Abstract
Esophageal atresia (EA) is the most common type of gastrointestinal atresia. The most common variant (type C) consists of a blind esophageal pouch with a fistula between the trachea and the distal esophagus. Surgical repair can be complicated by the development of benign stricture. Most strictures are amenable to dilation, but refractory strictures may require surgical intervention. A 24-month-old boy born with tracheoesophageal fistula and EA underwent surgical repair on day 1 of life. He developed esophageal stricture that responded to esophageal stent placement. Endoscopic biliary accessories can be safely used to dilate refractory esophageal strictures in children, and should be considered prior to seeking other complex alternatives.
Introduction
Esophageal atresia (EA) with or without tracheoesophageal fistula (TEF) is the most common type of gastrointestinal atresia, with occurrence rate of 1 in 3,000–5,000 births. The most common type is a blind upper esophagus with a fistula between the lower esophageal segment and the trachea. Surgical repair is the treatment of choice, but this may be complicated by development of anastomotic esophageal strictures that can be managed endoscopically using Savary-Gilliard bougies or balloon dilatators.1,2
An alternative method that has been reported in patients with severe strictures is retrograde gastric endoscopy, which has many complications. Major drawbacks of this technique include the risk of hypopharyngeal perforation and abdominal complications (bleeding, wound infection, fistulae), especially in patients who require minilaparotomy and gastrostomy for this retrograde approach to the esophagus.3 Endoscopic biliary accessories (balloons and stents) can be used to dilate non-traversable complex gastrointestinal strictures.4
Case Report
A newborn weighing 2,840 g was born at 39 weeks by Cesarean section due to breech presentation. Prenatal sonogram showed EA and TEF. Treatment included surgical repair of the EA and TEF on day 1 of life by primary end-to-end anastomosis. The patient subsequently developed a mid-esophageal stricture refractory to through-the-scope balloon dilation; the patient experienced symptoms and stenosis relapse shortly after each dilation. A 10 mm x 16 cm Endotek stent (Merit Medical Systems, South Jordan, UT) was placed, but was complicated by chest pain, cough, decreased oral intake, and high-grade fever, so the stent was removed after 3 days.
The patient was referred for surgical management. A biliary balloon dilator was used to decrease the risk of iatrogenic perforation due to the small size of the stricture (<4 mm) and because the stricture was long, fibrotic, and tortuous. At the initial esophagogastroduodenoscopy (EGD), a benign-appearing, intrinsic severe stenosis measuring 5 cm x 4 mm (inner diameter) was found 15 cm from the incisors (Figures 1 and 2). The stricture could not be traversed with an ultra-slim GIF-XP160 upper endoscope (Olympus America, Melville, NY), so biliary balloon dilators were passed over a guidewire and the stricture was dilated to 8 mm successfully.
Figure 1.
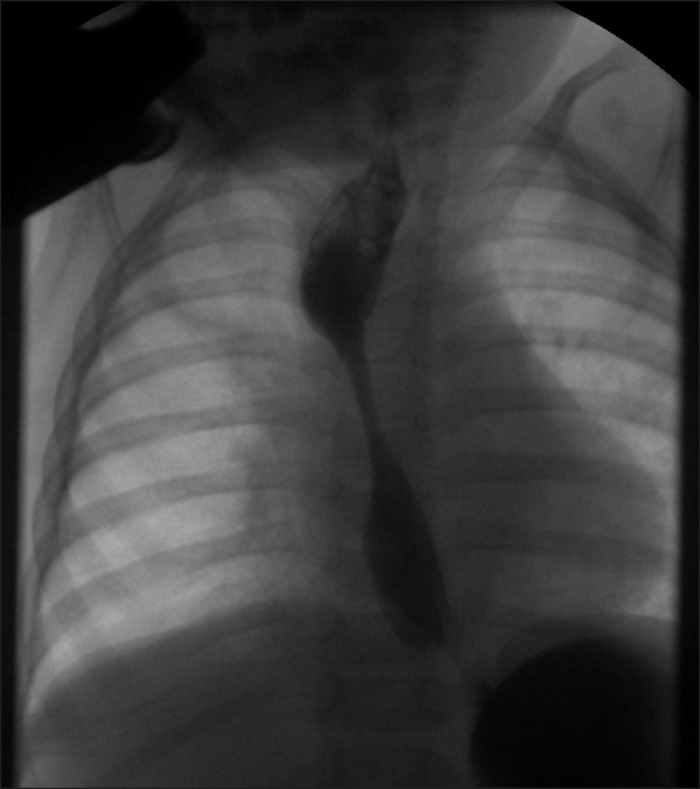
Mid-esophageal stricture found on EGD.
Figure 2.
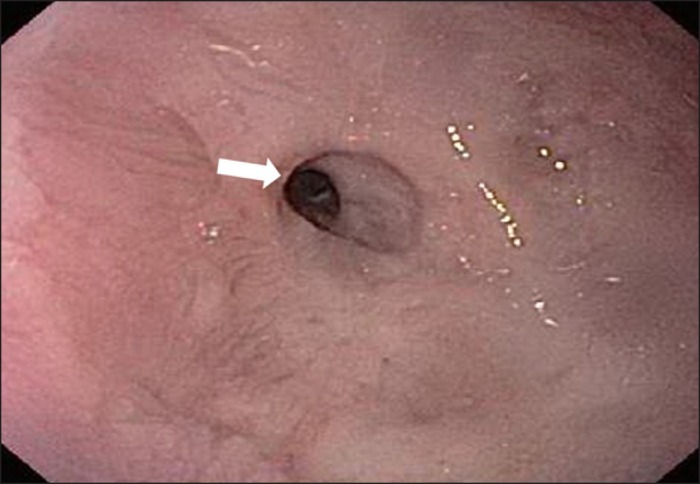
Endoscopic image of the stricture prior to dilatation.
After 1 week, repeat EGD with biliary balloon dilation to 8 mm was performed, followed by placement of a 10 mm x 6 cm VIABIL endoscopic prosthesis biliary stent (Gore Medical, Flagstaff, AZ) using a guidewire under fluoroscopic guidance without complications (Figure 3). We presumed that the biliary stent was better tolerated than the previous esophageal stent due to flexibility and smaller size. Six weeks later, the biliary stent was removed endoscopically and his stricture measured 5 cm x 10 mm. A fully covered, 12 mm x 70 mm ALIMAXX-ES esophageal stent (Merit Medical Systems, South Jordan, UT) was placed over guidewire under fluoroscopic guidance and the patient tolerated the procedure well (Figure 4). This stent was well tolerated for 5 weeks, but then the patient presented with vomiting and dysphagia to solids. The stent was removed; on exam, his stricture was open and could be traversed easily with a regular GIF-H180 upper endoscope (Olympus Imaging America, Center Valley, PA). Intralesional steroid of 1:1 diluted (triamcinolone 40 mg/mL) was performed during this procedure. A follow-up contrast study 4 weeks later showed that his stricture was still open with 12-mm inner diameter (Figure 5). Further EGDs and dilations may be needed, but this was the first time that his stricture remained open after endoscopic management.
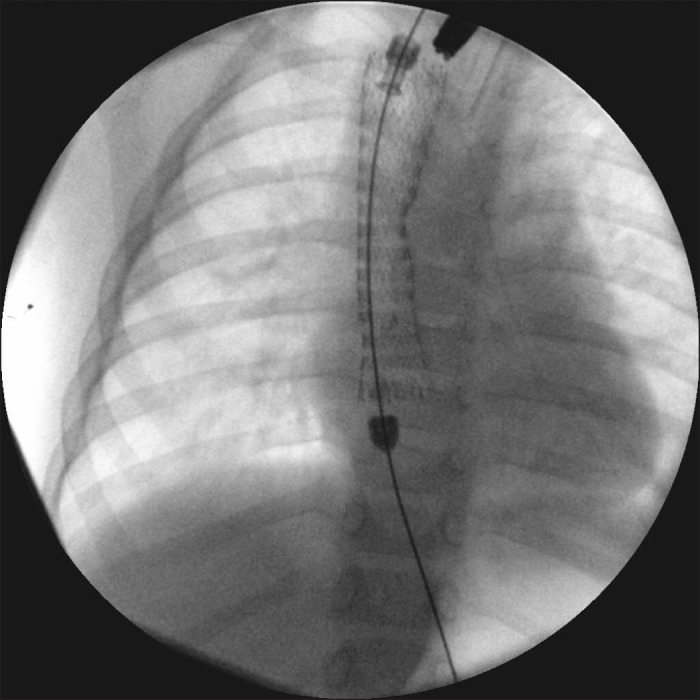
Figure 3.

Placement of a 10 mm x 6 cm biliary stent.
Figure 4.
Placement of a 12 x 70 mm esophageal stent.
Figure 5.

Contrast image showing resolution of the stricture.
Discussion
Most postoperative esophageal strictures are partial and amenable to endoscopic dilation. Patients with complete or nearly complete esophageal stricture may benefit from the use of endoscopic biliary accessories before sending them to surgery.
We describe a full-term infant with severe esophageal stricture post surgical repair of EA and TEF. The stricture was successfully dilated by biliary balloon dilator, allowing for placement of biliary stent, followed by placement of esophageal stent, a treatment progression that likely contributed to the long-term patency and success of the procedure. The sustainability of stricture patency will need to be evaluated with follow-up studies as clinically indicated.
There is paucity of data on the use of endoscopic biliary accessories (balloon and stents) and esophageal stent placement in the management of esophageal stricture in children. To our knowledge, the literature contains only 1 similar case report, wherein biliary accessories were used to bypass a very tight post-radiation therapy esophageal stricture in a 57-year-old laryngeal cancer patient.5 This approach should be considered in patients with complex esophageal strictures, especially after surgery, and prior to pursuing retrograde dilation or surgical repair.
Disclosures
Author contributions: R. Gebrail wrote the initial draft and is the article guarantor. I. Absah edited the draft.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
References
- 1. Gallardo LM, Fragoso Arbelo T, Sagaro G, et al. . Treatment of esophageal stenosis with Savary-Gilliard balloons in children. Gen. 1995;49(1):15–22. [PubMed] [Google Scholar]
- 2. Cho YK, Shin JH, Yook JH, et al. . Fluoroscopically guided balloon dilation of anastomotic strictures after total gastrectomy: Long-term results. Am J Roentgenol. 2007;188(3):647–51. [DOI] [PubMed] [Google Scholar]
- 3. Sullivan CA, Jaklitsch MT, Haddad R, et al. . Endoscopic management of hypopharyngeal stenosis after organ sparing therapy for head and neck cancer. Laryngoscope. 2004;114(11):1924–31. [DOI] [PubMed] [Google Scholar]
- 4. Parasher VK. A novel approach to facilitate dilation of complex non-traversable esophageal strictures by efficient wire exchange using a stent pusher. Gastrointest Endosc. 2000;51(6):730–1. [DOI] [PubMed] [Google Scholar]
- 5. Ahlawat SK, Davidson BJ, and Al-Kawas FH. Successful use of biliary accessories in antegrade dilation of complex upper esophageal stricture due to chemoradiation and surgery. Dis Esophagus. 2008;21(1):86–89. [DOI] [PubMed] [Google Scholar]


