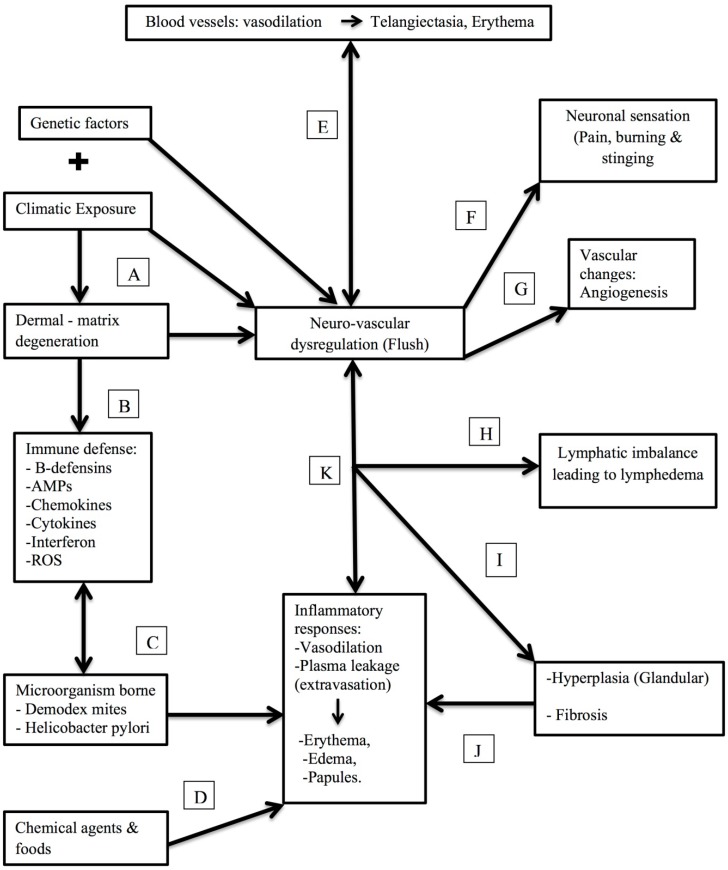
Figure 3.
The presumed pathophysiology of rosacea in correlation with specific molecular, immunological, neuronal and clinical triggers. (A) Recurrent exposure to extreme sunlight (environmental changes) causes the dermal matrix degeneration, which in turn may trigger genetic predisposition leading to hypersensitivity and flush on the skin. (B) As a part of hypersensitivity, it triggers the innate immune response. (C) Effect of microorganisms like Demodex and Helicobacter pylori gives rise to the several inflammatory responses in the body. (D) Chemical and food agents would also trigger inflammatory responses. (E) Vasodilation of blood vessels by immune responses that may lead to Telangiectasia, Erythema. (F) Neural activation results in vasodilatation, edema and burning sensation (G) Chronic neurogenic inflammation may lead to persistent erythema, followed by angiogenesis. (H) Imbalance in lymphatic system leads to lymphedema followed (I) Glandular hyperplasia and fibrosis (J) leading to inflammatory responses like vasodilation, extravasation and plasma leakage (severe case) giving rise to (K) erythema, edema and papules.