Cancer Hospital experience. Eur J Endocrinol 2008;159:799–803. 10.1530/EJE-08-0468 [DOI] [PubMed] [Google Scholar]
- 3.Liu J, Singh B, Tallini G et al. . Follicular variant of papillary thyroid carcinoma. Cancer 2006;107:1255–64. 10.1002/cncr.22138 [DOI] [PubMed] [Google Scholar]
- 4.Bommireddipalli S, Goel S, Gadiraju R et al. . Follicular variant of papillary thyroid carcinoma presenting as a toxic nodule by I-123 scintigraphy. Clin Nucl Med 2010;35:770–5. 10.1097/RLU.0b013e3181e4dc7f [DOI] [PubMed] [Google Scholar]
- 5.Ruggeri RM, Campenni A, Giovinazzo S et al. . Follicular variant of papillary thyroid carcinoma presenting as toxic nodule in an adolescent: coexistent polymorphism of the TSHR and Gsa genes. Thyroid 2013;23:239–42. 10.1089/thy.2012.0279 [DOI] [PubMed] [Google Scholar]
- 6.Cooper DS, Doherty GM, Haugen BR et al. . Revised American thyroid association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 2009;19:1167–214. 10.1089/thy.2009.0110 [DOI] [PubMed] [Google Scholar]