Abstract
We present a case of a large, sterile, subhepatic abdominal wall abscess secondary to foreign body reaction to dropped gallstones during laparoscopic cholecystectomy performed 10 years ago. Dropped gallstones are common complications of laparoscopic cholecystectomy, but they rarely result in abscess formation. When abscesses do occur, they may present a few months to a few years after surgery. It is important to recognize dropped gallstones as an etiology for subhepatic abscess in patients with history of laparoscopic cholecystectomy.
Introduction
The gold standard in the management of symptomatic gallstones is laparoscopic cholecystectomy. Dropped gallstones during laparoscopic cholecystectomy can be a nidus of infection and lead to the formation of an intraabdominal abscess, which may be misidentified as tumors or parasitic infections due to their similar radiologic appearance.
Case Report
A 72-year-old woman presented with a 6-month history of intermittent right upper quadrant abdominal and right flank pain unrelated to food intake. She denied fever, chills, night sweats, or weight loss. She had a laparoscopic cholecystectomy performed 10 years prior for symptomatic gallstones. Physical examination revealed erythema and mild tenderness on the right lateral aspect of the upper abdomen. Laboratory tests were unremarkable. A computed tomography (CT) of the abdomen showed a complex 21 x 5.8 x 8.8-cm subhepatic fluid collection with internal septations, which fistulized through the abdominal wall, forming a 5.6 x 2-cm subcutaneous fluid collection in the right flank (Figures 1 and 2). A hepatobiliary iminodiacetic acid (HIDA) scan and a magnetic resonance cholangiopancreatography (MRCP) were normal and showed no evidence of a bile leak. Ultrasound-guided drainage of the abscess produced 60 mL of thick, greenish, non-purulent fluid. Examination of the aspirate showed proteinaceous material with few inflammatory cells and many degenerated structures, suspicious for echinococcal cyst, but too poorly preserved for definitive diagnosis. Empiric intravenous ceftriaxone was started after aspiration of the fluid. Bacterial, fungal, and mycobacterial cultures of the abscess were negative, and ceftriaxone was stopped after a week. Testing for Mycobacterium tuberculosis and Entamoeba were negative. The patient was started on albendazole for suspected echinococcosis.
Figure 1.
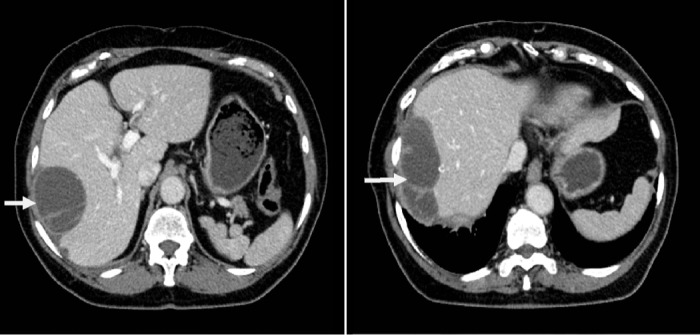
Abdominal CT showing a large subhepatic and perihepatic fluid collection with internal septations.
Figure 2.
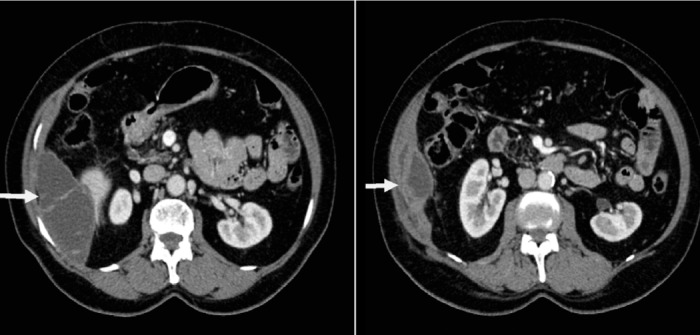
Abdominal CT showing subcutaneous fluid collection in the right flank following fistulization of the complex perihepatic fluid collection.
A PAIR procedure (puncture, aspiration, injection, and re-aspiration) with instillation of hypertonic saline was then performed, and 180 mL of thick greenish-white fluid was aspirated. The patient completed 6 weeks of albendazole; however, her symptoms persisted. A repeat CT scan failed to show a decrease in the size of the abscess. During exploratory laparotomy, 500 mL of greenish, non-purulent fluid was drained. Additionally, 28 gallstones were evacuated from the cavity. Fluid cultures were again negative for bacterial, fungal, and mycobacterial organisms. The patient's symptoms resolved following the surgery. Repeat CT scan performed 1 month after the surgery showed complete resolution of the abscess and normal liver parenchyma (Figure 3).
Figure 3.
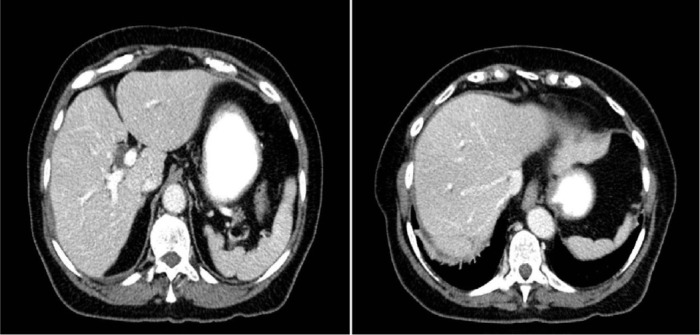
Abdominal CT 1 month after exploratory laparotomy showing resolution of the abscess.
Discussion
Gallbladder perforation and bile duct injury resulting in spillage of gallstones into the peritoneal cavity occurs in up to 40% of laparoscopic cholecystectomies.1 The complications from dropped gallstones are infrequent and have been reported to be about 1.7 per 1000 laparoscopic cholecystectomies.2 The most commonly reported complications of dropped gallstones are intra-abdominal and abdominal wall abscesses.2 These abscesses result from bacterial microcolonies that are often present throughout the interior of pigment gallstones.3 Pigment gallstones form as a composite of bacteria, bacterial gylcocalyx, and pigment solids.3 The gallstone matrix protects the bacteria from antimicrobial factors and can result in the development of an abscess. The mean duration between laparoscopic cholecystectomy and onset of symptoms is about 5.5 months, with a range of 0–3 years post-laparoscopic cholecystectomy.4 The rarity and chronicity of this problem can make the diagnosis challenging, and the abscess can be misidentified as tumors or parasitic infections due to their similar radiologic appearance. In our patient, the presence of degenerative cysts on pathology, along with the epidemiologic history and suspicious radiologic features, led us to a presumptive diagnosis of echinococcosis. However, our patient did not respond to the standard treatment for echinococcosis (albendazole and PAIR procedure).
Exploratory laparotomy is the treatment of choice for dropped gallstones. Percutaneous drainage is effective for resolving acute symptoms, but unless the gallstones are removed, recurrence of abscesses is common.8 It is uncertain whether antibiotics are required for treatment; however, most patients get a short course based on cultures that typically reveal E. coli, Klebsiella pneumonia, or Enterococcus.5 In our patient, cultures were negative, suggesting that the abscess was an inflammatory mass secondary to foreign body reaction to the dropped gallstones. The indolent nature of this inflammatory process explains the long duration between the laparoscopic cholecystectomy and the development of symptoms in our patient. Our case illustrates the importance of recognizing dropped gallstones in the differential diagnosis of subhepatic or intra-abdominal abscess in a patient with a history of laparoscopic cholecystectomy, regardless of the time elapsed from surgery.
Disclosures
Author contributions: AK Bartels and AR Murali wrote the manuscript. AR Murali is the article guarantor. J. Gonzales Zamora performed critical revision of the manuscript.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
Previous Presentation: This case report was presented as a poster at the ACG Annual Scientific Meeting; October 11-13, 2013; San Diego, California.
Disclaimer: The views expressed in the article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States Government.
References
- 1.Gerlinzani S, Tos M, Gornati R, et al. Is the loss of gallstones during laparoscopic cholecystectomy an underestimated complication? Surg Endosc. 2000;14(4):373–374. [DOI] [PubMed] [Google Scholar]
- 2.Zehetner J, Shamiyeh A, Wayand W. Lost gallstones in laparoscopic cholecystectomy: All possible complications. Am J Surg. 2007;193(1):73–8. [DOI] [PubMed] [Google Scholar]
- 3.Stewart L, Smith AL, Pellegrini CA, et al. Pigment gallstones form as a composite of bacterial microcolonies and pigment solids. Ann Surg. 1987;206(3):242–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brockmann JG, Kocher T, Senninger NJ, Schürmann GM. Complications due to gallstones lost during laparoscopic cholecystectomy. Surg Endosc. 2002;16(8):1226–32. [DOI] [PubMed] [Google Scholar]
- 5.Horton M, Florence MG. Unusual abscess patterns following dropped gallstones during laparoscopic cholecystectomy. Am J Surg. 1998;175(5):375–9. [DOI] [PubMed] [Google Scholar]


