Abstract
Background
In the literature on nipple-sparing mastectomy (NSM) with one-stage immediate implant reconstruction, contralateral symmetrisation has drawn little attention, with many surgeons still performing standard cosmetic mammaplasty procedures. However, standard implant-based mammaplasty usually does not result in proper symmetry with the mastectomy side, especially regarding breast projection, overall shape, and volume distribution.
Methods
We retrospectively reviewed 19 consecutive patients undergoing unilateral NSM with immediate prosthetic reconstruction and contralateral simultaneous symmetrisation by using the tailored reduction/augmentation mammaplasty technique between June 2012 and August 2013.
Results
The average follow-up time was 13 months (range, 10-24 months). No major complications, such as infection, haematoma, and nipple-areola complex necrosis, were experienced.
Conclusions
Our experience suggests that simultaneous contralateral symmetrisation with tailored reduction/augmentation mammaplasty after unilateral immediate implant reconstruction after NSM facilitates durable and pleasant symmetric outcomes.
Keywords: Mastectomy; Mastectomy, subcutaneous; Breast implants; Mammaplasty
INTRODUCTION
The literature contains abundant studies on breast reconstruction techniques after nipple-sparing mastectomy (NSM) [1,2,3]. However, contralateral symmetrisation mammaplasty after unilateral NSM implant-based breast reconstruction has received little attention [4,5,6].
An implant with a larger volume than the removed conus is necessary to properly fill up the deflated breast envelope after NSM. Standard breast augmentation or augmentation/pexy performed contralaterally can often result in asymmetry, even if the implants used are smaller and shaped differently than those used on the reconstructed side. This occurs because the implant-to-breast transition on the mastectomy side is different from that on the healthy side.
The purpose of this paper is to present the tailored reduction/augmentation mammaplasty technique used to achieve simultaneous contralateral symmetrisation following immediate one-stage implant reconstruction after unilateral NSM.
METHODS
Patients and methods
Between June 2012 and August 2013, 19 consecutive women underwent unilateral NSM with immediate prosthetic reconstruction to treat breast cancer, followed by contralateral symmetrisation with implants. NSM was restricted to oncologic patients who met the following inclusion criteria: tumour size <5 cm, tumour ≥2 cm from the nipple-areola complex (NAC), no skin involvement or inflammatory breast cancer, clinically negative axillae or a negative frozen section of the sentinel node, a negative intraoperative frozen section of the tissue immediately beneath the nipple, and the patients' choice to undergo NSM instead of breast conservative surgery.
The mean age of the patients was 45.2 years old (range, 36-58 years old). Six patients were of normal weight (body mass index [BMI] range, 18.5-24.9 kg/m2) and 13 were overweight (BMI range, 25-29.9 kg/m2).
With the aid of sizers, hyper-projected (used on the NSM side) and low-projected (used on the contralateral side) anatomical silicone-gel textured implants were placed in the submuscular plane by dissecting the submuscular-subfascial pocket on the mastectomy side and the dual-plane pocket on the healthy side (Table 1) [7,8,9]. The submuscular-subfascial pocket is accessed from the upper lateral border of the pectoralis major muscle and is defined by the pectoralis major muscle and its overlying fascia (superficial pectoralis fascia) up to the inferior margin of the pectoralis major muscle and inferolaterally by the superficial pectoralis fascia and coracoacromial fascia [9].
Table 1. Patients' features along with mastectomy specimen data, implants and tailored reduction/augmentation data.
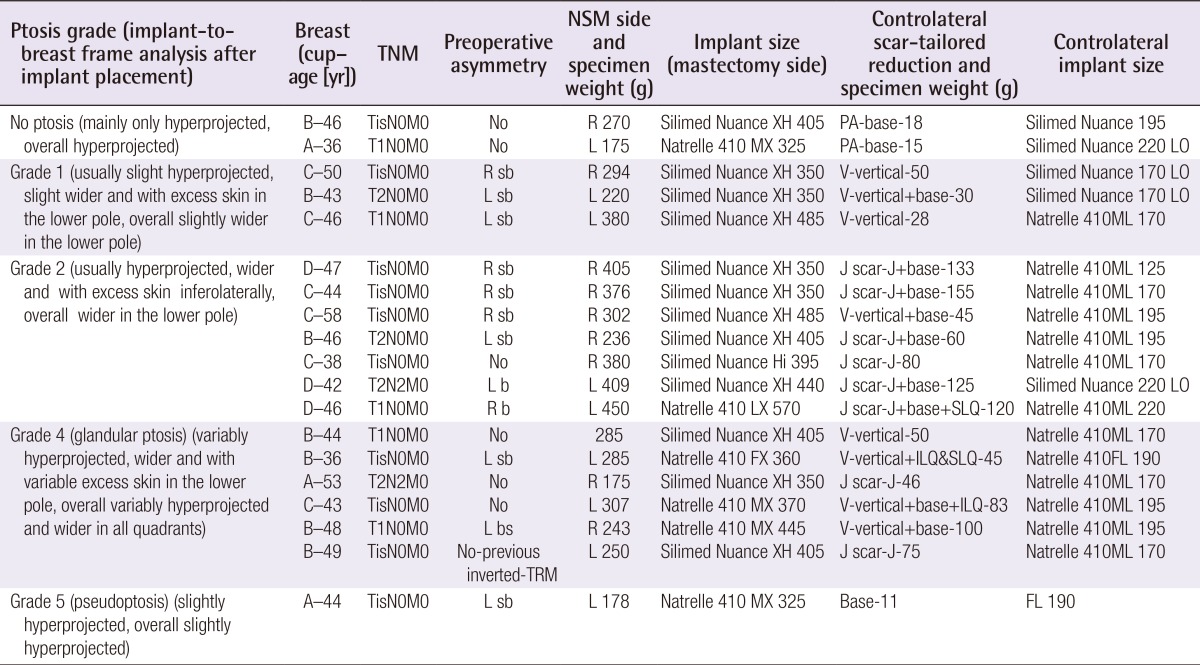
Grade 3 ptotic breasts and breasts with a cup size greater than D did not receive a surgical indication for implant-based reconstruction. Instead, autologous breast reconstruction was offered. Implants starting with letters (i.e., ML) are Allergan Natrelle 410 Style whereas implant starting with numbers are Silimed Nuance anatomical textured implants.
TNM, tumor, node, metastasis; NSM, nipple-sparing mastectomy; R, right; PA, periareolar; L, left; sb, slight bigger; V, vertical; b, bigger; ILQ, inferolateral quadrant; SLQ, superolateral quadrant; TRM, T reduction mammaplasty.
The reconstructive and aesthetic outcomes were evaluated separately by a blinded group of plastic surgeons as well as by the attending surgeon using our standard evaluation method (Table 2). This assessment was based on clinical examinations and by reviewing clinical pictures of the breasts. The BREAST-Q score was used to ascertain the patients' satisfaction.
Table 2. Evaluation methods of the aesthetic outcome using clinical photographs of the patients. It is based of five different items with three Likert subscales.
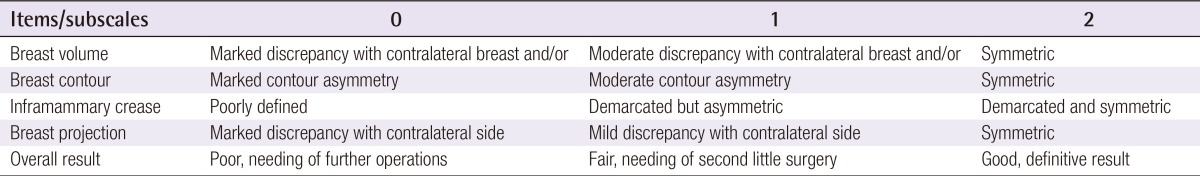
The cumulative score goes from 0 to 10, where 0-2 is considered as "bad", 3, 4 "poor", 5, 6 "fair", 7, 8 "good", and 9, 10 "excellent".
Surgical technique
After completing the NSM implant reconstruction, the dual-plane pocket was dissected on the healthy side through inferior hemi-periareolar access and the trans-parenchymal route. A low-projected anatomical silicone-gel textured implant was placed with the goal of ensuring a symmetrical breast bases. The patient was then placed in a semi-sitting position to check for symmetry. After implant placement, implant-to-breast transition analysis was performed by evaluating four parameters: projection, width, excess skin, and overall shape. This was carried out in order to tailor the contralateral symmetrisation after the implant was placed.
In non-ptotic breasts, the central breast base was reduced and circumareolar skin resection with interlocking suture (CRIS) was performed according to the technique described by Hammond [10,11].
Grade 1 and grade 2 ptotic breast cases were managed by vertical or J-scar breast reduction in order to correct the ptosis, to remove excess inferolateral breast tissue in the lower pole, and to match breast width. In these cases, projection was managed with central breast base reduction and CRIS.
Grade 4 (glandular ptosis) breast cases were managed according to the specific needs of each case. Since the excess breast tissue is not primarily displaced into the lower quadrants, as in ptotic breasts, but is instead distributed in all four quadrants, the tailored resection of both the inferolateral and superolateral quadrants may be needed to match the overall breast shape, in addition to vertical or J-scar breast reduction. In our study, this took place in two cases.
Grade 5 (pseudoptosis) breast cases were managed as non-ptotic breasts with smaller central breast base reduction and CRIS (Fig. 1).
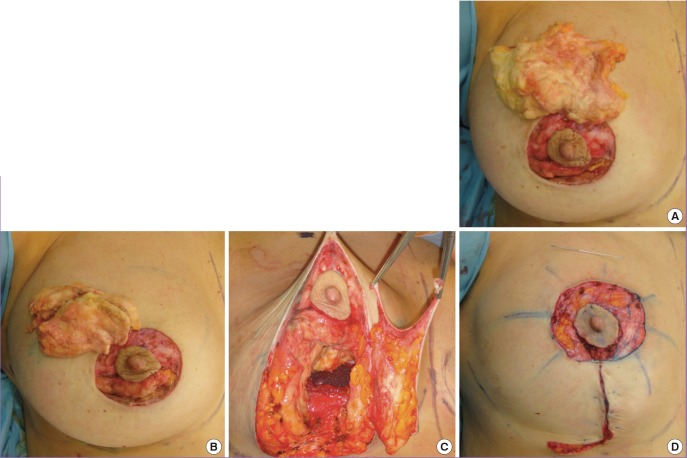
Fig. 1. Tailored mammaplasty case: intraoperative sequence.
(A) Dual-plane augmentation mammaplasty was performed through a periareolar approach, placing an Allergan Natrelle (Allergan Inc., Irvine, CA, USA) 410ML 220 mL implant. The breast base (i.e., retroareolar breast tissue) was removed. The specimen size is shown. (B) In order to symmetrize the lateral pole fullness, the superolateral breast quadrant was also resected. The specimen size is shown on the breast. (C) J-scar breast reduction was also performed. Notice the submuscular breast implant at the bottom of the image as well as the signs of tailored parenchyma resections. (D) Circumareolar skin resection and interlocking suture was performed before closure.
Augmentation mammoplasty was performed first, followed by the tailored resection of the central breast base and, eventually, the tailored resection of the lateral quadrants. Through inferior periareolar access, the central portion of the gland was undermined from the pectoralis major muscle and a bevelled resection was performed in the planned direction. After the resection, the patient was again placed into a semi-sitting position to check for symmetry. Vertical or J-scar breast reduction was performed when needed, following resection patterns that were marked intraoperatively [12]. Since this surgical manoeuvre further influences breast projection and overall shape, the breast was basted with temporary stitches, and then projection and overall shape were assessed. After the resection, the patient was again placed into a semi-sitting position to check for symmetry. If the implant-to-breast transition was still unsatisfactory, further resections of the base and, eventually, of the lateral quadrants were performed. The extent of periareolar skin resection was determined based on the goal of flattening the breast and NAC, and CRIS was performed with the goal of matching the contralateral NAC size (Figs. 2, 3).
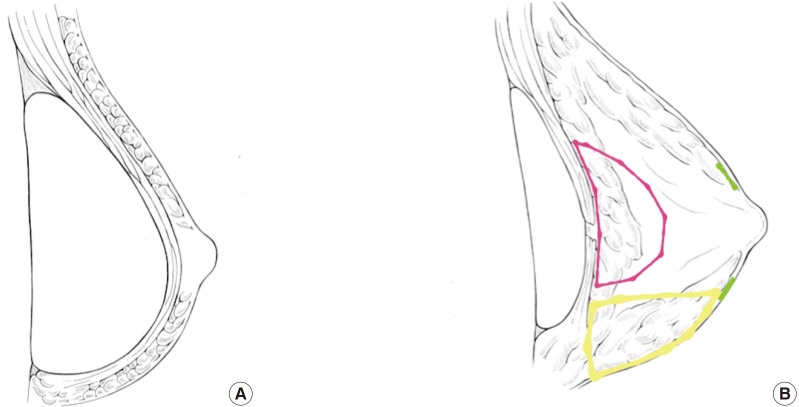
Fig. 2. Tailored mammaplasty along the breast transverse axis.
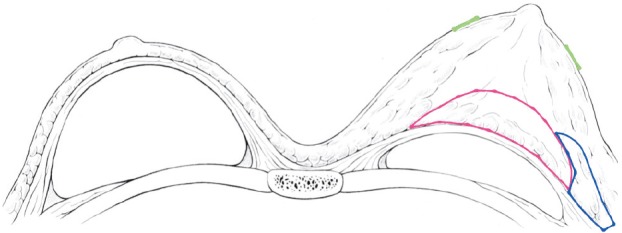
An artist's drawing illustrates the transverse axis of the right breast during one-stage immediate breast reconstruction after nipple-sparing mastectomy. Notice that the breast conus (parenchyma) is completely replaced by the definitive anatomic implant that provides the shape and projection of the reconstructed breast. The conical projection of the healthy breast is lost. The implant-to-breast transition is rough, consisting of the implant covered by the pectoralis major, a thin layer of subcutis, and skin. A smaller, low-projected implant has been placed in a dual-plane pocket to provide prosthetic imprinting to the contralateral breast. However, despite using the smallest implant possible, the augmentation mammaplasty alone cannot properly symmetrize the breast. The removal of the base of the breast (shown in pink), the resection of the lateral quadrants (shown in blue), and the removal of the circumareolar skin (shown in green) are the steps of tailored reduction designed to properly symmetrize the breast by flattening the breast and nipple-areola complex and symmetrizing the base of the breast.
Fig. 3. Tailored mammaplasty along the breast sagittal axis.
(A) An artist's drawing illustrates the sagittal axis of the breast during one-stage immediate breast reconstruction after nipple-sparing mastectomy. Notice that the breast conus (parenchyma) is completely replaced by the definitive anatomic implant that provides the shape and projection of the reconstructed breast. The conical projection of the healthy breast is lost. The implant-to-breast transition is rough, consisting of the implant covered by the pectoralis major, a thin layer of subcutis, and skin. (B) An artist's drawing shows the sagittal axis of the breast during a contralateral symmetrisation procedure. Notice that a smaller, low-projected implant has been placed in a dual-plane pocket to provide prosthetic imprinting to the contralateral breast. However, despite using the smallest implant possible, the augmentation mammaplasty alone cannot properly symmetrize the breast. The removal of the base of the breast (shown in pink), vertical/J-scar breast reduction (shown in yellow), and circumareolar skin removal (shown in green) are the steps of tailored reduction designed to properly symmetrize the breast by flattening the breast and nipple-areola complex and symmetrizing the base of the breast.
RESULTS
The average follow-up time was 13 months (range, 10-24 months). Seventeen of 19 patients did not require adjuvant chemo-radiotherapy according to the final tumour pathology, whereas two patients underwent postoperative radiotherapy because of the presence of more than four metastatic axillary nodes.
No major complications, such as infection, haematoma, or NAC necrosis, were experienced on the healthy symmetrized breasts.
Patient satisfaction was high to very high in all patients. No secondary procedures were needed on the healthy symmetrized breasts (Figs. 4, 5).
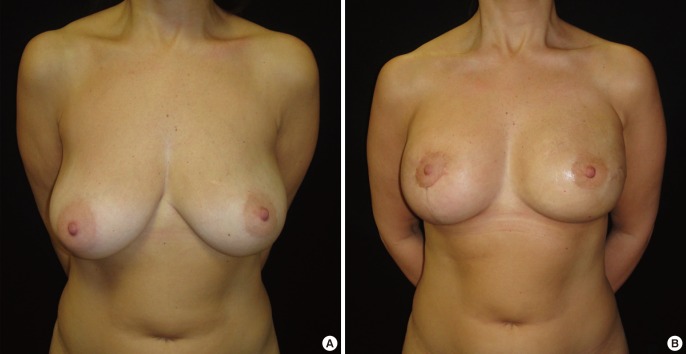
Fig. 4. A case of tailored mammaplasty.
(A) A preoperative picture of a 46-year-old left-breast cancer patient, for whom left nipple-sparing mastectomy, one-stage immediate reconstruction, and contralateral tailored reduction/augmentation mammaplasty were planned. Ptosis grade 2. (B) Two-month postoperative picture after left nipple-sparing mastectomy through a radial lazy S incision (mastectomy specimen 450 g) and implant reconstruction with an Allergan Natrelle (Allergan Inc., Irvine, CA, USA) 410LX 570 mL implant and contralateral tailored reduction/augmentation mammaplasty with a J-scar pattern; dual-plane augmentation with an Allergan Natrelle 410ML 220 g implant; inferior pole, base, and superolateral quadrant tailored reduction (total specimen weight of 120 g); and circumareolar skin resection with interlocking suture.
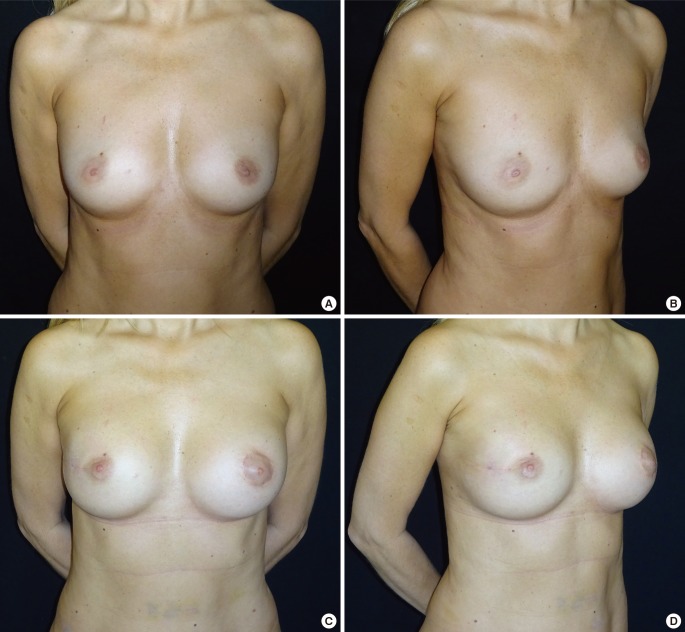
Fig. 5. A case of tailored mammaplasty.
(A, B) Preoperative pictures of a 45-year-old right-breast cancer patient for whom right nipple-sparing mastectomy, one-stage immediate reconstruction, and contralateral tailored reduction/augmentation mammaplasty were planned. No breast ptosis. (C, D) Three-month postoperative pictures after right nipple-sparing mastectomy through a radial lateral incision (mastectomy specimen 160 g) and implant reconstruction with a Silimed hyper-projected anatomical implant (Nuance 350 mL; Silimed International, Rio de Janeiro, Brazil). Contralateral tailored reduction/augmentation mammaplasty was performed via a periareolar scar, as well as dual-plane augmentation with an Allergan Natrelle 410ML 220 g (Allergan Inc., Irvine, CA, USA) implant, base reduction (specimen weight 35 g), and circumareolar skin resection with interlocking suture.
DISCUSSION
In NSM, unlike in skin-sparing mastectomy, constraints due to NAC positioning and whole-skin envelope preservation strongly limit the use of skin redraping procedures over the implant. These factors also have a dramatic influence on the contralateral symmetrisation procedure.
On the NSM side, the absence of the adipoglandular breast conus is responsible for a rough implant-to-breast transition, consisting of muscle and skin. The breast takes the shape of the implant with regard to height, width, and projection as the skin shrinks over the muscle, adapting to the new breast conus. The absence of the adipoglandular component strongly influences both projection, resulting in a somewhat flat breast with a shrunken NAC that is smaller in diameter, and the overall shape, which is not conical but more bowl-like.
When dealing with contralateral healthy breast symmetrisation, if a durable symmetrisation is sought, it is always necessary to place an implant in order to provide prosthetic imprinting on the contralateral side. Unlike the mastectomy side, the implant-to-breast transition on the healthy side is smoother because of the conus over the implant. This influences the height, width, projection, and overall shape of the new breast.
In order to optimize the symmetrisation, the surgeon should shape the healthy breast in order to make it similar to the reconstructed side.
Breast width and height can be easily matched by choosing the proper low-projection anatomical implant based on preoperative breast asymmetry (if any) and the dimensions of the reconstructive implant, with the aid of sizers. However, the healthy breast always has a hyper-projected (conical) appearance and sometimes has a different overall shape.
Hyper-projection can be easily managed by combining two manoeuvres: the tailored resection of central breast base in order to directly reduce projection and CRIS in order to flatten the breast and to match NAC size.
When the overall shape is still different, as occurs in larger and ptotic breasts, a vertical-to-J-scar inferior quadrant resection as well as a lateral quadrant tailored resection can help adjust the shape of the breast.
In conclusion, based on our experience, simultaneous contralateral symmetrisation with a tailored reduction/augmentation mammaplasty after unilateral immediate implant reconstruction following NSM is a technique that helps achieve durable and pleasant symmetric outcomes.
Footnotes
The authors thank Antonia Conti, Medical Artist, for designing high-fidelity artwork.
No potential conflict of interest relevant to this article was reported.
References
- 1.Endara M, Chen D, Verma K, et al. Breast reconstruction following nipple-sparing mastectomy: a systematic review of the literature with pooled analysis. Plast Reconstr Surg. 2013;132:1043–1054. doi: 10.1097/PRS.0b013e3182a48b8a. [DOI] [PubMed] [Google Scholar]
- 2.Salgarello M, Visconti G, Barone-Adesi L. Nipple-sparing mastectomy with immediate implant reconstruction: cosmetic outcomes and technical refinements. Plast Reconstr Surg. 2010;126:1460–1471. doi: 10.1097/PRS.0b013e3181ef8bce. [DOI] [PubMed] [Google Scholar]
- 3.Spear SL, Shuck J, Hannan L, et al. Evaluating long-term outcomes following nipple-sparing mastectomy and reconstruction in the irradiated breast. Plast Reconstr Surg. 2014;133:605e–614e. doi: 10.1097/PRS.0000000000000098. [DOI] [PubMed] [Google Scholar]
- 4.Losken A, Carlson GW, Bostwick J, 3rd, et al. Trends in unilateral breast reconstruction and management of the contralateral breast: the Emory experience. Plast Reconstr Surg. 2002;110:89–97. doi: 10.1097/00006534-200207000-00016. [DOI] [PubMed] [Google Scholar]
- 5.Leone MS, Priano V, Franchelli S, et al. Factors affecting symmetrization of the contralateral breast: a 7-year unilateral postmastectomy breast reconstruction experience. Aesthetic Plast Surg. 2011;35:446–451. doi: 10.1007/s00266-010-9622-7. [DOI] [PubMed] [Google Scholar]
- 6.Webster R. How does ptosis affect satisfaction after immediate reconstruction plus contralateral mammaplasty? Ann Plast Surg. 2010;65:294–299. doi: 10.1097/SAP.0b013e3181cc2a0a. [DOI] [PubMed] [Google Scholar]
- 7.Salgarello M, Visconti G, Barone-Adesi L. Dual-plane prosthetic reconstruction using the modified wise pattern mastectomy in women with macromastia. Plast Reconstr Surg. 2011;127:1740–1742. doi: 10.1097/PRS.0b013e31820a66b8. [DOI] [PubMed] [Google Scholar]
- 8.Salgarello M, Visconti G, Barone-Adesi L, et al. Inverted-T skin-reducing mastectomy with immediate implant reconstruction using the submuscular-subfascial pocket. Plast Reconstr Surg. 2012;130:31–41. doi: 10.1097/PRS.0b013e3182547d42. [DOI] [PubMed] [Google Scholar]
- 9.Salgarello M, Visconti G, Barone-Adesi L. One-stage immediate breast reconstruction with implants in conservative mastectomies [Internet] Croatia: InTech; 2012. [cited 2014 Jan 27]. Available from: http://www.intechopen.com/books/breast-reconstruction-current-techniques/one-stage-immediate-breast-reconstruction-with-implants-in-conservative-mastectomies. [Google Scholar]
- 10.Davidenko JM, Pertsov AV, Salomonsz R, et al. Stationary and drifting spiral waves of excitation in isolated cardiac muscle. Nature. 1992;355:349–351. doi: 10.1038/355349a0. [DOI] [PubMed] [Google Scholar]
- 11.Salgarello M, Visconti G, Barone-Adesi L. Interlocking circumareolar suture with undyed polyamide thread: a personal experience. Aesthetic Plast Surg. 2013;37:1061–1062. doi: 10.1007/s00266-013-0186-1. [DOI] [PubMed] [Google Scholar]
- 12.Gasperoni C, Salgarello M, Gasperoni P. A personal technique: mammaplasty with J scar. Ann Plast Surg. 2002;48:124–130. doi: 10.1097/00000637-200202000-00002. [DOI] [PubMed] [Google Scholar]