Abstract
Biliary complications are being increasingly encountered in post liver transplant patients because of increased volume of transplants and longer survival of these recipients. Overall management of these complications may be challenging, but with advances in endoscopic techniques, majority of such patients are being dealt with by endoscopists rather than the surgeons. Our review article discusses the recent advances in endoscopic tools and techniques that have proved endoscopic retrograde cholangiography with various interventions, like sphincterotomy, bile duct dilatation, and stent placement, to be the mainstay for management of most of these complications. We also discuss the management dilemmas in patients with surgically altered anatomy, where accessing the bile duct is challenging, and the recent strides towards making this prospect a reality.
Keywords: Liver transplant, Biliary, Complications, Strictures, Bile leak, Management, Endoscopy, Endoscopic retrograde cholangiography, Biloma, Stone, Cast
Core tip: Biliary complications are being increasingly encountered in post liver transplant patients because of increased volume of transplants and longer survival of these recipients. Overall management of these complications may be challenging, but with advances in endoscopic techniques, majority of such patients are being dealt with by endoscopists rather than the surgeons. Our review article discusses the recent advances in endoscopic tools and techniques which have proved ERCP with various interventions, like sphincterotomy, bile duct dilatation, and stent placement, to be the mainstay for management of most of these complications. We also deliberate the management dilemmas in patients with surgically altered anatomy, where accessing the bile duct is challenging, and the recent strides towards making this prospect a reality.
INTRODUCTION
Biliary tract complications (BTC) are described as Surgeons’ “Achilles Heel” after liver transplantation (LT)[1]. They constitute a major source of morbidity after LT and pose a challenge in both diagnosis and treatment. The incidence of BTC varies from 5% to 32% in various studies and has been decreasing with time; however, newer challenges are emerging with the more widespread use of living donor, donation after circulatory death and split-liver transplants[2,3]. The different complications that can be seen post LT include biliary strictures, leaks, cast formation, papillary stenosis and other less common ones[4,5]. Conventionally, post-LT biliary complications can be referred to as early (within 30 d of LT), delayed (1-3 mo post-LT) and late (beyond 3 mo post-LT). Even though each complication has a predominant manifestation period, for management purposes the clinical presentation and diagnosis are more important. With the advancement of imaging techniques, most of these complications are diagnosed using non-invasive imaging like traditional ultrasound (US), computed tomography (CT), magnetic resonance cholangiopancreatography (MRCP) and endoscopic ultrasound (EUS) with more invasive techniques like percutaneous transhepatic cholangiography (PTC) and endoscopic retrograde cholangiography (ERC) used for therapeutic purposes[6,7]. Over the last decade, there has been significant improvement in endoscopic techniques with an increase in the array of endoscopic assist devices, and consequently most of these complications are managed endoscopically, which will be the focus of this review.
TYPES OF SURGICAL RECONSTRUCTION AFTER LIVER TRANSPLANT
The technique of biliary reconstruction utilized during LT greatly influences the biliary tract complications seen in these patients[8-10]. It is necessary to be cognizant with the anatomy of the liver segments and its ducts, to be able to successfully diagnose and manage these complications. The two most common methods of biliary reconstruction include choledocho-choledochostomy (CC) or duct-to-duct anastomosis; and Roux-en-Y hepaticojejunostomy or choledochojejunostomy (RYC). It is imperative for endoscopists to have a thorough understanding of these anastomotic procedures as the former can be approached via conventional ERC whereas for the latter a percutaneous route is preferred. There is also an increasing usage of living, related-donor and split-liver transplants, because of limited availability of deceased donor liver transplants. During this procedure anastomosis is fashioned between donor’s right hepatic duct to the recipient’s common bile duct, which is even more complex than the traditional methods due to variability of the anatomy.
DIAGNOSIS AND EVALUATION OF BTC AFTER LT
Recognizing the risk factors for development of biliary complications is an important aspect of overall management, because if a risk factor is identified and appropriate remediation steps taken, the natural course of these complications may be altered. The common list factors are listed in Table 1 and discussed in detail at appropriate places in the article. Post-LT, patients with BTC can have varied presentations, which may range from asymptomatic transaminasemia to frank jaundice with abdominal pain and cholangitis. It is imperative to differentiate obstructive cholestasis from a non-obstructive cause like rejection - acute or chronic, drug induced cholestasis or recurrence of primary disease[11]. This is usually achieved with the help of imaging, which includes trans-abdominal ultrasound with Doppler, CT, MRCP, EUS, and HIDA scan (hepatobiliary iminodiacetic acid scan).
Table 1.
List of risk factors responsible development of various biliary complications
| Risk factor | Mechanism | Resultant biliary complication |
| HAT or stenosis | Being the main vascular supply to the bile duct, any compromise to integrity of HA or its branches induces acute and chronic ischemia of the biliary system | Anastomotic disruption Bile leak NAS AS Biliary cast syndrome |
| Type of transplant | Live-donor LT has higher overall biliary complications compared to Orthotopic LT | Bile leak HAT Unplanned re-explorations Portal vein thrombosis |
| Type of donor | DCD LT has higher biliary complication rate compared to DBD LT. This is because of increased risk of experiencing insufficient organ perfusion. Also increased risk if ABO blood group incompatibility between donor and recipient | Strictures (NAS) Bile duct filling defects (stones/sludge/clots/casts) |
| Type of anastomosis (biliary reconstruction) | Duct-to-duct CC anastomosis is preferred whenever possible, being simple and prevents enteric reflux into bile ducts, compared to RYC | Comparative biliary complication data is conflicting |
| Graft related factors | Use of grafts from older donors or grafts with increased steatosis (extended criteria), as well as increased cold (CIT) and warm ischemia times | Strictures (NAS and AS) Bile leak Bile duct filling defects (stones/sludge/clots/casts) |
| Surgical (or technical) factors-during both donor and recipient surgeries | Excessive dissection of periductal tissue during the procurement of native liver Excessive electrocautery to control bleeding during surgery Tension between the two ends of the biliary anastomosis Suture material used Denervation or injury to sphincter | Bile leak AS Mucocele Sphincter of Oddi Dysfunction |
| Placement of T-tubes (old strategy) | This increases chances of delayed healing, and may cause bile leaks. | Bile leak Hemobilia Infections (Cholangitis and Peritonitis) |
| Pre-LT factors | Infections (CMV or intra-abdominal infections) Diagnosis for LT: PSC or AIH | Infections (Cholangitis and Peritonitis) Strictures (NAS and AS) Bile duct filling defects (stones/sludge/clots/casts) |
| Post-LT factors | Immunosuppression: Emerging evidence that Sirolimus based regimen have higher risk of biliary strictures Infection, Acute cellular rejection, Obstruction, etc. Post-operative small bile leak is risk factor for future strictures Early HCV recurrence post-LT also increases inflammation and hence risk of strictures | Strictures (NAS and AS) Biliary cast syndrome |
HAT: Hepatic Artery Thrombosis; NAS: Non-anastomotic stricture; AS: Anastomotic stricture; DCD: Donor after cardiac death; DBD: Donor after brain death; CC: Choledocho-choledochostomy; RYC: Roux-en-Y choledochojejunostomy.
US with doppler can diagnose hepatic artery thrombosis in LT patients with a sensitivity of 91% and specificity of 99%[12]. Hepatic artery thrombosis is a risk factor for biliary leaks due to ischemic injury and hence, if detected on Doppler, warrants a confirmatory hepatic angiogram[2]. US can also be used to diagnose biliary strictures with a specificity of 98%; however, normal US findings do not exclude it and require further investigation with MRCP[13,14]. At present, MRCP is the initial imaging of choice to evaluate an LT patient for a biliary tract complications[15]. It provides detailed evaluation of both extra- and intra-hepatic biliary tree and can potentially avoid use of direct cholangiography[14]. It has several advantages over traditional and direct cholangiography, as it is non-invasive, there is no need of sedation, has minimal side effects and can demonstrate ducts both below and above a stricture. Several studies have been conducted to evaluate its role in LT patients with suspected biliary obstruction and in a meta-analysis, which included almost 400 LT-patients, MRCP was found to have a sensitivity of 96%, specificity of 94% with a positive likelihood ratio of 17 and a negative likelihood ratio of 0.04 for diagnosis of biliary obstruction[16-19]. However, it has limited role if LT was performed along with bilio-enteric anastomosis and for diagnosis of malignant strictures[16,20]. CT scan has limited role in evaluation of biliary tract complications in LT patients and maybe used to diagnose abscesses or fluid collections associated with biliary leaks.
TYPES OF BTC AFTER LT AND THEIR MANAGEMENT
Biliary strictures
Biliary strictures are the commonest complications after liver transplantation, with an incidence of 13% following deceased donor liver transplant (DDLT) but much higher (19%-32%) among living donor liver transplants (LDLT)[8]. They are encountered irrespective of type of anastomosis, although may be more common with Roux-en-Y hepaticojejunostomy or choledochojejunostomy reconstructions than duct-to-duct anastomoses[21]. They can be classified according to time of stricture development from LT as early (within 1 mo post-LT) vs late (more than 1 mo post-LT) or classified according to anatomical site into two categories-anastomotic strictures (AS) and non-anastomotic strictures (NAS) or ischemic strictures.
AS are usually single, localized to the site of anastomosis, short in length and occur within a year after LT[6,8] (Figure 1). Recent literature suggests their incidence to be < 10%, and they are formed as a result of ischemia, fibrosis or bile leak during or after the surgery. They are a reflection of intra-operative technical problems or small bile leaks or transient ischemia, resulting in peri-anastomotic fibro-inflammatory response leading to stenosis. Since bile leak is an important risk factor for development of AS, they need to be recognized early and managed appropriately. They can also form due to the sub-optimal surgical techniques like inappropriate suture material and excessive use of cautery for control of bleeding, in which case they are formed relatively early in the post-operative period[8]. Furthermore, there is emerging evidence that type of immunosuppression being used may have a role in development of AS, and need for early ERC for management of AS[22]. Most patients with very early stricture post-OLT may not have true AS, but a stenosis due to post-operative edema and inflammation, which responds very well to single dilatation and/or stenting session. True AS usually occurs between 3-12 mo after LT.
Figure 1.
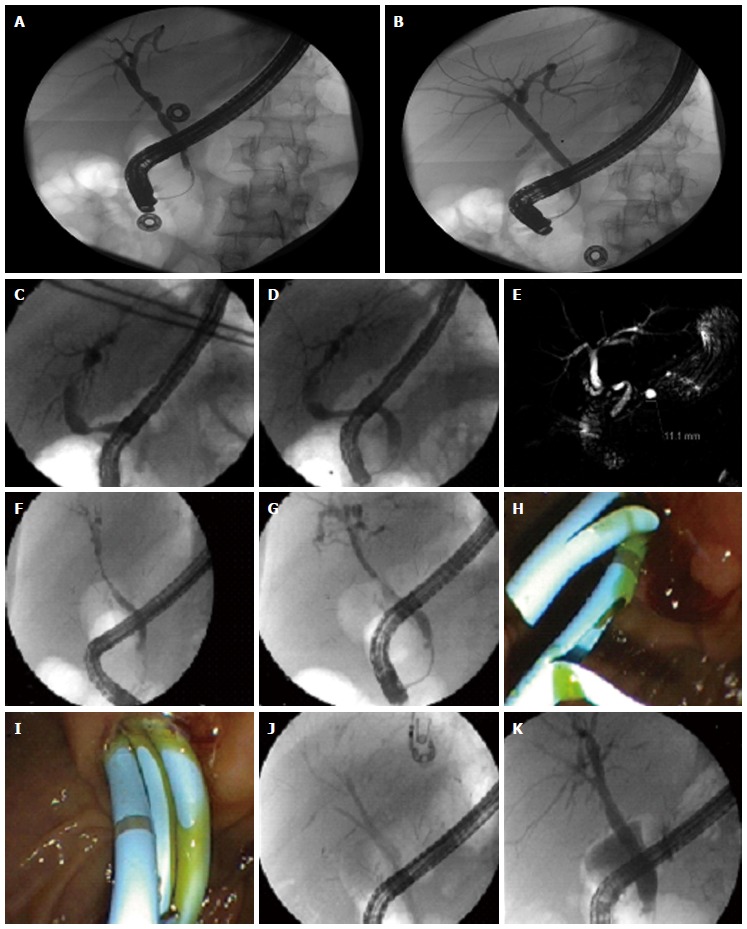
Different management strategies for biliary strictures. A: Post-LT anastomotic biliary stricture (as seen on ERC); B: managed with balloon dilatation only; C: Post-LT anastomotic biliary stricture (as seen on ERC); D: Managed with balloon dilatation; E: MRCP image of the same stricture; F: Long segment biliary stricture due to global hypotension post-LT; G: Dilatation performed with biliary balloon; H: Followed by placement of two plastic stents; I: Due to inadequate effect with two stents, sequential therapy strategy adopted with placement of three stents; J: Fluoroscopic image of three stents in right posterior and anterior hepatic and left hepatic ducts; K: Final cholangiogram suggesting a much improved bile duct diameter. ERC: Endoscopic retrograde cholangiography; LT: Liver transplantation.
NAS, on the other hand, tend to be multiple, longer in length and are either intrahepatic or in the donor duct proximal to anastomosis, and defined as being present more than 0.5 cm away from anastomotic site. They tend to occur earlier than AS with mean time of presentation 3-6 mo post-LT and have an incidence of 5%-15%[23,24]. Although most NAS are multifactorial, they can further be divided into 3 sub-types based on their etiology: (1) macroangiopathic - secondary to hepatic artery thrombosis (HAT) leading to biliary destruction; (2) microangiopathic - secondary to prolonged use of vasopressors in the donor, donation after cardiac death (DCD), prolonged warm and cold ischemic events; and (3) immunogenic - in patients with primary sclerosing cholangitis, ABO incompatibility, chronic rejection, CC chemokine receptor 5delta32 polymorphism or autoimmune hepatitis, which may act as an independent risk factor[8,23,25]. NAS can also be referred to as type I (extra-hepatic), or type II (intra-hepatic) and a combination of two[26]. Furthermore, Buis et al[27] proposed another classification of the anatomic regions of the biliary tree affected by non-anastomotic biliary strictures: hilar bifurcation (zone A), ducts between the first- and second-order branches (zone B), between second- and third-order branches (zone C) and in the periphery of the liver (zone D). Vascular NAS develops because the blood supply to donor bile duct comes from recipient hepatic artery, which is susceptible to ischemic injury post-transplant, while its native alternative supplies from smaller collaterals and branches of other arteries are transected during organ retrieval. The immunogenic NAS tend to occur later than vascular NAS. Because of their established relationship with ischemia, vascular patency of hepatic artery must be ascertained in these patients with a Doppler ultrasound. Patients who develop manifestations of NAS within the first year of transplant or have recurrent cholangitis, have the most unfavorable prognosis[28].
Management: Historically, post-LT biliary strictures were managed surgically via Roux-en-Y hepaticojejunostomy. However, over the past decade there has been tremendous improvement in endoscopic techniques, making endotherapy the treatment of choice for management of these strictures[29-31]. PTC and surgery are less often utilized, and usually reserved for cases where ERC cannot be used or has failed. Although not evidence-based, ursodeoxycholic acid is sometimes used to increase bile flow, and lower the chances of stone formation.
ERC is generally used to perform endoscopic biliary sphincterotomy (EBS) followed by balloon dilation and placement of biliary stent(s) to treat biliary strictures (Figure 1). Balloon dilation, if performed alone, has a high recurrence rate of 62% which decreases to 31% when performed with stent placement[32,33]. However, a recent prospective study by Kulaksiz et al[34] showed that dilation alone was as effective as dilation plus stent placement and in fact, stent placement was associated with a higher complication rate. However, more data is needed to clarify this discrepancy.
The most commonly used approach for treatment of AS consists of placement of large-bore 10-French plastic stents after balloon dilation and exchanging them every 3 mo (Figure 1). The median duration of plastic stent patency is around 3 mo (range 2-4 mo), as they are prone to debris deposition in their lumen resulting in obstruction, and risk of cholangitis. This approach has a success rate of 75% to 91% according to different studies for DDLT[32,35-38] but decreases to 37%-71% in patients with LDLT[39,40] because of the more complex duct-to-duct anastomosis. Factors limiting efficacy include peripheral location and presence of smaller and multiple biliary anastomotic strictures. It is also advised that balloon dilation should not be performed for very early strictures and for strictures in the setting of an anastomotic leak to prevent disintegration of biliary anastomosis. Severe complications of this technique are rare, although, a large study showed a complication rate of 6.6% per procedure which increases to 21% per patient as they get more than one procedure[41]. Some of the complications include pancreatitis, cholangitis, stent migration and hemorrhage. There was no death attributable to the procedure itself. An alternative approach to manage biliary strictures is to place maximum number of stents possible, which can then be exchanged at frequent intervals (Figure 1). This method is more aggressive but has shown to achieve a high long-term stricture resolution rate of 90%-94% with less frequent episodes of cholangitis[42,43]. This is a particular advantage of endoscopic therapy, as multiple stents cannot be placed using percutaneous catheter.
Metallic stents are generally useful only for malignant biliary obstruction as they provide effective palliation with a larger diameter (viz. 30-Fr) and longer patency[44]. They are either balloon-mouthed or self-expanding metallic stents (SEMS), but the fact that metal stents cannot be removed makes them less favorable in the setting of benign biliary diseases. Furthermore, possibility of reactive hyperplasia resulting in sludge/stone formation proximal to the stent poses a technical challenge, especially when SEMS cannot be removed. However, covered-SEMS (CSEMS = metallic skeleton with biocompatible and resistant synthetic covering viz. silicon, polyether polyurethane, polyurethane and expanded polytetrafluoroethylene) can be easily removed as the outer coating of the stents prevents tissue ingrowth, seen in about 20% patients. The major limitation with fully covered SEMS, however, is the relatively higher migration rate (6%-10%), which is now counterbalanced by development of partially-covered SEMS (PCSEMS), which provide advantages of covered stent but lower migration rates. Different types of metal stents are currently available, differing in their composition, like stainless steel or nitinol (which is a biocompatible metal alloy of titanium and nickel). Currently available SEMS are either fully covered (Viabil, Wallflex and Niti-S ComVi, etc.), or partially covered (Wallstent, Wallflex, etc.). Vandenbroucke et al[45] showed that Wallstents used in benign strictures after LT can be removed in 66% of patients and offer an option in patients with persistent proximal or anastomotic strictures who have multiple co-morbidities to undergo hepaticojejunostomy or re-transplantation. Similarly, Tee et al[46] showed benefit of such SEMSs in patients with refractory post-LT anastomotic biliary strictures. A recent meta-analysis by Kao et al[47] inferred that although SEMS appears to be promising strategy in management of anastomotic biliary strictures in post-LT patients, but current evidence is not enough to suggest clear advantage of SEMS over multiple plastic stents.
NAS are generally more difficult to treat and even though there have been several advancements in endoscopy, overall endoscopic management of NAS remains sub-optimal and endoscopic therapy only acts as a bridging therapy to liver transplantation. This is due to the fact that balloon dilation of all NAS is not feasible (Figure 2) and stent occlusion is rather rapid because of the smaller caliber of the intrahepatic ducts where these strictures are commonly observed. Basic management principles including sphincterotomy and stent placement with scheduled exchange are similar to AS, but endoscopic therapy of NAS typically utilizes smaller diameter balloon dilation (of 4- to 6-mm compared with 6 to 8 mm for AS). Also, just like AS, strategies like use of multiple stents, and stents of progressively increasing diameter have been employed in management of NAS successfully. However, despite all these maneuvers, there is evidence that NAS requires longer time to respond to endoscopic therapy (dilatation + stenting) compared to AS (185 vs 67 d)[48]. Use of conventional stents like Amsterdam stent is less satisfactory since these stents are rigid and do not have side holes for draining bile. However, long and large-caliber (up to 20 cm with 10 Fr), flexible and fenestrated stents (Johlin pancreatic wedge stents) can be used. The flexibility helps them to adapt to the tortuous contours of the intrahepatic ducts and multiple side holes allow adequate bile drainage. Endoscopic therapy for NAS, for reasons explained above, has an overall low success rate of 25%-33% in LDLT and 60% in DDLT[40]. In cases of NAS associated with early HAT, aggressive management with either revascularization or early re-transplantation is the key to management, prior to development of intrahepatic complications like biloma and abscess formation.
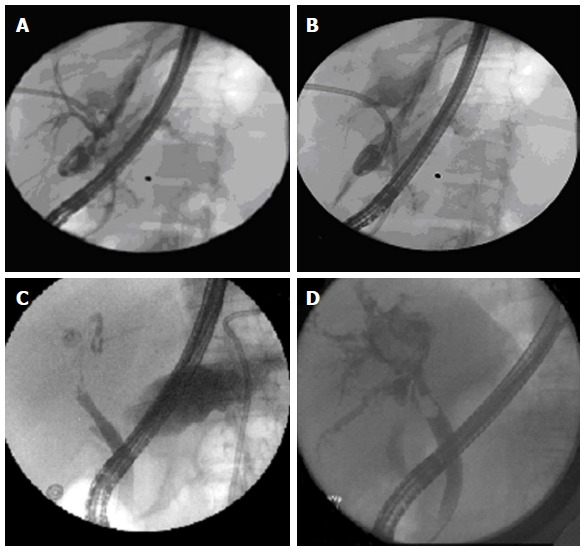
Figure 2.

Diffuse non-anastomotic intra-hepatic biliary structuring seen in a donation after cardiac death liver transplant patient, not amenable to endoscopic therapy.
Endoscopic therapy has generally been reserved for duct-to-duct anastomosis; however, with introduction of single (SBE) and double balloon enteroscopy (DBE), deep ERC can be performed even in patients with Roux-en-Y hepaticojejunostomy[49,50]. A large, multi-centric study by Shah et al[51] showed that in patients with surgically altered biliary anatomy, SBE, DBE or rotational over-tube enteroscopy can be used to perform ERC successfully in 88% of patients in whom papilla is reachable. Once the duct is accessed, all interventions can be performed like stricture dilatation or stent placement. Another recent advancement has been the use of steerable ERC cannulas like Swing-Tip cannula, which is potentially helpful equipment in management of hilar strictures by using multiple guide wires, and repeated dilation of strictures with placement of stents. These cannulas also help to achieve faster cannulation of the bile duct[52].
Direct cholangioscopy using SpyScope technology has also been utilized to visualize biliary anatomy, and diagnose and manage biliary strictures. It has been studied to be safe and technically superior to conventional cholangiogram in different reports[53-56]. Siddique et al[57] demonstrated that direct choledochoscopy also helps in providing targeted treatment to patients. Exciting advancements in this field are happening, although not rapidly enough to make cholangioscopy a consistent tool in management algorithm of post-LT strictures. Balderramo et al[58] observed two distinct visual patterns of post-LT AS on direct cholangioscopy, described either as erythema or as edema, sloughing and ulceration, to help predict outcomes after endoscopic therapy. AS patients with only edema responded better with endoscopic therapy, while patients with sloughing and ulceration needed longer duration of stenting[58]. Different types of cholangioscopes (Polyscope) and techniques like use of methylene blue are combined with cholangioscopy to diagnose and delineate features of biliary strictures in patients post-LT[59,60].
Apart from endoscopic therapy, percutaneous transhepatic cholangiography (PTC) can also be used for treatment of AS. However, it is usually reserved for patients with bilio-enteric anastomosis or patients who have failed endoscopic treatment or are at higher risk of complications like bile leaks, infections and hemorrhage[11,61]. Surgery and re-transplantation are reserved for strictures refractory to endoscopic therapy, when all endoscopic and non-surgical options have been exhausted.
Biliary leaks and bilomas
Biliary leaks can be seen in 10%-25% of patients after LT. Although, their incidence has decreased in post-MELD era, it is seen more common after LDLT[62-64]. Biliary leaks mostly occur at 3 sites-anastomotic site, exit site of T-tube and at the site of cystic duct remnant[65]. The bile leaks at anastomotic site are reflection of dehiscence due to technical errors, tension or ischemia and devascularization of the tissue surrounding the biliary tree, in which case hepatic artery thrombosis is a common culprit and must be investigated with ultrasound Doppler. Less common sites of bile leak include ischemic injury to extra-hepatic bile duct (at non-anastomotic site), gallbladder fossa, aberrant bile duct (Luschka’s duct) and cut surface of liver in LDLT or split livers (Figure 3). If bile extravasation occurs within the liver parenchyma or abdominal cavity, it may form collections called as biloma. Biliary leaks are generally divided according to time of occurrence into[66]: (1) early-occur within a month of the transplant and are usually associated with anastomotic leaks, ischemic injury and leakage around T-tube insertion site[2]; (2) late-occur more than a month after LT and noticed usually at the time of T-tube removal[67,68]. These are less common. Use of steroids or immunosuppressant medications post-LT is also alleged to hamper the healing process after T-tube removal.
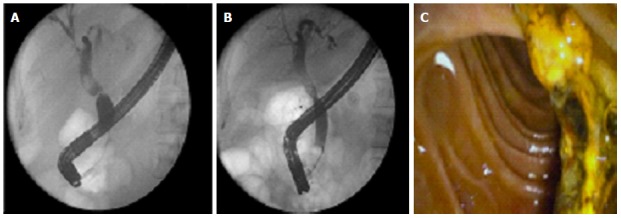
Figure 3.
Management strategies for bile leak and biloma. A: Bile leak from split surface of the liver in a patient with split-liver transplant; B: Managed successfully with endoscopic plastic stent placement; C: In a separate patient, bile leak successfully managed by placement of a fully covered metal stent; D: In yet another patient, intrahepatic biloma, which becomes apparent on occlusion cholangiogram.
Biliary leaks may present with abdominal pain or distension or patient might be asymptomatic, in which case, it is detected accidentally on abdominal imaging. One of the early indicators is the persistence of bile in the operative drain output. This can be confirmed with the help of a T-tube cholangiogram (in patients with a T-tube), or imaging like radionuclide scan (HIDA) or MRCP that can reliably detect a biloma and may localize the level of the leak[69].
Management: Most patients with biliary leaks can be managed endoscopically. ERC is most often used to perform biliary sphincterotomy and placement of biliary stent that can be kept in place for up to 2-3 mo (Figure 3). Although symptom resolution is fast after stent placement, the actual healing of leak may take up to 6-10 wk. Several studies suggest a success rate of 80%-90% using this strategy[8,70,71]. In case of an associated stricture, stent placement across the leak and stricture are prudent. In case of T-tube associated bile leaks confirmed on T-tube cholangiogram, leaving the drain open might suffice, without need for any further interventions. Naso-biliary drainage can also be performed in place of biliary stenting and Saab et al[72] in fact suggested that it might be the preferred strategy for management of biliary leaks. Although naso-biliary tubes can be useful for cholangiographic follow-up without further endoscopies and confirmation of leak sealing, however are very poorly tolerated. A small study showed that small leaks can be managed with sphincterotomy alone[73], however this is not the usual practice. In certain circumstances, along with bridging provided with the stent, drainage of the fluid collection might be needed, especially in large biloma with no communication with bile duct. This can be performed via EUS guided trans-gastric drainage or the traditional IR-guided drainage. Usually small bilomas resolve spontaneously, if there is adequate communication with duct, and some may require placement of a biliary stent. Despite these endoscopic advancements and options, there may be an occasional case where biliary leak cannot be treated endoscopically and thus requires surgery. These special cases include large anastomotic leaks, cases with Roux-en-Y anastomosis, early biliary leaks (< 1-2 wk after LT), bile duct necrosis or failure of primary therapy[3,69].
Sphincter of Oddi Dysfunction or papillary stenosis
Sphincter of Oddi Dysfunction (SOD) has an incidence of 2%-3.5% after LT. It is an incompletely understood and poorly defined syndrome of questionable significance[74]. It is thought to occur secondary to denervation of Sphincter of Oddi during LT leading to a hypertonic sphincter. It can be divided into 2 types based on the mechanism of its pathogenesis: (1) SOD with stenosis - which occurs due to scarring and inflammation. The contributing processes can be CBD manipulation during LT, stone passage through papilla, or infection. Sphincter of Oddi has high basal pressure in this type; and (2) SOD with dyskinesia - which occurs due to functional disturbance of the sphincter resulting in intermittent biliary blockage. The sphincter in these cases has low basal pressure and absent phasic activity[74], and additional neurological or hormonal disturbances may be associated with development of functional disturbance[75].
Both types of SOD can lead to pain, recurrent pancreatitis and cholestasis without any apparent etiology, and hence need a high clinical suspicion for diagnosis. Biliary manometry can be utilized to confirm the diagnosis. Selective patients may be managed endoscopically, and ERC with sphincterotomy is usually reserved for patients with dilated bile duct with cholestasis liver chemistries, without any other obvious cause. It is aimed at cutting the sphincter muscles, resulting in reduction of the intra-luminal biliary and pancreatic hypertension, and symptomatic relief. However, the procedure has high risk of post-procedure pancreatitis and usually pancreatic duct stent is placed prophylactically[76]. In case of failure of endoscopic therapy, choledochojejunostomy is the last resort.
Biliary stones, sludge, casts, and blood clots
Biliary stones, sludge, casts, and blood clots are collectively referred to as “Common Bile Duct (CBD) Filling Defects” and can be seen in 3.3%-12.3% of patients after LT[77,78] (Figure 4). Stricture, infection and ischemia can result in biliary stones and sludge; and sloughed biliary epithelium, chronic rejection, infection, and bile stasis, have been associated with formation of biliary casts. They have been postulated to be related to strictures, bacterial infection, mucosal damage and ischemia[78-80]. These patients might present with abdominal pain, cholestatic liver enzyme pattern or may have recurrent episodes of cholangitis and pancreatitis[11]. However, many patients with choledocholithiasis may be completely asymptomatic, which is often attributed to the fact that transplanted graft is denervated, and may also be afebrile because of steroids and immunosuppressant medications they are on post-LT. Occasionally, CBD filling defects may form due to stagnation of bile proximal to a stricture, in which case management becomes challenging (Figure 4). Because of ischemic etiology to biliary cast syndrome, HAT exclusion with appropriate imaging becomes prudent.
Figure 4.
Management of common bile duct filling defects. A: Common bile duct (CBD) filling defect seen proximal to mid-CBD stricture in a post-liver transplantation patient; B: Successful removal of stone after dilatation the stricture; C: Endoscopic image of successfully extracted stone and sludge in this case.
Management: ERC with sphincterotomy has a success rate of 90%-100% in clearing biliary stones and sludge; however removal of biliary casts can be challenging and may require multiple procedures including sphincterotomy, balloon or basket extraction, stent placement and lithotripsy, or may need PTC eventually[77,79]. For removal of biliary casts, endoscopy has shown to successful in 25%-60% of patients across different studies[79,81]. In fact, in cases with severe biliary necrosis and casts, repeated interventions with baskets and dilatations are necessary, and placement of stents is not generally recommended in the early course, for risk of occlusion by biliary debris[82]. On the contrary, biliary duct stones are usually easily removed using ERC with biliary sphincterotomy and balloon sweeps (Figure 4). Occasionally, proximal stones may pose a challenge, and in those cases direct cholangioscopy can be performed to remove biliary stones. Also if filling defect lies proximal to a post-LT stricture, then stricture management becomes first step towards the goal of clearing the duct (Figure 4). Lithotripsy and Holmium Laser can be combined with this procedure for stone dis-impaction. Direct cholangioscopy can be performed using ultra-slim, pediatric endoscopes which can be directly advanced into the bile duct to examine duct anatomy and removal of biliary stones and casts[69]. Again, deep enteroscopy can be utilized to perform ERC in patients with Roux-en-Y anastomosis to remove biliary stones or casts[83].
Mucocele
Mucocele of cystic duct results from collection of mucus from the cells lining the cystic duct remnant, and is an extremely rare entity in post-LT patients. Key to diagnosis is cognizance of this diagnostic possibility in a patient with post-LT obstructive jaundice or cholangitis with no apparent cause, and confirmation with MRCP, which would show an extrinsic mass (fluid collection) compressing the bile or hepatic ducts[84]. Patients usually require surgical or radiological drainage. To prevent this complication, usual operative practice involves either excising the cystic duct, or incorporating the distal end of the transected cystic duct into the suture line of the biliary anastomosis to ensure drainage[85].
Hemobilia
While hemobilia may not be a direct consequence or complication of liver transplant itself, it can happen after liver biopsy or PTC performed in post-LT period for management of various issues. Patients present with abdominal pain, jaundice and gastrointestinal bleeding, and upper endoscopy using regular forward-viewing gastroscope (or side viewing duodenoscope) typically reveals blood extruding from the ampulla. Management goals are hemostasis, as well as confirming clearance of bile duct of any clots, which would otherwise be a source of potential obstruction and cholangitis. Hemostasis may be achieved with a multi-prong strategy of coagulopathy correction, endoscopic therapy with use of epinephrine and electro-cautery if bleeding site is accessible, otherwise localization of bleeding with hepatic artery angiogram followed by embolization of feeding vessel radiologically[86]. Once hemostasis is achieved, clot retrieval and clearance of duct can be achieved with ERC if there is evidence of biliary obstruction. Figure 5 (used with permission from Farshad Aduli, MD) represents a case seen by authors, of post-LT hepatic artery pseudo-aneurysm fistulizing to the common bile duct resulting in hemobilia, which was managed by intravascular stent placement by interventional radiology.
Figure 5.
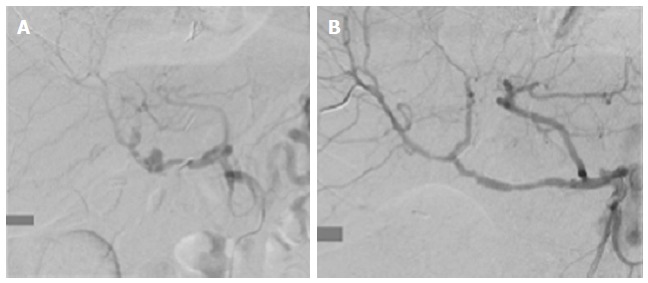
Rare cause of Hemobilia. A: Hepatic artery pseudoaneurysm fistulizing to the common bile duct, resulting in hemobilia; B: Managed with intravascular stent placement by interventional radiology.
SPECIAL ISSUES AFTER LT
Management of biliary complications in patients with Roux-en-Y Hepaticojejunostomy and Roux-en-Y gastric bypass
With the increase in number of liver transplants being performed and limited number of DDLT, there is increase in use of LDLT and split liver transplant strategies. This has resulted in more complex anatomy post-LT. Roux-en-Y Hepaticojejunostomy and Roux-en-Y gastric bypass are the 2 main altered surgical anatomies that are often encountered in post-LT patients. Roux-en-Y gastric bypass creates a common limb of 150 cm and a bilio-pancreatic limb of 150 cm, which makes conventional endoscopy and ERC challenging. Traditional PTC has been utilized for management of post-LT biliary complications in such patients with altered anatomy. However, as mentioned earlier, development of DBE, SBE and spiral enteroscopy has increased the endoscopic options that permit ERC in these patients[51,87,88]. Details of the success of this technique have been discussed earlier. However, it may not be possible to utilize this strategy in all patients, due to unfavorable surgical anatomy, adhesions, limited maneuverability of the scope around biliary anastomosis, and limited number of small-caliber ERC instruments that can be used through these devices. Also, these procedures require high skill and expertise and the learning curve is steep and hence available only at specialized centers. Another specialized technique that is being tried is formation of gastrostomy, either surgically or percutaneously using EUS, and then performing ERC through the gastrostomy port[89]. A single study using this approach achieved biliary intervention successfully in all patients as compared to 58% success rate with deep enteroscopy, and should be evaluated further[90]. Lastly, an alternative approach that may be potentially used in patients with altered anatomy is the use of direct cholangioscopy after percutaneous tract has been created. Direct visualization of bile ducts is possible using this method and can be used for removal of bile duct stones, dilation of stricture and placement of stents.
Biliary complications in recipients of LDLT and DCD transplants
Biliary complications after LT from living donors (LDLT) or grafts from donors after cardiac death (DCD) are more frequent than encountered with conventional donors after brain death (DBD). Complications that occur at a higher rate after LDLT included biliary leak (31.8% vs 10.2%), unplanned re-exploration (26.2% vs 17.1%), HAT (6.5% vs 2.3%) and portal vein thrombosis (2.9% vs 0.0%)[91]. However, there is suggestion that these complications may decrease as experience of LDLT center grows. The main reason for higher biliary complications is relatively smaller duct size, making the anastomosis technically difficult, and hence a higher chance of ischemic injury, especially in right-lobe LDLT[92]. Endoscopic management in LDLT recipients may be challenging given the complex nature of their duct-to-duct reconstruction, especially those involving smaller caliber ducts (< 4 mm), than when a hepatico-jejunostomy is used with these duct sizes. If attempted, smaller diameter stents (7.0-8.5 Fr) need to be used in these scenarios, and ERC performed more regularly because rates of re-stenosis are high with shorter duration of stenting. On the contrary, DCD is commonly associated with significant risk for both early and late biliary complications, including strictures, and many patients develop more than one biliary complication[93]. The major difference between pathogenesis of post-LT NAS in DCD is that the contributing mechanism is ischemic injury, which occurs before organ retrieval, rather than ischemia post-anastomosis in conventional DBD NAS[93]. There is also emerging evidence that the type of preservative solution (HTK solution) may also affect future incidence of biliary complications in DCD patients[94]. The endoscopic management principles remain the same, although intra-hepatic and small duct strictures may be more common making them less amenable to endoscopic management. There is evidence that although unilateral and easily approachable strictures may be managed endoscopically (with > 85% long-term survival), most DCD patients have diffuse intrahepatic structuring disease, due to global organ ischemia, which negatively impacts their long-term survival[95].
Sedation for ERC in post-LT patients
The sedation regimen for ERC in non-transplant setting may vary based on country, type of practice, endoscopist preference, age and co-morbidities of patient, and availability of anesthesia support. Conscious sedation (using opioids and/or benzodiazepines) is being increasingly less preferred for ERC, because it is long and uncomfortable procedure, and adequate patient relaxation and sedation is vital for the success of this critical procedure. Data suggests that propofol is superior to benzodiazepines for sedation during an ERC procedure, even in high-risk octogenarians[96]. Further studies proved that the combined use of propofol and midazolam or fentanyl for sedation has some benefits and no safety concerns, compared to using either drug alone[97]. There are adequate safety results for the administration of propofol by nonanesthesiologists[98]. For these reasons, at our center, like most of the other hospitals in the United States, ERC’s are usually performed under anesthetist administered general anesthesia or monitored anesthesia care using propofol. Safety of opioids/benzodiazepines as well as propofol based regimens have been adequately demonstrated for GI endoscopic procedures, in several studies[99,100]. However, there is no such data available in post-LT patients, and is an area for further research. Nevertheless, in our experience of performing ERC’s on post-LT patients over the last 6 years, we have not encountered any sedation related complication, and we attribute that to proper patient selection and careful optimization of patient co-morbidities before embarking on this critical procedure. Based on our experience, we endorse anesthetist administered anesthesia as a routine sedation strategy for all post-transplant patients requiring ERC, taking into consideration the overall high-risk nature and length of this procedure, frequent need for multiple therapeutic interventions and patient co-morbidities.
CONCLUSION
Biliary complications are being increasingly encountered in post liver transplant patients because of increased volume of transplants being done and longer survival of these recipients. Overall management of these complications may be challenging, but with advances in endoscopic techniques, majority of such patients are being dealt with by endoscopists rather than the surgeons. ERC with various interventions, like sphincterotomy, bile duct dilatation, and stent placement, remains the mainstay for management of bile leaks, strictures and bile duct filling defects. Recurrence of native disease is the greatest mimicker of post-LT biliary complications, and hence must be investigated thoroughly with advanced imaging or endoscopic means (Figure 6). With increasing number of patients with altered anatomy, whether due to obesity epidemic or use of non-traditional anastomoses in liver transplant strategies like living-donor or split livers, ERC in these patients has been a perplexing issue and many require interventional radiology or surgical procedures. However, with ongoing attempts at developing improved tools and techniques to access the bile duct in patients with surgically altered anatomy, endoscopy will likely become unopposed frontier in this subgroup of patients as well.
Figure 6.
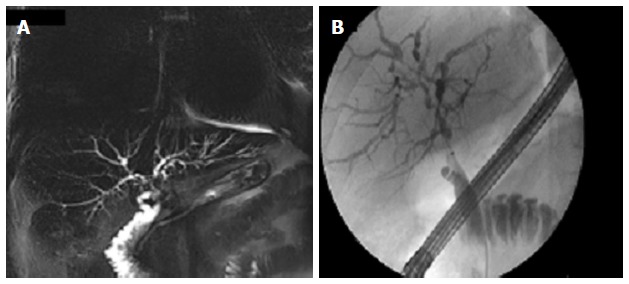
Don’t forget the native disease. Recurrence of native disease can mimic biliary complications, hence appropriately investigated with magnetic resonance cholangiopancreatography (A) and/or endoscopic retrograde cholangiography (B). This patient was transplanted for primary sclerosing cholangitis, and had disease recurrence involving the intra-hepatics few years later.
Footnotes
Conflict-of-interest: None.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: October 1, 2014
First decision: October 28, 2014
Article in press: February 9, 2015
P- Reviewer: Chiu KW, Eysselein VE, Jonaitis L, Kapetanos D, Xu CF S- Editor: Song XX L- Editor: A E- Editor: Wu HL
References
- 1.Calne RY, McMaster P, Portmann B, Wall WJ, Williams R. Observations on preservation, bile drainage and rejection in 64 human orthotopic liver allografts. Ann Surg. 1977;186:282–290. doi: 10.1097/00000658-197709000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ayoub WS, Esquivel CO, Martin P. Biliary complications following liver transplantation. Dig Dis Sci. 2010;55:1540–1546. doi: 10.1007/s10620-010-1217-2. [DOI] [PubMed] [Google Scholar]
- 3.Seehofer D, Eurich D, Veltzke-Schlieker W, Neuhaus P. Biliary complications after liver transplantation: old problems and new challenges. Am J Transplant. 2013;13:253–265. doi: 10.1111/ajt.12034. [DOI] [PubMed] [Google Scholar]
- 4.Wojcicki M, Milkiewicz P, Silva M. Biliary tract complications after liver transplantation: a review. Dig Surg. 2008;25:245–257. doi: 10.1159/000144653. [DOI] [PubMed] [Google Scholar]
- 5.Jagannath S, Kalloo AN. Biliary Complications After Liver Transplantation. Curr Treat Options Gastroenterol. 2002;5:101–112. doi: 10.1007/s11938-002-0057-3. [DOI] [PubMed] [Google Scholar]
- 6.Sharma S, Gurakar A, Jabbour N. Biliary strictures following liver transplantation: past, present and preventive strategies. Liver Transpl. 2008;14:759–769. doi: 10.1002/lt.21509. [DOI] [PubMed] [Google Scholar]
- 7.Kitazono MT, Qayyum A, Yeh BM, Chard PS, Ostroff JW, Coakley FV. Magnetic resonance cholangiography of biliary strictures after liver transplantation: a prospective double-blind study. J Magn Reson Imaging. 2007;25:1168–1173. doi: 10.1002/jmri.20927. [DOI] [PubMed] [Google Scholar]
- 8.Akamatsu N, Sugawara Y, Hashimoto D. Biliary reconstruction, its complications and management of biliary complications after adult liver transplantation: a systematic review of the incidence, risk factors and outcome. Transpl Int. 2011;24:379–392. doi: 10.1111/j.1432-2277.2010.01202.x. [DOI] [PubMed] [Google Scholar]
- 9.Yazumi S, Chiba T. Biliary complications after a right-lobe living donor liver transplantation. J Gastroenterol. 2005;40:861–865. doi: 10.1007/s00535-005-1698-5. [DOI] [PubMed] [Google Scholar]
- 10.Saidi RF, Elias N, Ko DS, Kawai T, Markmann J, Cosimi AB, Hertl M. Biliary reconstruction and complications after living-donor liver transplantation. HPB (Oxford) 2009;11:505–509. doi: 10.1111/j.1477-2574.2009.00093.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Safdar K, Atiq M, Stewart C, Freeman ML. Biliary tract complications after liver transplantation. Expert Rev Gastroenterol Hepatol. 2009;3:183–195. doi: 10.1586/egh.09.4. [DOI] [PubMed] [Google Scholar]
- 12.Vit A, De Candia A, Como G, Del Frate C, Marzio A, Bazzocchi M. Doppler evaluation of arterial complications of adult orthotopic liver transplantation. J Clin Ultrasound. 2003;31:339–345. doi: 10.1002/jcu.10190. [DOI] [PubMed] [Google Scholar]
- 13.Kok T, Van der Sluis A, Klein JP, Van der Jagt EJ, Peeters PM, Slooff MJ, Bijleveld CM, Haagsma EB. Ultrasound and cholangiography for the diagnosis of biliary complications after orthotopic liver transplantation: a comparative study. J Clin Ultrasound. 1996;24:103–115. doi: 10.1002/(SICI)1097-0096(199603)24:3<103::AID-JCU1>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 14.Beswick DM, Miraglia R, Caruso S, Marrone G, Gruttadauria S, Zajko AB, Luca A. The role of ultrasound and magnetic resonance cholangiopancreatography for the diagnosis of biliary stricture after liver transplantation. Eur J Radiol. 2012;81:2089–2092. doi: 10.1016/j.ejrad.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 15.Katz LH, Benjaminov O, Belinki A, Geler A, Braun M, Knizhnik M, Aizner S, Shaharabani E, Sulkes J, Shabtai E, et al. Magnetic resonance cholangiopancreatography for the accurate diagnosis of biliary complications after liver transplantation: comparison with endoscopic retrograde cholangiography and percutaneous transhepatic cholangiography - long-term follow-up. Clin Transplant. 2010;24:E163–E169. doi: 10.1111/j.1399-0012.2010.01300.x. [DOI] [PubMed] [Google Scholar]
- 16.Rösch T, Meining A, Frühmorgen S, Zillinger C, Schusdziarra V, Hellerhoff K, Classen M, Helmberger H. A prospective comparison of the diagnostic accuracy of ERCP, MRCP, CT, and EUS in biliary strictures. Gastrointest Endosc. 2002;55:870–876. doi: 10.1067/mge.2002.124206. [DOI] [PubMed] [Google Scholar]
- 17.Taylor AC, Little AF, Hennessy OF, Banting SW, Smith PJ, Desmond PV. Prospective assessment of magnetic resonance cholangiopancreatography for noninvasive imaging of the biliary tree. Gastrointest Endosc. 2002;55:17–22. doi: 10.1067/mge.2002.120324. [DOI] [PubMed] [Google Scholar]
- 18.Pecchi A, De Santis M, Gibertini MC, Tarantino G, Gerunda GE, Torricelli P, Di Benedetto F. Role of magnetic resonance imaging in the detection of anastomotic biliary strictures after liver transplantation. Transplant Proc. 2011;43:1132–1135. doi: 10.1016/j.transproceed.2011.03.016. [DOI] [PubMed] [Google Scholar]
- 19.Jorgensen JE, Waljee AK, Volk ML, Sonnenday CJ, Elta GH, Al-Hawary MM, Singal AG, Taylor JR, Elmunzer BJ. Is MRCP equivalent to ERCP for diagnosing biliary obstruction in orthotopic liver transplant recipients? A meta-analysis. Gastrointest Endosc. 2011;73:955–962. doi: 10.1016/j.gie.2010.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kinner S, Dechêne A, Paul A, Umutlu L, Ladd SC, de Dechêne EM, Zöpf T, Gerken G, Lauenstein TC. Detection of biliary stenoses in patients after liver transplantation: is there a different diagnostic accuracy of MRCP depending on the type of biliary anastomosis? Eur J Radiol. 2011;80:e20–e28. doi: 10.1016/j.ejrad.2010.06.003. [DOI] [PubMed] [Google Scholar]
- 21.Colonna JO, Shaked A, Gomes AS, Colquhoun SD, Jurim O, McDiarmid SV, Millis JM, Goldstein LI, Busuttil RW. Biliary strictures complicating liver transplantation. Incidence, pathogenesis, management, and outcome. Ann Surg. 1992;216:344–450; discussion 350-452. doi: 10.1097/00000658-199209000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tabibian JH, Girotra M, Yeh HC, Segev DL, Gulsen MT, Cengiz-Seval G, Singh VK, Cameron AM, Gurakar A. Sirolimus based immunosuppression is associated with need for early repeat therapeutic ERCP in liver transplant patients with anastomotic biliary stricture. Ann Hepatol. 2013;12:563–569. [PubMed] [Google Scholar]
- 23.Guichelaar MM, Benson JT, Malinchoc M, Krom RA, Wiesner RH, Charlton MR. Risk factors for and clinical course of non-anastomotic biliary strictures after liver transplantation. Am J Transplant. 2003;3:885–890. doi: 10.1034/j.1600-6143.2003.00165.x. [DOI] [PubMed] [Google Scholar]
- 24.Pascher A, Neuhaus P. Bile duct complications after liver transplantation. Transpl Int. 2005;18:627–642. doi: 10.1111/j.1432-2277.2005.00123.x. [DOI] [PubMed] [Google Scholar]
- 25.Verdonk RC, Buis CI, Porte RJ, van der Jagt EJ, Limburg AJ, van den Berg AP, Slooff MJ, Peeters PM, de Jong KP, Kleibeuker JH, et al. Anastomotic biliary strictures after liver transplantation: causes and consequences. Liver Transpl. 2006;12:726–735. doi: 10.1002/lt.20714. [DOI] [PubMed] [Google Scholar]
- 26.Theilmann L, Küppers B, Kadmon M, Roeren T, Notheisen H, Stiehl A, Otto G. Biliary tract strictures after orthotopic liver transplantation: diagnosis and management. Endoscopy. 1994;26:517–522. doi: 10.1055/s-2007-1009026. [DOI] [PubMed] [Google Scholar]
- 27.Buis CI, Verdonk RC, Van der Jagt EJ, van der Hilst CS, Slooff MJ, Haagsma EB, Porte RJ. Nonanastomotic biliary strictures after liver transplantation, part 1: Radiological features and risk factors for early vs. late presentation. Liver Transpl. 2007;13:708–718. doi: 10.1002/lt.21166. [DOI] [PubMed] [Google Scholar]
- 28.Verdonk RC, Buis CI, van der Jagt EJ, Gouw AS, Limburg AJ, Slooff MJ, Kleibeuker JH, Porte RJ, Haagsma EB. Nonanastomotic biliary strictures after liver transplantation, part 2: Management, outcome, and risk factors for disease progression. Liver Transpl. 2007;13:725–732. doi: 10.1002/lt.21165. [DOI] [PubMed] [Google Scholar]
- 29.Akay S, Karasu Z, Ersöz G, Kiliç M, Akyildiz M, Günşar F, Akarca U, Batur Y, Ilter T. Results of endoscopic management of anastomotic biliary strictures after orthotopic liver transplantation. Turk J Gastroenterol. 2006;17:159–163. [PubMed] [Google Scholar]
- 30.Rossi AF, Grosso C, Zanasi G, Gambitta P, Bini M, De Carlis L, Rondinara G, Arcidiacono R. Long-term efficacy of endoscopic stenting in patients with stricture of the biliary anastomosis after orthotopic liver transplantation. Endoscopy. 1998;30:360–366. doi: 10.1055/s-2007-1001283. [DOI] [PubMed] [Google Scholar]
- 31.Mahajani RV, Cotler SJ, Uzer MF. Efficacy of endoscopic management of anastomotic biliary strictures after hepatic transplantation. Endoscopy. 2000;32:943–949. doi: 10.1055/s-2000-9619. [DOI] [PubMed] [Google Scholar]
- 32.Schwartz DA, Petersen BT, Poterucha JJ, Gostout CJ. Endoscopic therapy of anastomotic bile duct strictures occurring after liver transplantation. Gastrointest Endosc. 2000;51:169–174. doi: 10.1016/s0016-5107(00)70413-5. [DOI] [PubMed] [Google Scholar]
- 33.Zoepf T, Maldonado-Lopez EJ, Hilgard P, Malago M, Broelsch CE, Treichel U, Gerken G. Balloon dilatation vs. balloon dilatation plus bile duct endoprostheses for treatment of anastomotic biliary strictures after liver transplantation. Liver Transpl. 2006;12:88–94. doi: 10.1002/lt.20548. [DOI] [PubMed] [Google Scholar]
- 34.Kulaksiz H, Weiss KH, Gotthardt D, Adler G, Stremmel W, Schaible A, Dogan A, Stiehl A, Sauer P. Is stenting necessary after balloon dilation of post-transplantation biliary strictures? Results of a prospective comparative study. Endoscopy. 2008;40:746–751. doi: 10.1055/s-2008-1077489. [DOI] [PubMed] [Google Scholar]
- 35.Alazmi WM, Fogel EL, Watkins JL, McHenry L, Tector JA, Fridell J, Mosler P, Sherman S, Lehman GA. Recurrence rate of anastomotic biliary strictures in patients who have had previous successful endoscopic therapy for anastomotic narrowing after orthotopic liver transplantation. Endoscopy. 2006;38:571–574. doi: 10.1055/s-2006-925027. [DOI] [PubMed] [Google Scholar]
- 36.Rerknimitr R, Sherman S, Fogel EL, Kalayci C, Lumeng L, Chalasani N, Kwo P, Lehman GA. Biliary tract complications after orthotopic liver transplantation with choledochocholedochostomy anastomosis: endoscopic findings and results of therapy. Gastrointest Endosc. 2002;55:224–231. doi: 10.1067/mge.2002.120813. [DOI] [PubMed] [Google Scholar]
- 37.Elmi F, Silverman WB. Outcome of ERCP in the management of duct-to-duct anastomotic strictures in orthotopic liver transplant. Dig Dis Sci. 2007;52:2346–2350. doi: 10.1007/s10620-006-9142-0. [DOI] [PubMed] [Google Scholar]
- 38.Morelli J, Mulcahy HE, Willner IR, Cunningham JT, Draganov P. Long-term outcomes for patients with post-liver transplant anastomotic biliary strictures treated by endoscopic stent placement. Gastrointest Endosc. 2003;58:374–379. doi: 10.1067/s0016-5107(03)00011-7. [DOI] [PubMed] [Google Scholar]
- 39.Kim TH, Lee SK, Han JH, Park do H, Lee SS, Seo DW, Kim MH, Song GW, Ha TY, Kim KH, et al. The role of endoscopic retrograde cholangiography for biliary stricture after adult living donor liver transplantation: technical aspect and outcome. Scand J Gastroenterol. 2011;46:188–196. doi: 10.3109/00365521.2010.522722. [DOI] [PubMed] [Google Scholar]
- 40.Tsujino T, Isayama H, Sugawara Y, Sasaki T, Kogure H, Nakai Y, Yamamoto N, Sasahira N, Yamashiki N, Tada M, et al. Endoscopic management of biliary complications after adult living donor liver transplantation. Am J Gastroenterol. 2006;101:2230–2236. doi: 10.1111/j.1572-0241.2006.00797.x. [DOI] [PubMed] [Google Scholar]
- 41.Holt AP, Thorburn D, Mirza D, Gunson B, Wong T, Haydon G. A prospective study of standardized nonsurgical therapy in the management of biliary anastomotic strictures complicating liver transplantation. Transplantation. 2007;84:857–863. doi: 10.1097/01.tp.0000282805.33658.ce. [DOI] [PubMed] [Google Scholar]
- 42.Costamagna G, Pandolfi M, Mutignani M, Spada C, Perri V. Long-term results of endoscopic management of postoperative bile duct strictures with increasing numbers of stents. Gastrointest Endosc. 2001;54:162–168. doi: 10.1067/mge.2001.116876. [DOI] [PubMed] [Google Scholar]
- 43.Tabibian JH, Asham EH, Han S, Saab S, Tong MJ, Goldstein L, Busuttil RW, Durazo FA. Endoscopic treatment of postorthotopic liver transplantation anastomotic biliary strictures with maximal stent therapy (with video) Gastrointest Endosc. 2010;71:505–512. doi: 10.1016/j.gie.2009.10.023. [DOI] [PubMed] [Google Scholar]
- 44.Vitale GC, Larson GM, George M, Tatum C. Management of malignant biliary stricture with self-expanding metallic stent. Surg Endosc. 1996;10:970–973. doi: 10.1007/s004649900216. [DOI] [PubMed] [Google Scholar]
- 45.Vandenbroucke F, Plasse M, Dagenais M, Lapointe R, Lêtourneau R, Roy A. Treatment of post liver transplantation bile duct stricture with self-expandable metallic stent. HPB (Oxford) 2006;8:202–205. doi: 10.1080/13651820500501800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tee HP, James MW, Kaffes AJ. Placement of removable metal biliary stent in post-orthotopic liver transplantation anastomotic stricture. World J Gastroenterol. 2010;16:3597–3600. doi: 10.3748/wjg.v16.i28.3597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kao D, Zepeda-Gomez S, Tandon P, Bain VG. Managing the post-liver transplantation anastomotic biliary stricture: multiple plastic versus metal stents: a systematic review. Gastrointest Endosc. 2013;77:679–691. doi: 10.1016/j.gie.2013.01.015. [DOI] [PubMed] [Google Scholar]
- 48.Rizk RS, McVicar JP, Emond MJ, Rohrmann CA, Kowdley KV, Perkins J, Carithers RL, Kimmey MB. Endoscopic management of biliary strictures in liver transplant recipients: effect on patient and graft survival. Gastrointest Endosc. 1998;47:128–135. doi: 10.1016/s0016-5107(98)70344-x. [DOI] [PubMed] [Google Scholar]
- 49.Haruta H, Yamamoto H, Mizuta K, Kita Y, Uno T, Egami S, Hishikawa S, Sugano K, Kawarasaki H. A case of successful enteroscopic balloon dilation for late anastomotic stricture of choledochojejunostomy after living donor liver transplantation. Liver Transpl. 2005;11:1608–1610. doi: 10.1002/lt.20623. [DOI] [PubMed] [Google Scholar]
- 50.Sanada Y, Mizuta K, Yano T, Hatanaka W, Okada N, Wakiya T, Umehara M, Egami S, Urahashi T, Hishikawa S, et al. Double-balloon enteroscopy for bilioenteric anastomotic stricture after pediatric living donor liver transplantation. Transpl Int. 2011;24:85–90. doi: 10.1111/j.1432-2277.2010.01156.x. [DOI] [PubMed] [Google Scholar]
- 51.Shah RJ, Smolkin M, Yen R, Ross A, Kozarek RA, Howell DA, Bakis G, Jonnalagadda SS, Al-Lehibi AA, Hardy A, et al. A multicenter, U.S. experience of single-balloon, double-balloon, and rotational overtube-assisted enteroscopy ERCP in patients with surgically altered pancreaticobiliary anatomy (with video) Gastrointest Endosc. 2013;77:593–600. doi: 10.1016/j.gie.2012.10.015. [DOI] [PubMed] [Google Scholar]
- 52.Laasch HU, Tringali A, Wilbraham L, Marriott A, England RE, Mutignani M, Perri V, Costamagna G, Martin DF. Comparison of standard and steerable catheters for bile duct cannulation in ERCP. Endoscopy. 2003;35:669–674. doi: 10.1055/s-2003-41515. [DOI] [PubMed] [Google Scholar]
- 53.Gürakar A, Wright H, Camci C, Jaboour N. The application of SpyScope® technology in evaluation of pre and post liver transplant biliary problems. Turk J Gastroenterol. 2010;21:428–432. doi: 10.4318/tjg.2010.0131. [DOI] [PubMed] [Google Scholar]
- 54.Petersen BT. Cholangioscopy for special applications: primary sclerosing cholangitis, liver transplant, and selective duct access. Gastrointest Endosc Clin N Am. 2009;19:579–586. doi: 10.1016/j.giec.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 55.Parsi MA, Guardino J, Vargo JJ. Peroral cholangioscopy-guided stricture therapy in living donor liver transplantation. Liver Transpl. 2009;15:263–265. doi: 10.1002/lt.21584. [DOI] [PubMed] [Google Scholar]
- 56.Wright H, Sharma S, Gurakar A, Sebastian A, Kohli V, Jabbour N. Management of biliary stricture guided by the Spyglass Direct Visualization System in a liver transplant recipient: an innovative approach. Gastrointest Endosc. 2008;67:1201–1203. doi: 10.1016/j.gie.2007.10.055. [DOI] [PubMed] [Google Scholar]
- 57.Siddique I, Galati J, Ankoma-Sey V, Wood RP, Ozaki C, Monsour H, Raijman I. The role of choledochoscopy in the diagnosis and management of biliary tract diseases. Gastrointest Endosc. 1999;50:67–73. doi: 10.1016/s0016-5107(99)70347-0. [DOI] [PubMed] [Google Scholar]
- 58.Balderramo D, Sendino O, Miquel R, de Miguel CR, Bordas JM, Martinez-Palli G, Leoz ML, Rimola A, Navasa M, Llach J, et al. Prospective evaluation of single-operator peroral cholangioscopy in liver transplant recipients requiring an evaluation of the biliary tract. Liver Transpl. 2013;19:199–206. doi: 10.1002/lt.23585. [DOI] [PubMed] [Google Scholar]
- 59.Cennamo V, Luigiano C, Fabbri C, Maimone A, Bazzoli F, Ceroni L, Morace C, Jovine E. Cholangioscopy using a new type of cholangioscope for the diagnosis of biliary tract disease: a case series. Endoscopy. 2012;44:878–881. doi: 10.1055/s-0032-1310016. [DOI] [PubMed] [Google Scholar]
- 60.Hoffman A, Kiesslich R, Moench C, Bittinger F, Otto G, Galle PR, Neurath MF. Methylene blue-aided cholangioscopy unravels the endoscopic features of ischemic-type biliary lesions after liver transplantation. Gastrointest Endosc. 2007;66:1052–1058. doi: 10.1016/j.gie.2007.04.022. [DOI] [PubMed] [Google Scholar]
- 61.Kim ES, Lee BJ, Won JY, Choi JY, Lee DK. Percutaneous transhepatic biliary drainage may serve as a successful rescue procedure in failed cases of endoscopic therapy for a post-living donor liver transplantation biliary stricture. Gastrointest Endosc. 2009;69:38–46. doi: 10.1016/j.gie.2008.03.1113. [DOI] [PubMed] [Google Scholar]
- 62.Thuluvath PJ, Pfau PR, Kimmey MB, Ginsberg GG. Biliary complications after liver transplantation: the role of endoscopy. Endoscopy. 2005;37:857–863. doi: 10.1055/s-2005-870192. [DOI] [PubMed] [Google Scholar]
- 63.Sheng R, Sammon JK, Zajko AB, Campbell WL. Bile leak after hepatic transplantation: cholangiographic features, prevalence, and clinical outcome. Radiology. 1994;192:413–416. doi: 10.1148/radiology.192.2.8029406. [DOI] [PubMed] [Google Scholar]
- 64.Sundaram V, Jones DT, Shah NH, de Vera ME, Fontes P, Marsh JW, Humar A, Ahmad J. Posttransplant biliary complications in the pre- and post-model for end-stage liver disease era. Liver Transpl. 2011;17:428–435. doi: 10.1002/lt.22251. [DOI] [PubMed] [Google Scholar]
- 65.Thuluvath PJ, Atassi T, Lee J. An endoscopic approach to biliary complications following orthotopic liver transplantation. Liver Int. 2003;23:156–162. doi: 10.1034/j.1600-0676.2003.00823.x. [DOI] [PubMed] [Google Scholar]
- 66.Greif F, Bronsther OL, Van Thiel DH, Casavilla A, Iwatsuki S, Tzakis A, Todo S, Fung JJ, Starzl TE. The incidence, timing, and management of biliary tract complications after orthotopic liver transplantation. Ann Surg. 1994;219:40–45. doi: 10.1097/00000658-199401000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Scanga AE, Kowdley KV. Management of biliary complications following orthotopic liver transplantation. Curr Gastroenterol Rep. 2007;9:31–38. doi: 10.1007/s11894-008-0018-7. [DOI] [PubMed] [Google Scholar]
- 68.Shuhart MC, Kowdley KV, McVicar JP, Rohrmann CA, McDonald MF, Wadland DW, Emerson SS, Carithers RL, Kimmey MB. Predictors of bile leaks after T-tube removal in orthotopic liver transplant recipients. Liver Transpl Surg. 1998;4:62–70. doi: 10.1002/lt.500040109. [DOI] [PubMed] [Google Scholar]
- 69.Arain MA, Attam R, Freeman ML. Advances in endoscopic management of biliary tract complications after liver transplantation. Liver Transpl. 2013;19:482–498. doi: 10.1002/lt.23624. [DOI] [PubMed] [Google Scholar]
- 70.Solmi L, Cariani G, Leo P, Miracolo A, Nigro G, Roda E. Results of endoscopic retrograde cholangiopancreatography in the treatment of biliary tract complications after orthotopic liver transplantation: our experience. Hepatogastroenterology. 2007;54:1004–1008. [PubMed] [Google Scholar]
- 71.Krok KL, Cárdenas A, Thuluvath PJ. Endoscopic management of biliary complications after liver transplantation. Clin Liver Dis. 2010;14:359–371. doi: 10.1016/j.cld.2010.03.008. [DOI] [PubMed] [Google Scholar]
- 72.Saab S, Martin P, Soliman GY, Machicado GA, Roth BE, Kunder G, Han SH, Farmer DG, Ghobrial RM, Busuttil RW, et al. Endoscopic management of biliary leaks after T-tube removal in liver transplant recipients: nasobiliary drainage versus biliary stenting. Liver Transpl. 2000;6:627–632. doi: 10.1053/jlts.2000.8200. [DOI] [PubMed] [Google Scholar]
- 73.Llach J, Bordas JM, Elizalde JI, Enrico C, Ginès A, Pellisé M, Mondelo F, Piqué JM. Sphincterotomy in the treatment of biliary leakage. Hepatogastroenterology. 2002;49:1496–1498. [PubMed] [Google Scholar]
- 74.Douzdjian V, Abecassis MM, Johlin FC. Sphincter of Oddi dysfunction following liver transplantation. Screening by bedside manometry and definitive manometric evaluation. Dig Dis Sci. 1994;39:253–256. doi: 10.1007/BF02090194. [DOI] [PubMed] [Google Scholar]
- 75.Londoño MC, Balderramo D, Cárdenas A. Management of biliary complications after orthotopic liver transplantation: the role of endoscopy. World J Gastroenterol. 2008;14:493–497. doi: 10.3748/wjg.14.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Freeman ML. Pancreatic stents for prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis. Clin Gastroenterol Hepatol. 2007;5:1354–1365. doi: 10.1016/j.cgh.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 77.Park JS, Kim MH, Lee SK, Seo DW, Lee SS, Han J, Min YI, Hwang S, Park KM, Lee YJ, et al. Efficacy of endoscopic and percutaneous treatments for biliary complications after cadaveric and living donor liver transplantation. Gastrointest Endosc. 2003;57:78–85. doi: 10.1067/mge.2003.11. [DOI] [PubMed] [Google Scholar]
- 78.Sheng R, Ramirez CB, Zajko AB, Campbell WL. Biliary stones and sludge in liver transplant patients: a 13-year experience. Radiology. 1996;198:243–247. doi: 10.1148/radiology.198.1.8539387. [DOI] [PubMed] [Google Scholar]
- 79.Shah JN, Haigh WG, Lee SP, Lucey MR, Brensinger CM, Kochman ML, Long WB, Olthoff K, Shaked A, Ginsberg GG. Biliary casts after orthotopic liver transplantation: clinical factors, treatment, biochemical analysis. Am J Gastroenterol. 2003;98:1861–1867. doi: 10.1111/j.1572-0241.2003.07617.x. [DOI] [PubMed] [Google Scholar]
- 80.Yang YL, Shi LJ, Lin MJ, Zhang HW, Li JY. Clinical analysis and significance of cholangiography for biliary cast/stone after orthotopic liver transplantation. J Nanosci Nanotechnol. 2013;13:171–177. doi: 10.1166/jnn.2013.6790. [DOI] [PubMed] [Google Scholar]
- 81.Pfau PR, Kochman ML, Lewis JD, Long WB, Lucey MR, Olthoff K, Shaked A, Ginsberg GG. Endoscopic management of postoperative biliary complications in orthotopic liver transplantation. Gastrointest Endosc. 2000;52:55–63. doi: 10.1067/mge.2000.106687. [DOI] [PubMed] [Google Scholar]
- 82.Buxbaum JL, Biggins SW, Bagatelos KC, Ostroff JW. Predictors of endoscopic treatment outcomes in the management of biliary problems after liver transplantation at a high-volume academic center. Gastrointest Endosc. 2011;73:37–44. doi: 10.1016/j.gie.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 83.Saleem A, Baron TH. Successful endoscopic treatment of biliary cast syndrome in an orthotopic liver transplant patient with a Roux-en-Y anastomosis via balloon enteroscopy. Liver Transpl. 2010;16:527–529. doi: 10.1002/lt.22007. [DOI] [PubMed] [Google Scholar]
- 84.Zajko AB, Bennett MJ, Campbell WL, Koneru B. Mucocele of the cystic duct remnant in eight liver transplant recipients: findings at cholangiography, CT, and US. Radiology. 1990;177:691–693. doi: 10.1148/radiology.177.3.2243970. [DOI] [PubMed] [Google Scholar]
- 85.Chatterjee S, Das D, Hudson M, Bassendine MF, Scott J, Oppong KE, Sen G, French JJ. Mucocele of the cystic duct remnant after orthotopic liver transplant: a problem revisited. Exp Clin Transplant. 2011;9:214–216. [PubMed] [Google Scholar]
- 86.Parsi MA. Hemobilia: endoscopic, fluoroscopic, and cholangioscopic diagnosis. Hepatology. 2010;52:2237–2238. doi: 10.1002/hep.23948. [DOI] [PubMed] [Google Scholar]
- 87.Lennon AM, Kapoor S, Khashab M, Corless E, Amateau S, Dunbar K, Chandrasekhara V, Singh V, Okolo PI. Spiral assisted ERCP is equivalent to single balloon assisted ERCP in patients with Roux-en-Y anatomy. Dig Dis Sci. 2012;57:1391–1398. doi: 10.1007/s10620-011-2000-8. [DOI] [PubMed] [Google Scholar]
- 88.Saleem A, Levy MJ, Petersen BT, Que FG, Baron TH. Laparoscopic assisted ERCP in Roux-en-Y gastric bypass (RYGB) surgery patients. J Gastrointest Surg. 2012;16:203–208. doi: 10.1007/s11605-011-1760-y. [DOI] [PubMed] [Google Scholar]
- 89.Attam R, Leslie D, Freeman M, Ikramuddin S, Andrade R. EUS-assisted, fluoroscopically guided gastrostomy tube placement in patients with Roux-en-Y gastric bypass: a novel technique for access to the gastric remnant. Gastrointest Endosc. 2011;74:677–682. doi: 10.1016/j.gie.2011.05.018. [DOI] [PubMed] [Google Scholar]
- 90.Schreiner MA, Chang L, Gluck M, Irani S, Gan SI, Brandabur JJ, Thirlby R, Moonka R, Kozarek RA, Ross AS. Laparoscopy-assisted versus balloon enteroscopy-assisted ERCP in bariatric post-Roux-en-Y gastric bypass patients. Gastrointest Endosc. 2012;75:748–756. doi: 10.1016/j.gie.2011.11.019. [DOI] [PubMed] [Google Scholar]
- 91.Freise CE, Gillespie BW, Koffron AJ, Lok AS, Pruett TL, Emond JC, Fair JH, Fisher RA, Olthoff KM, Trotter JF, et al. Recipient morbidity after living and deceased donor liver transplantation: findings from the A2ALL Retrospective Cohort Study. Am J Transplant. 2008;8:2569–2579. doi: 10.1111/j.1600-6143.2008.02440.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gondolesi GE, Varotti G, Florman SS, Muñoz L, Fishbein TM, Emre SH, Schwartz ME, Miller C. Biliary complications in 96 consecutive right lobe living donor transplant recipients. Transplantation. 2004;77:1842–1848. doi: 10.1097/01.tp.0000123077.78702.0c. [DOI] [PubMed] [Google Scholar]
- 93.Maheshwari A, Maley W, Li Z, Thuluvath PJ. Biliary complications and outcomes of liver transplantation from donors after cardiac death. Liver Transpl. 2007;13:1645–1653. doi: 10.1002/lt.21212. [DOI] [PubMed] [Google Scholar]
- 94.Gulsen MT, Girotra M, Cengiz-Seval G, Price J, Singh VK, Segev DL, Cameron AM, Gurakar A. HTK preservative solution is associated with increased biliary complications among patients receiving DCD liver transplants: a single center experience. Ann Transplant. 2013;18:69–75. doi: 10.12659/AOT.883831. [DOI] [PubMed] [Google Scholar]
- 95.Fung JJ, Eghtesad B, Patel-Tom K. Using livers from donation after cardiac death donors--a proposal to protect the true Achilles heel. Liver Transpl. 2007;13:1633–1636. doi: 10.1002/lt.21388. [DOI] [PubMed] [Google Scholar]
- 96.Riphaus A, Stergiou N, Wehrmann T. Sedation with propofol for routine ERCP in high-risk octogenarians: a randomized, controlled study. Am J Gastroenterol. 2005;100:1957–1963. doi: 10.1111/j.1572-0241.2005.41672.x. [DOI] [PubMed] [Google Scholar]
- 97.VanNatta ME, Rex DK. Propofol alone titrated to deep sedation versus propofol in combination with opioids and/or benzodiazepines and titrated to moderate sedation for colonoscopy. Am J Gastroenterol. 2006;101:2209–2217. doi: 10.1111/j.1572-0241.2006.00760.x. [DOI] [PubMed] [Google Scholar]
- 98.Rex DK, Deenadayalu VP, Eid E, Imperiale TF, Walker JA, Sandhu K, Clarke AC, Hillman LC, Horiuchi A, Cohen LB, et al. Endoscopist-directed administration of propofol: a worldwide safety experience. Gastroenterology. 2009;137:1229–1237; quiz 1518-1519. doi: 10.1053/j.gastro.2009.06.042. [DOI] [PubMed] [Google Scholar]
- 99.Correia LM, Bonilha DQ, Gomes GF, Brito JR, Nakao FS, Lenz L, Rohr MR, Ferrari AP, Libera ED. Sedation during upper GI endoscopy in cirrhotic outpatients: a randomized, controlled trial comparing propofol and fentanyl with midazolam and fentanyl. Gastrointest Endosc. 2011;73:45–51, 51.e1. doi: 10.1016/j.gie.2010.09.025. [DOI] [PubMed] [Google Scholar]
- 100.Fagà E, De Cento M, Giordanino C, Barletti C, Bruno M, Carucci P, De Angelis C, Venon WD, Musso A, Reggio D, et al. Safety of propofol in cirrhotic patients undergoing colonoscopy and endoscopic retrograde cholangiography: results of a prospective controlled study. Eur J Gastroenterol Hepatol. 2012;24:70–76. doi: 10.1097/MEG.0b013e32834c16ab. [DOI] [PubMed] [Google Scholar]


