Abstract
A 61-year-old woman presented with features of acute cholangitis and distal common bile duct obstruction. Histopathology from ampulla of Vater biopsy demonstrated extensive local amyloid deposition. Amyloidomas can cause local obstructive effects and have been described in the small intestine, stomach, and gallbladder. This is the second case of a discrete amyloid deposit causing extrahepatic biliary obstruction and cholangitis.
Introduction
Amyloidosis is a disorder of extracellular insoluble protein deposition, most commonly presenting with fatigue, light-headedness, and weight loss.1 Primary (AL-type) and secondary (AA-type) are the most common amyloid subclassifications, with smaller numbers of patients affected by dialysis-related, senile, and familial amyloidoses. Liver involvement in amyloidosis is common, reported in up to 70% patients at autopsy,2 but is usually asymptomatic.3 Jaundice is a poor prognostic indicator, and is most often due to intrahepatic amyloid deposition. Amyloid infiltration in the gastrointestinal system is usually diffuse,4 but focal deposits of amyloid may occur as pseudotumours, or “amyloidomas.” These have been described in the stomach, duodenum, jejunum, and gallbladder,5-7 where they may be mistaken for a primary malignancy and cause physical obstruction.
Case Report
A 61-year-old woman presented with 1 week of fever, rigors, and vomiting, and 4 months of malaise and dizziness. She described a 15-kg weight loss and nocturnal pain in both feet. Past medical history included cholecystectomy at age 54 years. Physical examination revealed mild right upper quadrant tenderness and bilaterally reduced proprioception in the great toe. Admission blood tests showed white cell count 22 x 109/L, C-reactive protein 72.5 mg/L, alkaline phosphatase 333 U/L, albumin 29 g/L, and prothrombin time of 13.1 s. CA 19-9 was not elevated, and she was not jaundiced.
Computerized tomography revealed calcific material within the distal CBD at the level of the ampulla, with dilation of the CBD and intrahepatic ducts. Cholangiography demonstrated dilation of the CBD with a distal filling defect (Figure 1), although no stone was retrieved with balloon trawl. The ampulla was noted to be inflamed and edematous, and biopsies were taken. Sphincterotomy was not done due to excessive bleeding from the biopsy, but a plastic stent was placed across the biliary orifice. Intravenous antibiotics were given for cholangitis, and the patient made an uneventful recovery.
Figure 1.
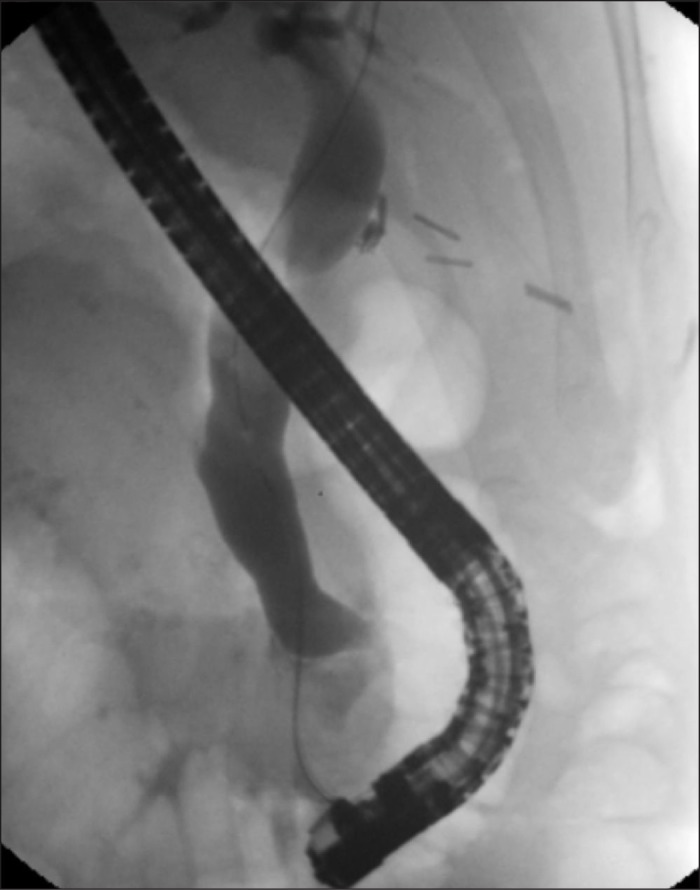
ERCP demonstrating dilated common bile duct with distal filling defect. Previous cholecystectomy clips noted.
Analysis of the ampullary biopsy revealed infiltration with a congophilic material, which showed apple-green birefringence consistent with amyloid. Detailed analysis confirmed AL-type amyloidosis (kappa subtype; Figure 2), with evidence of extensive local amyloid deposits replacing the normal structure. Scintigraphy did not identify any evidence of cardiac or renal amyloid involvement, and the patient had a good response to chemotherapy with cisplatin, vinblastine, and dacarbazine.
Figure 2.
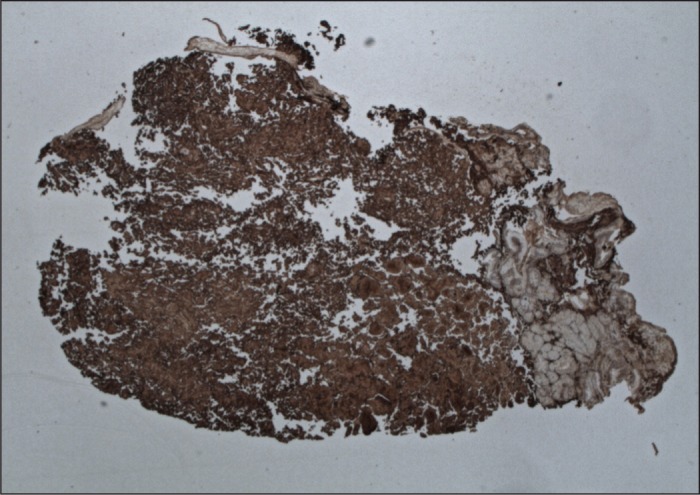
Ampullary biopsy with kappa light chain immunohistochemistry staining revealing infiltration with a congophilic material of apple-green birefringence consistent with amyloid.
Discussion
Gastrointestinal involvement in amyloidosis is common, with liver involvement reported in up to 90% of cases.4 Findings suggestive of liver involvement are hepatomegaly and persistently elevated alkaline phosphatase.8 The degree of hepatic dysfunction seen on liver function tests does not correlate well with the extent of systemic amyloid deposit,9 but liver involvement is often a poor prognostic indicator.1 Several case studies have identified amyloidosis as a cause of cholestatic jaundice,2,3,10-12 with evidence of perisinusoidal amyloid deposition in intrahepatic bile ducts causing physical obstruction to the flow of bile.1,13
Amyloid deposition in the gastrointestinal tract is usually diffuse,4 but localized amyloid pseudotumours or “amyloidomas” can form. These have been described in the stomach and gallbladder, where they may be mistaken for primary tumors,5-7 and in the small intestine, where they may cause intestinal obstruction. In one case, a large duodenal amyloidoma exerted a significant mass effect, resulting in duodenal obstruction and obstructive jaundice.6 This is the second reported case in which an amyloidoma at the ampulla of Vater caused CBD obstruction, resulting in jaundice and cholangitis.10 In our case, biopsy of the ampullary lesion revealed the diagnosis, and allowed for timely initiation of appropriate chemotherapy.14
Although gastrointestinal involvement in amyloidosis is common, the liver is never the sole organ affected.15 Amyloidosis still carries a significant mortality with a median 1-year survival of 50% in untreated AL amyloidosis.16 Over half of patients with evidence of hepatic amyloidosis will have proteinuric renal involvement or cardiac dysfunction, and renal failure remains the most frequent cause of death in patients with systemic amyloidosis.3 Although amyloidosis represents a rare cause of cholestatic jaundice, it is important to consider it in the differential, as many of the presenting features are non-specific.
Disclosures
Author contributions: J. Clough wrote the manuscript. R. Shah reviewed the manuscript and is the article guarantor.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
Acknowledgements: The authors would like to thank Professor Philip Hawkins at the National Amyloidosis Centre, University College, London, and Dr. Stephen Samson, Consultant Histopathologist, Epsom and St Helier NHS University Hospitals, NHS Trust for their assistance with this manuscript.
References
- 1.Petre S, Shah IA, Gilani N. Review article: Gastrointestinal amyloidosis: Clinical features, diagnosis, and therapy. Aliment Pharmacol Ther. 2008;27(11):1006–1016. [DOI] [PubMed] [Google Scholar]
- 2.Veluru CS, Soloman A, Sappati Biyanni RSR.. A case of cholestatic jaundice: Amyloidosis. Clin Gastroenterol Hepatol. 2013;8(10):e104–e105. [DOI] [PubMed] [Google Scholar]
- 3.Peters RA, Koukoulis G, Gimson A, et al. Primary amyloidosis and severe intrahepatic jaundice. Gut. 1994;35: 1322–1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Picken MM, Dogan A, Herrera GA. Amyloid and Related Disorders: Surgical and Clinical Correlations. New York, NY: Current Clinical Pathology; 2012 [Google Scholar]
- 5.Saindane AM, Losada M, Macari M. Focal amyloidoma of the small bowel mimicking adenocarcinoma on CT. Am J Roentgenol. 2005;185(5):1187–1189. [DOI] [PubMed] [Google Scholar]
- 6.Rodríguez OM, Carabias HA, Montano NE, et al. Obstructive jaundice caused by amyloidosis successfully treated with surgery. Gastroenterol Hepatol. 2007;30(4):229–31. [DOI] [PubMed] [Google Scholar]
- 7.Wu D, Lou JY, Chen J, et al. A case report of localized gastric amyloidosis. World J Gastroenterol. 2003;9(11):2632–2634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ebert EC, Nagar M. Gastrointestinal manifestations of amyloidosis. Am J Gastroenterol. 2008;103: 776–787. [DOI] [PubMed] [Google Scholar]
- 9.Gertz MA, Kyle RA. Hepatic amyloidosis (primary [AL], immunoglobulin light chain): The natural history in 80 patients. Am J Med. 1988;85: 73–80. [DOI] [PubMed] [Google Scholar]
- 10.Yoshiki Y, Yamamoto G, Takazawa Y, et al. AL amyloidosis with severe gastrointestinal invasion and acute obstructive suppurative cholangitis. Ann Hematol. 2012;91: 467–468. [DOI] [PubMed] [Google Scholar]
- 11.Mir-Madjlessi SH, Farmer RG, Hawk WA. Cholestatic jaundice associated with primary amyloidosis. Cleveland Clin Quarterly. 1972;39(4):167–75. [DOI] [PubMed] [Google Scholar]
- 12.Faa G, Van Eyken P, De Vos R, et al. Light chain deposition disease of the liver associated with AL-type amyloidosis and severe cholestasis: A case report and literature review. J Hepatol. 1991;12: 75–82. [DOI] [PubMed] [Google Scholar]
- 13.Terada T, Hirata K, Hisada Y, et al. Obstructive jaundice caused by the deposition of amyloid-like substances in the extrahepatic and large intrahepatic bile ducts in a patient with multiple myeloma. Histopathol. 1994;24(5):485–7. [DOI] [PubMed] [Google Scholar]
- 14.Palladini G, Merlini G. Current treatment of AL amyloidosis. Haematologica. 2009;94(8):1044–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lovat LB, Persey MR, Madhoo S, et al. The liver in systemic amyloidosis: Insights from 123I serum amyloid P component scintigraphy in 484 patients. Gut. 1998;42: 727–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.James DG, Zuckerman GR, Sayuk GS, et al. Clinical recognition of AL type amyloidosis of the luminal gastrointestinal tract. Clin Gastroenterol Hepatol. 2007;5: 582–588. [DOI] [PubMed] [Google Scholar]


