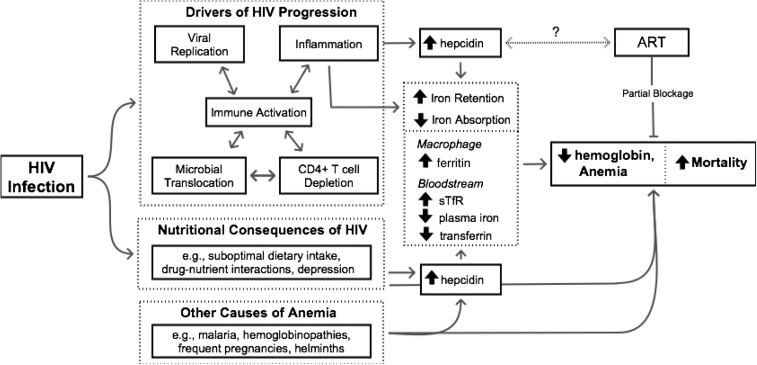
FIGURE 2.
Pathways to HIV-associated anemia. A complex combination of interdependent factors including viral replication, microbial translocation, CD4 cell depletion, and chronic immune activation has been proposed as the driving force behind HIV disease progression (36). The production of proinflammatory cytokines (including IL-6) appears to both contribute to and be dependent on factors driving disease progression and, in turn, stimulates hepcidin production and triggers the acute phase response. As a result, there is an increase in hepcidin-mediated ferroportin degradation and a characteristic shift in iron from the bloodstream to the macrophage that is characterized by decreased plasma iron, decreased hemoglobin, decreased transferrin, increased sTfR, and increased ferritin, ultimately resulting in HIV-associated anemia. Although ART is known to resolve some (but not all) HIV-associated anemia, its role in the proposed pathway is currently unknown. Alternatively, HIV-associated anemia may be the result of nutritional consequences of HIV and/or other (non–HIV-related) causes of anemia. Arrows indicate connected entities that are part of a pathway whereby solid arrows represent established pathways and dotted arrows remain hypothetical; lines ending without arrows indicate inhibition or blockage. ART, antiretroviral therapy; sTfR, soluble transferrin receptor.