Abstract
AIM: To evaluate the association between patient disease knowledge of inflammatory bowel disease (IBD) and health related quality of life (HRQoL) and identify patient and disease related predictors of patient knowledge of IBD.
METHODS: We performed a cross-sectional study of IBD patients with an established diagnosis of IBD longer than 3 mo prior to enrollment. The Crohn’s and colitis knowledge score (CCKNOW) and short inflammatory bowel disease questionnaire (SIBDQ) were self-administered to assess patient knowledge of IBD and HRQoL, respectively. Demographic and disease characteristics were abstracted from the electronic medical record. The correlation between CCKNOW and SIBDQ scores was assessed by a linear regression model. Associations of patient knowledge and the variables of interest were calculated using ANOVA.
RESULTS: A total of 101 patients were recruited. Caucasian race, younger age at diagnosis, and having a college or post-graduate degree were significantly associated with higher CCKNOW scores. Patients with CD had higher CCKNOW scores compared to patients with ulcerative colitis and inflammatory bowel disease type unclassified, P < 0.01. There was no significant correlation between overall CCKNOW and SIBDQ scores (r2 = 0.34, P = 0.13). The knowledge sub-domain of diet in CCKNOW was negatively correlated with HRQoL (r2 = 0.69, P < 0.01).
CONCLUSION: IBD diagnosis at a younger age in addition to Caucasian race and higher education were significantly associated with higher knowledge about IBD. However, patient knowledge of IBD was not correlated with HRQoL. Further studies are required to study the effect of patient knowledge of IBD on other clinical outcomes.
Keywords: Crohn’s disease, Ulcerative colitis, Crohn’s and Colitis Knowledge Score, Short inflammatory bowel disease questionnaire, Health related quality of life
Core tip: No prior study on inflammatory bowel disease (IBD) has attempted to determine if there is a correlation between a patient’s knowledge about his/her disease and their health related quality of life. Furthermore, no such study attempting to quantify a patient’s knowledge of their IBD has been performed in the United States. While we found no statistically significant association, we did find several predictors of a patient’s knowledge about their disease as well as disparities in knowledge. Through this study, we hope to bring to light these predictors and disparities in hopes of providing targeted opportunities for patient directed education tools.
INTRODUCTION
Inflammatory bowel disease (IBD) is a chronic inflammatory condition of the gastrointestinal tract resulting in a marked decrease in health related quality of life (HRQoL)[1-4]. Despite advances in pharmacologic and surgical treatment strategies, patient understanding and knowledge of their disease varies widely[5]. It would appear that these advances have yet to translate into a meaningful improvement in patients’ understanding of their disease[6]. Poor knowledge and understanding about IBD may impair a patient’s ability to be an active participant in his/her own management. In one study, only 14% of ulcerative colitis (UC) patients in a tertiary care hospital were aware UC was associated with an increased risk of colorectal cancer (CRC)[7]. A working knowledge of their disease and its management is essential for patients with chronic disorders such as IBD[8]. Among patients with type 1 diabetes mellitus, higher levels of patient knowledge were associated with higher medication compliance and lower glycosylated hemoglobin levels[9,10].
Although a validated patient knowledge score for IBD has been developed (the Crohn’s and colitis knowledge score (CCKNOW), IBD patient knowledge has not been assessed in the United States patient population, nor has it been studied in relationship to HRQoL. Prior studies in the United Kingdom have demonstrated considerable gaps in patient knowledge specifically in medication options and IBD related complications[8]. Demographic and disease-related factors may potentially be used to identify patients at risk for non-adherence, though published studies have reported conflicting data[11,12]. Additionally, disease related knowledge of IBD among patients may affect adherence to medications or coping skills, and hence affect HRQoL.
We hypothesized that IBD-specific knowledge is associated HRQoL. The primary aim of this study was to identify associated patient and disease related factors associated with IBD knowledge. Secondary aims of this study were to quantify disease related knowledge among United States military veterans with IBD receiving care from the veterans affairs (VA) health system and to assess the association between knowledge and HRQoL. Identification of deficits by knowledge domain may provide opportunities for focused interventional patient education, and provide a baseline measurement against which future programs can be measured.
MATERIALS AND METHODS
Study population
Patients were recruited from the IBD clinic at the Michael E. DeBakey VA Medical Center in Houston, TX. Inclusion criteria: (1) diagnosis of IBD ascertained by a gastroenterologist based on clinical, endoscopic, and radiographic data[13]; (2) a diagnosis of IBD greater than 3 mo from enrollment; and (3) at least one prior outpatient clinic visit with a gastroenterologist. Patients who declined consent were excluded. Patients were recruited in a consecutive fashion and were asked to complete two self-assessed questionnaires at the time of their clinic visit.
Data collection
The CCKNOW and short inflammatory bowel disease questionnaire (SIBDQ) were prospectively completed at the time of clinic encounter. Another published IBD questionnaire, the Jones Knowledge Questionnaire, has limited evidence to support its use whereas the CCNOW has been embraced internationally[14]. Therefore the Jones Knowledge Questionnaire was not administered. The CCKNOW is a 30-item questionnaire that quantifies the disease-related knowledge of patients with IBD based on four domains: general knowledge, medication, diet, and complications of IBD. CCKNOW has been shown to be readable and reliable[8]. Permission to use the SIBDQ was obtained from McMaster University. The SIBDQ uses 10 questions derived from the original 32 item full Inflammatory Bowel Disease Questionnaire to subjectively assess the HRQoL in patients with IBD[15,16]. The SIBDQ examines four domains: bowel symptoms, systemic symptoms, emotional function, and social function. Each question is scored from 0 to 7 with a total score ranging from 10 (worst health) to 70 (best health). The total score is then divided by 10.
Medical chart review was performed by two of the investigators (JT and TM) using a standardized data collection form. Data were collected for care documented in the VA clinical encounter when the patient was enrolled. IBD diagnosis was confirmed based on endoscopic, histologic or radiologic findings consistent with standard clinical criteria[13]. Demographic data (race and ethnicity, gender, education), disease characteristics (age at diagnosis, IBD type, disease location, extra-intestinal manifestations), surgical history, and IBD related hospitalizations were abstracted. Education was classified as no high school, high school graduate, college degree, and post-graduate degree. Ethnicity was based on self-reported classification as Caucasian, Hispanic, African-American, Asian, other, and unknown. IBD age of diagnosis, location, and behavior were described according to the Montreal classification[17]. Bowel resection was defined as any small bowel or colonic resection, excluding perianal surgery. Perianal surgery included fistulotomy, abscess drainage, and seton placement. Extraintestinal manifestations (EIM) were defined as involvement of skin (pyoderma gangrenous or erythema nodosum), eye (uveitis, iritis, or episcleritis), or joint (inflammatory arthritis) and primary sclerosing cholangitis (PSC). Physician global assessment (PGA) was specifically noted in progress notes as quiescent, mild, moderate or severe.
Statistical analysis
The correlation between CCKNOW and SIBDQ scores was assessed by a linear regression model, and expressed as the Pearson correlation coefficient. Categorical variables were defined as age of diagnosis (< 17 years old, 17-40 years old, > 40 years old); current age (< 65 years old, ≥ 65 years old); education (college degree vs no college degree); race (Caucasian vs non-Caucasian); previous number of surgeries (0 or ≥ 1); disease duration (< 5, ≥ 5 years); and disease activity (remission vs active disease by PGA). The association of patient knowledge and the variables of interest were calculated ANOVA. Statistical analysis was performed using Stata version 11 software.
RESULTS
A total of 101 IBD patients were recruited consisting of 49 patients with UC (48.5%), 43 patients with Crohn’s disease (CD) (42.6%), and 9 patients with inflammatory bowel disease type unclassified (IBDU) (8.9%) (Table 1). The patients were 91% male, 66% Caucasian, and 34% non-Caucasian (27% African-American, 5% Hispanic, and 2% Asian). The mean age at time of IBD diagnosis was 39.6 years [standard deviation (SD) 14.6], and the mean age at time of enrollment was 51.5 years (SD 13.3) (Table 2). The average duration of disease of these patients was 11.8 years (SD 11.5). Of the 52 patients who provided their level of education, 35% had a college or post-graduate degree. The average CCKNOW score was 11.5 (SD 5.2), representing correct answers to 38% of questions.
Table 1.
Demographic features and their association with patient knowledge (Crohn’s and Colitis knowledge score)
| CCKNOW score, mean ± SD | P value | ||
| Total | 101% | 11.5 ± 5.2 | |
| Gender | 0.06 | ||
| Female | 9% | 14.8 ± 3.2 | |
| Male | 91% | 11.2 ± 5.2 | |
| Race | 0.02 | ||
| Caucasian | 33.70% | 12.5 ± 5.2 | |
| Non-caucasian | 66.30% | 9.6 ± 4.7 | |
| Age at diagnosis (yr) | < 0.01 | ||
| < 17 | 1% | 14 ± 0.0 | |
| 17-40 | 56.4% | 13.1 ± 4.8 | |
| > 40 | 42.6% | 9.2 ± 7.8 | |
| Level of education | 0.07 | ||
| No college | 65% | 10.7 ± 4.1 | |
| College/ post-graduate | 35% | 13.5 ± 5.4 |
CCKNOW: Crohn’s and Colitis knowledge score.
Table 2.
Inflammatory bowel disease characteristics and their association with patient knowledge (Crohn’s and Colitis knowledge score)
| Characteristics | CCKNOW Score, mean ± SD | P value | |
| Disease duration (yr) | 0.02 | ||
| < 5 | 37.6% | 9.9 ± 5.2 | |
| ≥ 5 | 62.4% | 12.5 ± 4.9 | |
| Type of IBD | < 0.01 | ||
| UC | 48.5% | 10.2 ± 4.7 | |
| CD | 42.6% | 13.6 ± 5.0 | |
| IBDU | 8.9% | 8.8 ± 5.9 | |
| UC location | 0.53 | ||
| Proctitis | 18.4% | 9.5 ± 2.9 | |
| Left colon | 22.4% | 9.8 ± 5.5 | |
| Pancolitis | 53.1% | 11.1 ± 4.9 | |
| NA | 6.1% | 7 ± 2.7 | |
| CD location | 0.92 | ||
| Proximal | 0 | - | |
| Ileal | 21% | 13.1 ± 2.6 | |
| Ileocolonic | 58% | 13.9 ± 5.2 | |
| Colonic | 21% | 13.4 ± 6.6 | |
| Family history of IBD | 0.69 | ||
| Yes | 14.9% | 12.6 ± 5.9 | |
| No | 80.1% | 11.3 ± 5.1 | |
| Unknown/adopted | 5% | 10.7 ± 5.8 | |
| Tobacco | 0.14 | ||
| Never | 39.6% | 12.6 ± 4.9 | |
| Current | 18.8% | 12.1 ± 5.8 | |
| Quit | 41.6% | 10.2 ± 4.9 | |
| IBD-related Hospitalizations | 0.23 | ||
| 0 | 62.4% | 11 ± 5.2 | |
| ≥ 1 | 37.6% | 12.4 ± 5.1 | |
| Previous IBD-related surgeries | 0.02 | ||
| 0 | 65.3% | 10.5 ± 5.0 | |
| ≥ 1 | 34.7% | 13.3 ± 5.1 |
CCKNOW: Crohn’s and Colitis knowledge score; SD: Standard deviation; IBD: Inflammatory bowel disease; UC: Ulcerative colitis; CD: Crohn’s disease; IBDU: Inflammatory bowel disease unclassified.
Association of patient knowledge and HRQoL
There was no significant correlation between overall CCKNOW and SIBDQ scores (r2 = 0.34, P = 0.13) (Figure 1). On analysis of CCKNOW sub-domains, higher diet knowledge scores were moderately associated with lower HRQoL (r2 = 0.69, P < 0.01). There were no associations between the general knowledge, treatment, and complication sub-domains with SIBDQ scores (r2 = 0.49, P = 0.25; r2 = 0.41, P = 0.67; r2 = 0.44, P = 0.59, respectively).
Figure 1.
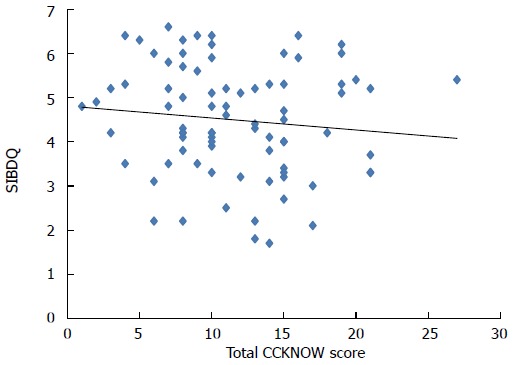
Correlation of quantified patient knowledge (Crohn’s and Colitis knowledge score) and health related quality of life (short inflammatory bowel disease questionnaire).
Patient factors associated with patient knowledge
Caucasian patients had higher CCKNOW overall scores as well as general knowledge sub-domain CCKNOW scores (7.75 ± 3.20) compared to non-Caucasians (6.00 ± 2.98), P = 0.03 (Table 1). While Caucasian patients had numerically higher CCKNOW scores in diet, treatment, and complication domains compared to non-Caucasians, these were not statistically significant (Table 3).
Table 3.
Inflammatory bowel disease characteristics and Crohn’s and Colitis knowledge score sub-domains
| Characteristics | General knowledge | SD | P value | Diet | SD | P value | Treatment | SD | P value | Complications | SD | P value |
| Gender | 0.09 | 0.06 | 0.56 | 0.04 | ||||||||
| Male | 43% | 20.39 | 45.15% | 23.51 | 25.47% | 20.43 | 29.56% | 19.25 | ||||
| Female | 55.47% | 10.47 | 61.11% | 33.33 | 29.63% | 20.03 | 43.75% | 12.40 | ||||
| Race | 0.03 | 0.26 | 0.28 | 0.08 | ||||||||
| Caucasian | 47.34% | 20.00 | 48.51% | 24.57 | 27.44% | 21.13 | 33.33% | 20.81 | ||||
| Non-caucasian | 37.5% | 18.64 | 42.65% | 25.02 | 22.73% | 18.55 | 26.04% | 14.63 | ||||
| Education | 0.10 | < 0.01 | 0.48 | 0.15 | ||||||||
| No college | 39.54% | 15.52 | 41.18% | 19.35 | 26.26% | 20.85 | 31.25% | 15.70 | ||||
| College/post-graduate | 48.75% | 21.16 | 58.33% | 19.17 | 30.56% | 20.00 | 40% | 25.04 | ||||
| IBD type | < 0.01 | 0.52 | 0.15 | 0.17 | ||||||||
| UC | 39.49% | 17.67 | 45.92% | 22.45 | 20.92% | 19.64 | 28.03% | 18.89 | ||||
| CD | 51.92% | 19.88 | 45.35% | 28.48 | 30.49% | 20.38 | 35% | 19.17 | ||||
| IBDU | 31.25% | 20.59 | 55.56% | 16.67 | 20.37% | 21.70 | 25% | 23.57 |
CCKNOW: Crohn’s and Colitis Knowledge score; SD: Standard deviation; IBD: Inflammatory bowel disease; UC: Ulcerative colitis; CD: Crohn’s disease; IBDU: Inflammatory bowel disease type unclassified.
Higher levels of education were numerically but not statistically significantly associated with overall higher CCKNOW scores, P = 0.22. Patients with a college or post-graduate degree had a higher diet subdomain CCKNOW scores (1.16 ± 0.38) compared to patients with no college degree (0.82 ± 0.39) P < 0.01. While patients with a college or post-graduate degree had higher numerical CCKNOW scores in general knowledge, treatment, and complications domains, these were not statistically significant.
Younger age of diagnosis was associated with higher CCKNOW scores. This association was seen across all knowledge sub-domains [general knowledge (P < 0.01), treatment (P = 0.02) and complications (P = 0.03)], except for diet (P = 0.12). Longer disease duration was also associated with higher CCKNOW scores (9.91 vs 12.54, for < 5 and ≥ 5 years, respectively, P = 0.02). Neither family history nor tobacco use was associated with CCKNOW scores.
IBD factors associated with patient knowledge
CD patients had higher CCKNOW scores (13.58; SD 4.95) compared to patients with UC (10.24 ± 4.65) and IBDU (8.75 ± 5.90), P < 0.01. Patients with a history of IBD related surgeries also had a higher CCKNOW (13.33 ± 5.09) compared to those without surgery (10.51 ± 4.98), P = 0.02. However, prior hospitalization, disease location, and disease activity were not associated with CCKNOW score.
Patients with joint EIMs had significantly higher CCKNOW scores (13.50 ± 5.54) compared to patients without joint manifestations (10.81 ± 4.89), P = 0.03. Other EIMs were not associated with CCKNOW score.
DISCUSSION
Caucasian race, younger age at time of diagnosis, and having a college or post-graduate degree were statistically significantly associated with higher CCKNOW scores. The patient populations of greatest IBD-specific knowledge deficiencies were in patients who were non-Caucasian, did not have a college or post-graduate degree, and at an older age at IBD diagnosis. However, we observed no significant correlation between overall patient knowledge of IBD and HRQoL, although higher diet related knowledge was associated with lower HRQoL.
We observed similar IBD-specific patient knowledge scores to prior studies in non- United States populations, ranging from a median CCKNOW score of 4 in Iran, to 7-10 in the United Kingdom, to 13 in Canada[18-20]. Caucasian race was associated with higher disease related knowledge in our study. In our study, all patients were native English speakers and therefore we do not believe the racial disparity observed can be attributed to a language barrier. Our observation of racial disparity in IBD knowledge is in contrast to a prior study from Australia using CCKNOW among 258 IBD patients recruited from ambulatory clinics and outpatient offices which showed no difference in knowledge based on race comparing Caucasians and non-Caucasians[21]. However, our observation is in line with those observed in other disease states. A study by Abubakari et al[22] evaluating disease knowledge among patients with type 2 diabetes found that white-British patients had a higher disease-specific knowledge compared to black-African and black-Caribbean counterparts. Additionally, the study found that the latter two populations had high levels of misconceptions regarding their disease compared to the white-British patients. Racial disparities in disease specific knowledge have been attributed to level of education as well as health literacy[18,19]. Racial disparities in IBD-specific knowledge, as identified in our study, highlight potential areas of educational intervention, specifically targeting non-Caucasian populations.
We observed that a younger age at time of IBD diagnosis was associated with greater disease-specific knowledge. This was independent from duration of disease, which was not significantly associated with IBD-specific knowledge. Younger patients may be more likely to seek information on their own or have easier access to information outside of the medical setting. Presumably, younger patients may possess an increased access to online research enabling them to ascertain more validated or accurate disease information. However, patient access to potentially inaccurate internet information may be damaging[23-25]. Our observations suggest educational programs and materials may need to be tailored to reach older patients with IBD.
Although we did not observe a correlation between patient knowledge and HRQoL, areas of knowledge deficiency may still have a significant clinical impact and role in patient activation and self-care. One possible reason for our finding is that patients lack self-efficacy - even if aware of their disease state, they may lack the means to change their health and be active members in medical decisions making. It is also possible that increased knowledge about one’s disease may result in depression, anxiety, or fear about the disease. Larsson and colleagues demonstrated that patients with high levels of anxiety did not exhibit improved angst after participating in educational programs about their disease[26]. Despite this, non-adherence has not been shown to be associated with anxiety and depression or disease-related patient knowledge[27].
Patients have been shown to rely on clinicians for their information needs[28]. A study assessing the effective measure of patient education to improve IBD-specific reproductive knowledge, found a single group-delivered session increased patient understanding and knowledge regarding the implications of disease for fertility and pregnancy[29]. This study used another precise questionnaire developed by Selinger entitled the Crohn’s and Colitis Pregnancy Knowledge Score (CCPKnow)[30]. Of the CCKNOW sub-domains, higher diet knowledge scores were significantly correlated with lower HRQoL. This finding may in part reflect the diet specific questions on the CCKNOW that refer to enteral nutrition and lactose intolerance, which may bias towards patients with a history of more severe disease.
Our study has several limitations. Level of education was missing in 49% of patients who declined to answer that question on the survey. However, we were still able to detect differences in level of education associated with disease-specific knowledge. The surveys were self-administered and health literacy may impact the assessment of disease-specific knowledge and decrease the scores of CCKNOW. It is also important to note that half of patients felt CCNOW questions were too difficult as documented in a previous study by Elkjaer et al[31]. Lastly, the patient population in this study was predominantly male, which is typically expected in the VA patient population. Therefore, conclusions regarding gender may not be generalizable. However, CCKNOW scores observed in this study parallel those of studies in other patient populations. Despite these limitations, our study has several strengths. This is the first study to use both the CCKNOW and SIBDQ questionnaires to evaluate patient knowledge and HRQoL in patients with IBD in the United States and also within the Veteran population. The Veteran patient population also represents a relatively diverse IBD population, both in race and age, relative to other frequently studied IBD populations. SIBDQ and CCKNOW were obtained prospectively from a non-tertiary practice and may therefore more closely represent IBD patients in the general population compared to complicated patients referred to tertiary IBD referral centers.
In conclusion, a cohort of United States military veterans with IBD, disease-specific knowledge of IBD was not correlated with HRQoL. Variations in disease-specific knowledge of IBD were observed based on age at IBD diagnosis, level of education, and race. These disparities may provide targeted opportunities for patient directed education tools. Further studies are required to study the effect of patient knowledge of IBD on other clinical outcomes.
COMMENTS
Background
Amongst a United States military veteran population with inflammatory bowel disease (IBD), disease-specific knowledge of IBD was not correlated with health related quality of life (HRQoL). While no correlation was shown, specific variables including Caucasian race, younger age at time of diagnosis, and having a college or post-graduate degree were significantly associated with higher Crohn’s and colitis knowledge score (CCKNOW) scores.
Research frontiers
Although disease-related IBD knowledge may not be directly correlated with overall HRQoL as observed in this study, the wide variation in disease-specific knowledge provides important insight into opportunities to address knowledge gaps and improve other clinical outcomes.
Innovations and breakthroughs
Despite the existence of a validated patient knowledge score in the CCKNOW in Europe, IBD patient knowledge has not been assessed in the United States to date. This is the first study to explore the correlation between CCKNOW and SIBDQ questionnaires to evaluate patient knowledge and HRQoL in patients with IBD in the United States and also within the Veteran population.
Applications
Given the identified variations in disease-specific IBD knowledge based upon race, age of diagnosis, and education level, future studies and projects may shed light on expanding programs to narrow this gap in an effort to improve a range of clinical outcomes.
Peer-review
This study is interesting and useful for the medical practice.
Footnotes
Supported by American College of Gastroenterology Junior Faculty Development Award (Hou) and with resources at the VA HSRD Center for Innovations in Quality, Effectiveness and Safety No. CIN 13-413, at the Michael E DeBakey VA Medical Center, Houston, TX (Hou).
Ethics approval: This study was conducted with the approval of the Baylor College of Medicine Institutional Review Board and the Michael E. DeBakey Veterans Affairs Medical Center Office of Research in Houston, Texas.
Informed consent: All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Conflict-of-interest: The authors have no disclosures relevant to this manuscript.
Data sharing: No additional data are available.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: November 10, 2014
First decision: December 11, 2014
Article in press: February 5, 2015
P- Reviewer: Mihaila RG S- Editor: Qi Y L- Editor: A E- Editor: Zhang DN
References
- 1.Allen PB, Kamm MA, Peyrin-Biroulet L, Studd C, McDowell C, Allen BC, Connell WR, De Cruz PP, Bell SJ, Elliot RP, et al. Development and validation of a patient-reported disability measurement tool for patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2013;37:438–444. doi: 10.1111/apt.12187. [DOI] [PubMed] [Google Scholar]
- 2.Drossman DA, Patrick DL, Mitchell CM, Zagami EA, Appelbaum MI. Health-related quality of life in inflammatory bowel disease. Functional status and patient worries and concerns. Dig Dis Sci. 1989;34:1379–1386. doi: 10.1007/BF01538073. [DOI] [PubMed] [Google Scholar]
- 3.Farmer RG, Easley KA, Farmer JM. Quality of life assessment by patients with inflammatory bowel disease. Cleve Clin J Med. 1992;59:35–42. doi: 10.3949/ccjm.59.1.35. [DOI] [PubMed] [Google Scholar]
- 4.Sørensen VZ, Olsen BG, Binder V. Life prospects and quality of life in patients with Crohn’s disease. Gut. 1987;28:382–385. doi: 10.1136/gut.28.4.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wolfe BJ, Sirois FM. Beyond standard quality of life measures: the subjective experiences of living with inflammatory bowel disease. Qual Life Res. 2008;17:877–886. doi: 10.1007/s11136-008-9362-1. [DOI] [PubMed] [Google Scholar]
- 6.Limdi JK, Soteriadou S. CCKNOW and the dilemma of patient knowledge in inflammatory bowel disease. Eur J Gastroenterol Hepatol. 2014;26:574–575. doi: 10.1097/MEG.0000000000000071. [DOI] [PubMed] [Google Scholar]
- 7.Subasinghe D, Wijekoon NS, Nawarathne NM, Samarasekera DN. Disease-related knowledge in inflammatory bowel disease: experience of a tertiary care centre in a developing country in South Asia. Singapore Med J. 2010;51:484–489. [PubMed] [Google Scholar]
- 8.Eaden JA, Abrams K, Mayberry JF. The Crohn’s and Colitis Knowledge Score: a test for measuring patient knowledge in inflammatory bowel disease. Am J Gastroenterol. 1999;94:3560–3566. doi: 10.1111/j.1572-0241.1999.01536.x. [DOI] [PubMed] [Google Scholar]
- 9.Surawy C. Knowledge about diabetes in type 1 patients is related to metabolic control. Diabet Med. 1989;6:784–786. doi: 10.1111/j.1464-5491.1989.tb01279.x. [DOI] [PubMed] [Google Scholar]
- 10.Tan AS, Yong LS, Wan S, Wong ML. Patient education in the management of diabetes mellitus. Singapore Med J. 1997;38:156–160. [PubMed] [Google Scholar]
- 11.Jackson CA, Clatworthy J, Robinson A, Horne R. Factors associated with non-adherence to oral medication for inflammatory bowel disease: a systematic review. Am J Gastroenterol. 2010;105:525–539. doi: 10.1038/ajg.2009.685. [DOI] [PubMed] [Google Scholar]
- 12.Selinger CP, Robinson A, Leong RW. Clinical impact and drivers of non-adherence to maintenance medication for inflammatory bowel disease. Expert Opin Drug Saf. 2011;10:863–870. doi: 10.1517/14740338.2011.583915. [DOI] [PubMed] [Google Scholar]
- 13.Nikolaus S, Schreiber S. Diagnostics of inflammatory bowel disease. Gastroenterology. 2007;133:1670–1689. doi: 10.1053/j.gastro.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 14.Jones SC, Gallacher B, Lobo AJ, Axon AT. A patient knowledge questionnaire in inflammatory bowel disease. J Clin Gastroenterol. 1993;17:21–24. doi: 10.1097/00004836-199307000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Guyatt G, Mitchell A, Irvine EJ, Singer J, Williams N, Goodacre R, Tompkins C. A new measure of health status for clinical trials in inflammatory bowel disease. Gastroenterology. 1989;96:804–810. [PubMed] [Google Scholar]
- 16.Irvine EJ, Zhou Q, Thompson AK. The Short Inflammatory Bowel Disease Questionnaire: a quality of life instrument for community physicians managing inflammatory bowel disease. CCRPT Investigators. Canadian Crohn’s Relapse Prevention Trial. Am J Gastroenterol. 1996;91:1571–1578. [PubMed] [Google Scholar]
- 17.Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006;55:749–753. doi: 10.1136/gut.2005.082909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wardle RA, Mayberry JF. Patient knowledge in inflammatory bowel disease: the Crohn’s and Colitis Knowledge Score. Eur J Gastroenterol Hepatol. 2014;26:1–5. doi: 10.1097/MEG.0b013e328365d21a. [DOI] [PubMed] [Google Scholar]
- 19.Butcher RO, Law TL, Prudham RC, Limdi JK. Patient knowledge in inflammatory bowel disease: CCKNOW, how much do they know? Inflamm Bowel Dis. 2011;17:E131–E132. doi: 10.1002/ibd.21810. [DOI] [PubMed] [Google Scholar]
- 20.Rezailashkajani M, Roshandel D, Ansari S, Zali MR. Knowledge of disease and health information needs of the patients with inflammatory bowel disease in a developing country. Int J Colorectal Dis. 2006;21:433–440. doi: 10.1007/s00384-005-0030-4. [DOI] [PubMed] [Google Scholar]
- 21.Selinger CP, Lal S, Eaden J, Jones DB, Katelaris P, Chapman G, McDonald C, Leong RW, McLaughlin J. Better disease specific patient knowledge is associated with greater anxiety in inflammatory bowel disease. J Crohns Colitis. 2013;7:e214–e218. doi: 10.1016/j.crohns.2012.09.014. [DOI] [PubMed] [Google Scholar]
- 22.Abubakari AR, Jones MC, Lauder W, Kirk A, Anderson J, Devendra D, Naderali EK. Ethnic differences and socio-demographic predictors of illness perceptions, self-management, and metabolic control of type 2 diabetes. Int J Gen Med. 2013;6:617–628. doi: 10.2147/IJGM.S46649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Angelucci E, Orlando A, Ardizzone S, Guidi L, Sorrentino D, Fries W, Astegiano M, Sociale O, Cesarini M, Renna S, et al. Internet use among inflammatory bowel disease patients: an Italian multicenter survey. Eur J Gastroenterol Hepatol. 2009;21:1036–1041. doi: 10.1097/MEG.0b013e328321b112. [DOI] [PubMed] [Google Scholar]
- 24.Cima RR, Anderson KJ, Larson DW, Dozois EJ, Hassan I, Sandborn WJ, Loftus EV, Pemberton JH. Internet use by patients in an inflammatory bowel disease specialty clinic. Inflamm Bowel Dis. 2007;13:1266–1270. doi: 10.1002/ibd.20198. [DOI] [PubMed] [Google Scholar]
- 25.Powell JA, Darvell M, Gray JA. The doctor, the patient and the world-wide web: how the internet is changing healthcare. J R Soc Med. 2003;96:74–76. doi: 10.1258/jrsm.96.2.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Larsson K, Sundberg Hjelm M, Karlbom U, Nordin K, Anderberg UM, Lööf L. A group-based patient education programme for high-anxiety patients with Crohn disease or ulcerative colitis. Scand J Gastroenterol. 2003;38:763–769. doi: 10.1080/00365520310003309. [DOI] [PubMed] [Google Scholar]
- 27.Selinger CP, Eaden J, Jones DB, Katelaris P, Chapman G, McDonald C, Smith P, Lal S, Leong RW, McLaughlin J, et al. Modifiable factors associated with nonadherence to maintenance medication for inflammatory bowel disease. Inflamm Bowel Dis. 2013;19:2199–2206. doi: 10.1097/MIB.0b013e31829ed8a6. [DOI] [PubMed] [Google Scholar]
- 28.Limdi JK, Butcher RO. Information resources and inflammatory bowel disease. Inflamm Bowel Dis. 2011;17:E89–E90. doi: 10.1002/ibd.21749. [DOI] [PubMed] [Google Scholar]
- 29.Mountifield R, Andrews JM, Bampton P. It IS worth the effort: Patient knowledge of reproductive aspects of inflammatory bowel disease improves dramatically after a single group education session. J Crohns Colitis. 2014;8:796–801. doi: 10.1016/j.crohns.2013.12.019. [DOI] [PubMed] [Google Scholar]
- 30.Selinger CP, Eaden J, Selby W, Jones DB, Katelaris P, Chapman G, McDonald C, McLaughlin J, Leong RW, Lal S. Patients’ knowledge of pregnancy-related issues in inflammatory bowel disease and validation of a novel assessment tool (‘CCPKnow’) Aliment Pharmacol Ther. 2012;36:57–63. doi: 10.1111/j.1365-2036.2012.05130.x. [DOI] [PubMed] [Google Scholar]
- 31.Elkjaer M, Burisch J, Avnstrøm S, Lynge E, Munkholm P. Development of a Web-based concept for patients with ulcerative colitis and 5-aminosalicylic acid treatment. Eur J Gastroenterol Hepatol. 2010;22:695–704. doi: 10.1097/MEG.0b013e32832e0a18. [DOI] [PubMed] [Google Scholar]


