Abstract
Background:
Despite the advances in surgical treatment options, massive rotator cuff (r-c) tears still represent a challenge for orthopedic surgeons. This study assesses the effectiveness of fascia lata allograft in reconstruction of massive and irreparable r-c tear and to evaluate the healing and functional outcomes.
Materials and Methods:
68 patients (38 men, 30 women, mean age 64.9 years) with massive or irreparable r-c tears were treated with placement of fascia lata allograft to fill the defect between February 2006 and February 2010. At 43 months followup they were evaluated clinically using the constant score, preoperatively and postoperatively. Magnetic resonance imaging (MRI) and ultrasound were used postoperatively, to assess the integrity of the allograft at the repair site. Postoperatively, standard rehabilitation protocol was followed with gradual restoration.
Results:
Postoperative constant score increased from 32.5 preoperatively to 88.7 postoperatively. The most important was the pain relief from 2.4 preoperatively to 14.1 postoperatively and range of motion. The results of the MRI were not reliable, but the ultrasound was satisfactory. Finally, there was no infection or rejection of the graft in any of the patients.
Conclusions:
Despite advances in surgical methods, there is still not a universally accepted treatment for massive and irreparable rotator cuff tears, because the standard methods have dubious results, with excessive retear rates and poor outcomes, necessitating the need for new repair strategies. We documented significant clinical improvement using fascia lata allograft in the repair of massive irreparable r-c tear, acting as scaffold to bridge the defect, enhancing the healing at the repair site.
Keywords: Allograft reconstruction, fascia lata allograft, rotator cuff tear, patch graft, rotator cuff repair, shoulder
MeSH terms: Allograft, shoulder, rotator cuff
INTRODUCTION
There have been various classifications to define a massive rotator cuff (r-c) tear. DeOrio and Cofield defined it as a tear of one tendon measuring more than 5 cm in diameter. Other authors define massive tears as those involving at least two complete tendons. Others classify them based on chronicity and acuity or the location of the tear as posterosuperior or anterosuperior.1,2,3,4 As reported by Neer, Harryman and others, up to 30% of rotator cuff tears may present as massive irreparable tears1,5 and the postoperative retear rates after primary repairs range from 20% to 90%.6,7,8,9 Noteworthy is that in USA there are performed about 3,000,000 repairs of the r-c on an annual basis, which costs $3 billion.10 These tears are likely to cause pain, weakness, periscapular atrophy, reduced shoulder range of motion (ROM) and degenerative changes in the glenohumeral joint over time.2,10 Factors believed to contribute to this high failure rate of tears include size of the tear, tendon quality, degree of muscle atrophy, acuity, postoperative rehabilitation protocol, age, repair technique, tension on the repair, and hypovascularity of the r-c.8,9,11,12,13,14,15,16 Consequently, treatment of massive r-c tears still presents a major challenge for the orthopedic surgeon.5,17,18,19,20,21 Many surgical procedures have been developed including debridement of the r-c without attempting reconstruction, partial repair, various tendon transfers (the most recent of latissimus dorsi) however characterized by donor site morbidity.1,16 Other procedures are the glenohumeral arthrodesis, reverse total shoulder arthroplasty when tear is associated with glenohumeral joint arthropathy, making it not a viable option for younger patients.11,14,19,20,21,22 Galatz published one of the earliest series of arthroscopic rotator cuff repair for massive tears and determined that 94% resulted in repeated tears.3
Autografts, allografts, or synthetic implants have been used as an alternative treatment which can bridge the unrepairable rotator cuff tears, improving the biological and biomechanical environment at the repair site and thus becoming an extracellular matrix scaffold, which can stimulate and enhance the intrinsic healing potential of the patient.7,18,23 Furthermore, the matrix should be biocompatible in order to not be rejected and also the graft should be properly processed to avoid the risk of disease transmission or immune response.6 The results of the use of various grafts for rotator cuff repair are ambiguous, regarding surgical outcomes and complication rates.9,20
The present study describes the technique and functional outcome of massive irreparable rotator cuff tears using fascia lata as an allograft. We chose fascia lata, because it has been used successfully for many years for the reconstruction of human connective tissue in gynecologic, urologic and orthopedic surgical procedures.13,24 Furthermore, it is technically easy to perform and finally reduces the tension at the reconstruction site, which is the cause of postoperative retearing or joint stiffness.21
MATERIALS AND METHODS
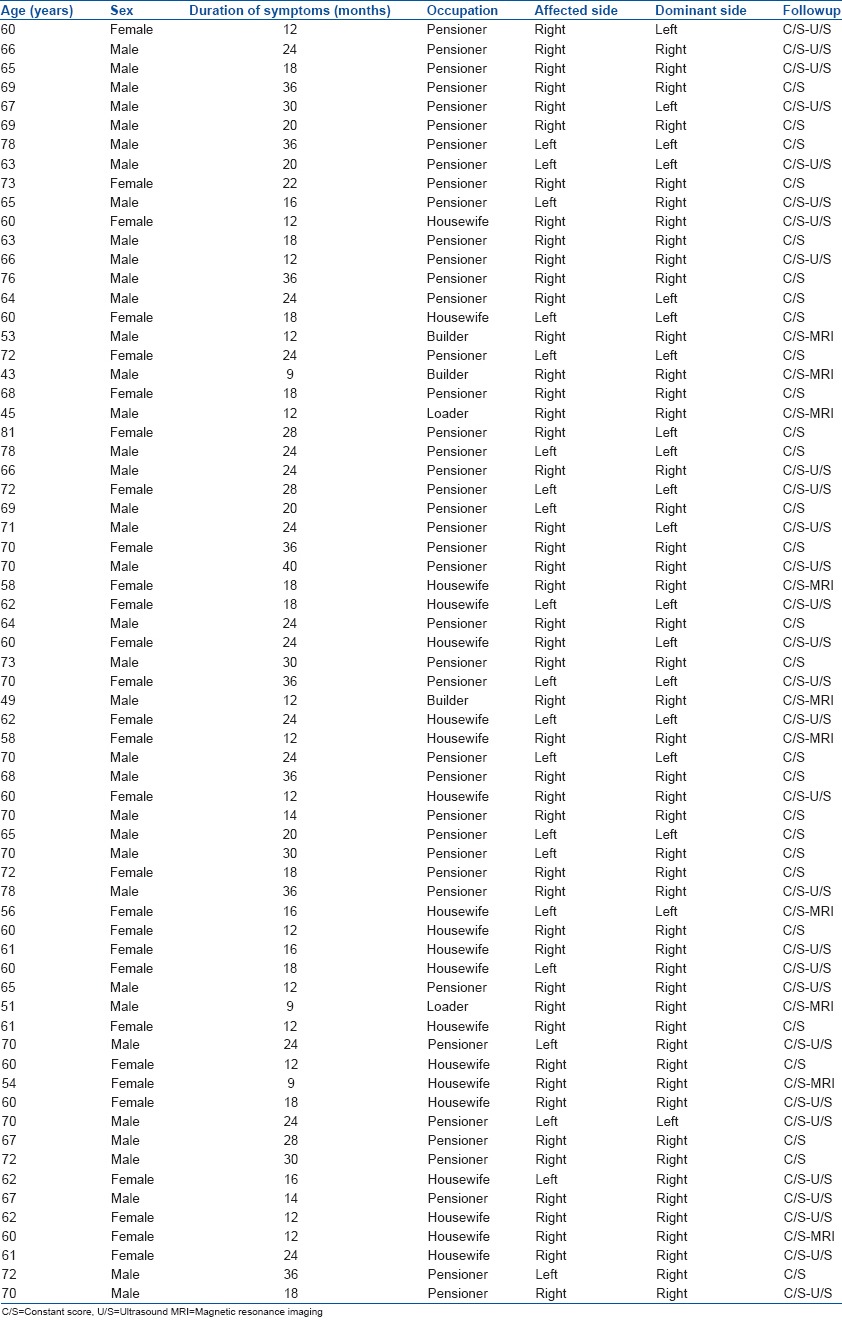
68 consecutive patients with massive irreparable rotator cuff tear operated between February 2006 and February 2010 were included in this prospective study. All the patients were operated covering the defect with fascia lata allograft. All procedures were performed by the same surgeon. The study group consisted of 38 men and 30 women, with average age of 64.9 years (range 43–81 years), who were followed up for a mean of 43 months (range 31–77 months). Operations were done within 48 right and 20 left shoulders, of which 55 were the dominant side and all were primary repairs and not revisions. The study included all patients which had at least two ruptured tendons, measuring more than 5 cm in maximal diameter, proven by MRI [Figure 1] and confirmed at the time of surgery, impossible to be reparable with simple suture, without producing tension at the repair site, even with release of the tendons. No patient was excluded who do not fulfill the above criteria except in patients suffering from advanced glenohumeral arthritis, because of stiffness which can develop in these patients. All tears that fixed in this way were 5–7 cm and the measurement performed at the time of surgery. The graft modified until match the respective tear each time. In our study, as far as muscular atrophy is concerned, all patients had retraction of the involved muscles with fatty replacement (three and above, by Goutallier score), observed in preoperative MRI. Patients were symptomatic, with pain, mainly nocturnal, and decreased function, despite all conservative treatment. Patients were evaluated with preoperative and postoperative constant score, as well as magnetic resonance imaging (MRI) and followup ultrasound examination.4,5 All patients were evaluated with preoperative, in 4 and 12 months postoperative constant score, 10 patients underwent MRI in 8 months postoperatively while 30 other patients underwent ultrasound in 12 months postoperatively. The remaining 28 patients were unwilling to undergo further testing because they were satisfied with the clinical outcome. However, all 68 patients were measured with a constant score preoperatively, 4 and 12 months postoperatively [Table 1].
Figure 1.
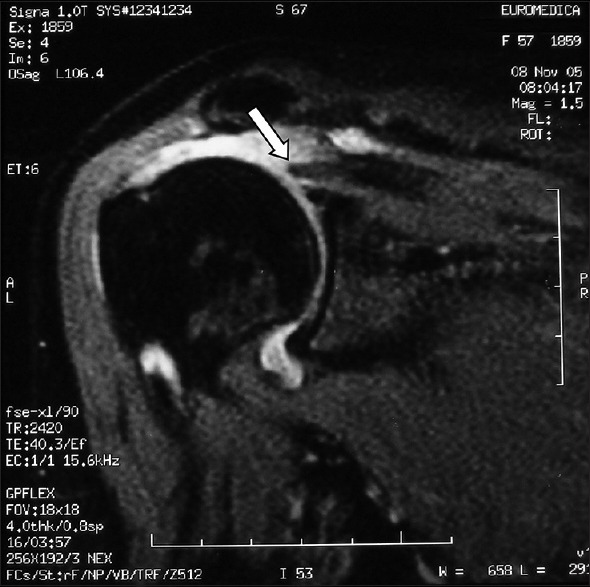
Preoperative coronal MR image demonstrates massive tear and proximal retraction (arrow) of the rotator cuff
Table 1.
Clinical details of patients
Operative procedure
Under general anesthesia, the patients were placed in the beach chair position. A lateral approach of the shoulder was performed followed by careful deltoid detachment from the anterior acromion. The edges of the involved tendons were then identified, debrided and mobilized by sequential releases (anterior and posterior) confirming that simple suture repair was impossible without excessive tension due to tendon retraction [Figure 2]. The greater tuberosity was then prepared with lightly shaving of its cortical bone. The size of the r-c tear was then measured, and the fascia lata allograft was hydrated in a sterile solution for 30 min and cut to the proper size according to the measurements. The source of the fascia lata allografts is cadaveric donors. The procurement, processing, and storage of these allografts is in accordance with the EU directives for human tissue and the standards set by the American Association of tissue banks and the Food and Drug Administration. Tissue derived by cadaveric donors has all the necessary approvals and consent for its further use as allograft. The allografts have been processed by Osteotech Inc., (A Medtronic Company) in the USA.
Figure 2.
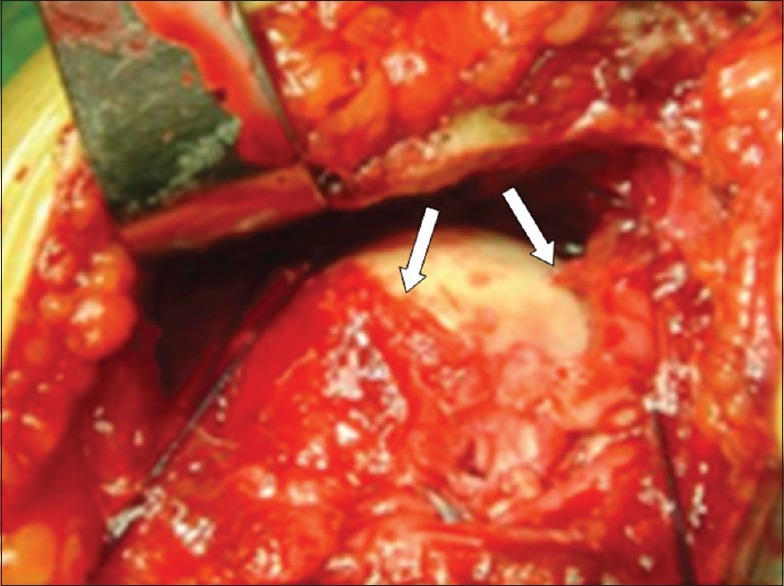
Intraoperative photograph showing an irreparable rotator cuff tear. Arrows mark the position of the two cut tendinous ends
The next step was to reduplicate the graft in three layers thickness, to reinforce it. We stabilized the final form of the patch inserting absorbable stitches (vicryl no. 2.0) [Figure 3].
Figure 3.
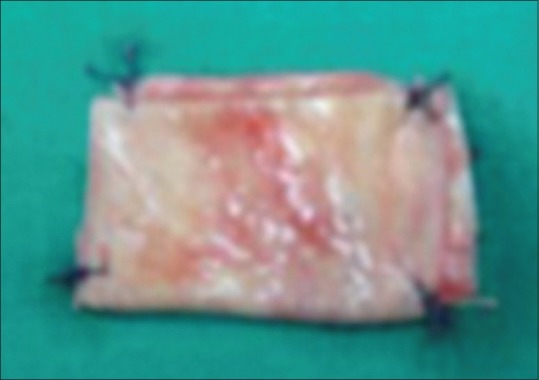
Peroperative clinical photograph showing final form of the graft
The graft was pushed down over the r-c defect and the medial side of the graft was sutured with the remaining r-c tissue medially with 6–8 stitches no. 2 Ethibond suture (Ethicon, Johnson and Johnson, Somerville, NJ), in such a way as the graft to overlap the remaining stump of the tendon and then was tensioned so that the lateral end of the fascia was attached on the footprint of the supraspinatus insertion to the greater tuberosity with five anchors loaded with no. 2 nonabsorbable suture (5.5 mm Lactoscrew Anchors, with Needles #2 Maxbraid (Lactosorb L-15 resorbable copolymer) (Sterile, EO; Biomet Inc.) [Figure 4], in order for the fascia lata to cover the area of repair completely and to be under slight tension. At the time of repair, the shoulder was in a neutral position regarding internal and external rotation and in 10–20° abduction. During the closure of the wound, it is very important for the postoperative outcome of the shoulder function the correct re-attachment of the deltoid back to the acromion via transosseous insertion with suture (PDS No. 1-Ethicon). All patients received three doses of intravenous antibiotics (cefazolin). The first dose 30 min before the procedure, the second dose 1 h after the surgery, and the last one 4 h later.
Figure 4.
Peroperative clinical photograph showing fixation of the graft
After surgery, the arm was maintained in a standard abduction pillow, for 6 weeks. The sling was removed for the 1st time 2 days after surgery for elbow, wrist, and hand active exercises. Pendulum exercises were started 3 weeks after surgery. The passive motion continued for a period of 6 weeks, after which patients were encouraged to progress gradually to active assisted motion and active motion. Finally, the strengthening started at 12 weeks, and the resistance exercises at 16 weeks and patients returned to activity as tolerated at 24 weeks.
RESULTS
Results were based on the assessment of two factors: The relief of pain and the degree of motion of the shoulder, as these were the most serious complaints reported preoperatively. Pain relief was the most dramatic benefit observed [Table 2] The constant score at 4 months is similar to that of 12 months and the difference in rates is not considerable.
Table 2.
Preoperative and 12 months postoperative assessment of pain, daily activities, ROM and strength of each patient based on C/S
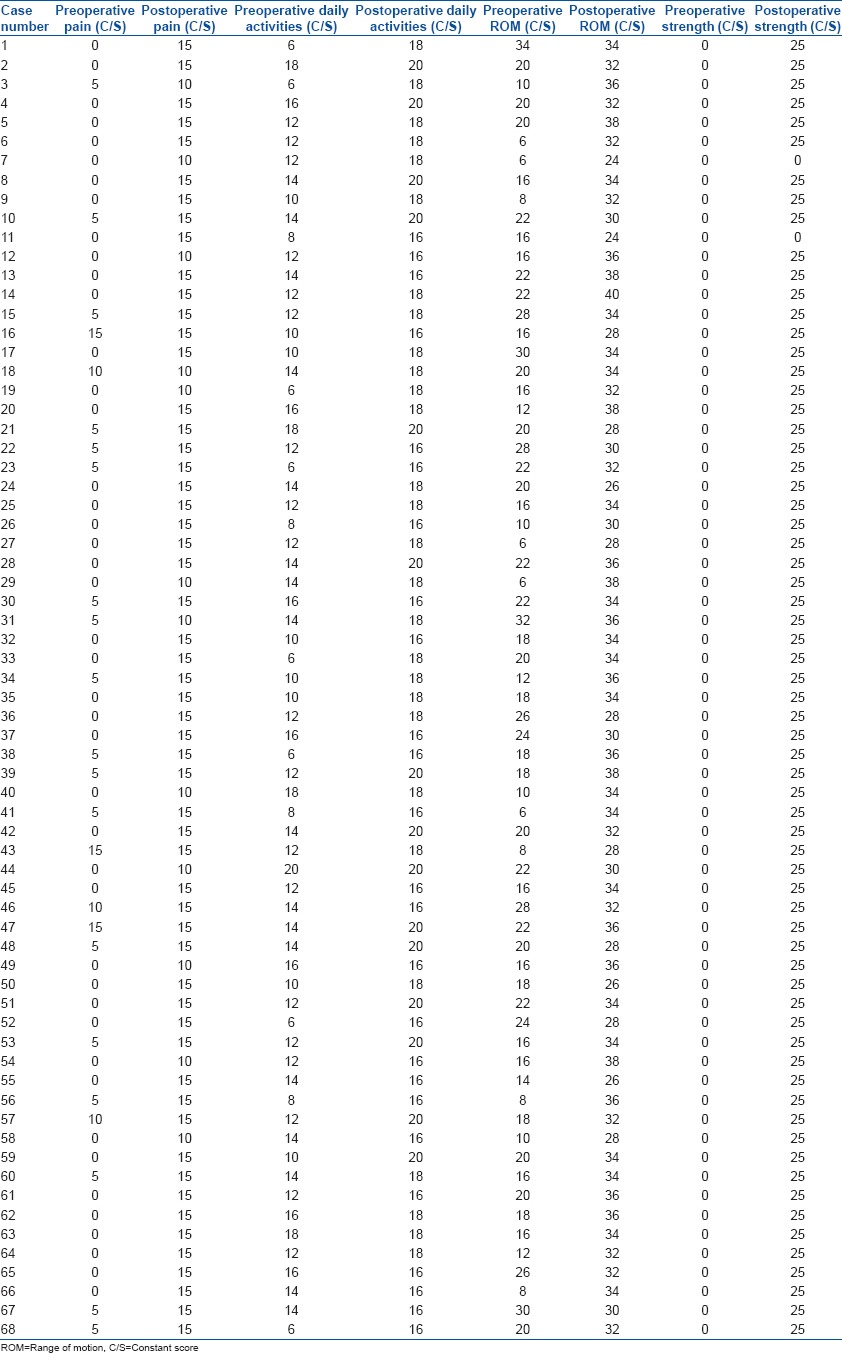
According to the constant score, the mean pain score improved from 2.4 to 14.1 postoperatively. Assessment based on total constant score revealed an improvement from 32.5 preoperatively to 88.7 postoperatively. The most significant improvements occurred in forward flexion which increased from 4.6 preoperatively to 8.5 postoperatively. Similar increments occurred in regards to abduction from 4.2 to 8.3, and to external rotation from 4.1 to 8.5, 12 months postoperatively [Table 3]. In all 10 patients who underwent a followup MRI, the results were confusing regarding the structural integrity of the graft due mainly to altering of the magnetic signal by the graft. On the other hand, of the other 30 patients who underwent ultrasound examination at the final followup in 12 months, 27 showed an intact graft, at the anatomical location of the r-c, without a new rupture at the repair site [Figure 5] and only in three patients there was a retear of the graft observed. The fatty infiltration observed in preoperative MRI, was not reversed based on MRI postoperatively. No intraoperative complications were noted in any patient.
Table 3.
Preoperative and 12 months postoperative absolute C/S of the shoulders
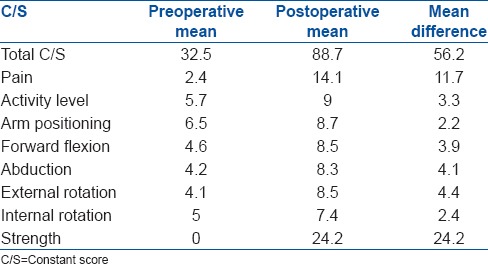
Figure 5.
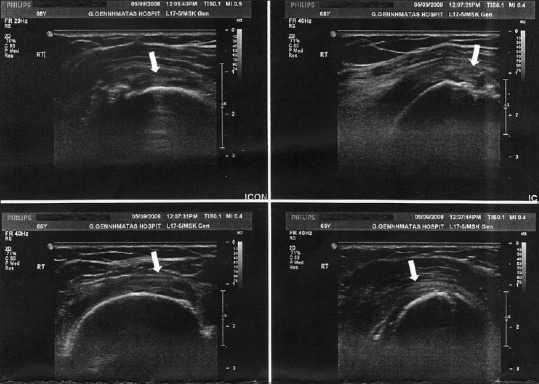
Postoperative ultrasound images showing intact rotator cuff graft (arrows)
DISCUSSION
Massive and irreparable r-c tears are not uncommon and consist of a difficult problem for orthopedic surgeons. Despite much investigation and many suggested treatments in the literature, there is still not a clear treatment option, for this kind of tear.1,20 The results of the methods used so far, such as debridement, partial repair or tendon transfers, do not seem to have good results as far as massive tears are concerned. Several studies, mainly in animal models, have evaluated the bridging of the irreparable r-c tear by graft and the results have a studying interest, because the outcomes are various. Specifically, Neviaser et al. in 1978, first reported poor results in 14 of 16 patients by use of a freeze-dried allograft to repair the r-c defect.25 Nasca reported only two satisfactory results in a series of 13 cases, utilizing the same materials and methods as Neviaser.20 Moore et al. reported complete radiographic failure of all 15 human allografts.5 while Galatz documented similar failures, but with improved pain and motion, despite residual tears documented on MRI.5,20 Dejardin reported that porcine small intestine submucosa (SIS) was an effective solution,22 while Sclamberg et al. evaluated the use of SIS which also showed disappointing results with clinical and MRI findings consistent with a retear in 10 out of 11 patients.2,11 Kimura et al. reported all specimens failed after use of polytetrafluoroethylene synthetic graft to address irreparable tears of the infraspinatus in dogs.26 Adams et al. presented an acellular human dermal allograft matrix to repair infraspinatus defects in dogs and they noted an almost normal tendon structure at the repair site.27 Finally, Sano et al. presented the use of fascial autograft to repair supraspinatus defects in rabbits and they found a normal tendon structure at 8 weeks, with histologic incorporation of the graft.10 Because of the good results of using fascia lata in animal models, we decided to use a fascia lata allograft to bridge the massive irreparable r-c tear in humans and to record the results.
The fascia lata is the deep fascia of the thigh, originating from the tensor fascia lata muscle and inserting into Gerdy's tubercle at the knee,24 and it has been used with success for other ligament or tendon reconstructions, having the ability to gradually remodel into a tendinous tissue, similar to a normal tendon.21 Moreover, based on its mechanical, chemical, and ultrastructural similarity to tendon, fascia lata has the advantage to be natural, strong, large, providing good suture retention and enhanced healing.24 The allograft is preserved with a proprietary freeze-drying method that retains its natural structure, is prehydrated, sterilized, but needs to be rinsed before using.17 Indications for use of the patch were a massive, irreparable r-c tear and/or significant fatty degeneration.18 A relative contraindication was advanced glenohumeral arthritis, because of stiffness which can develop in these patients.19 There are many factors that can affect the success of tissue grafting such as the properties of the graft material selected, the degree of muscle atrophy, tendon quality, rehabilitation protocol, use of nicotine or nonsteroidal antiinflammatory drugs and repair method.17 Burkhart et al. have suggested that lower r-c repair tension may provide less mechanoreceptor stimulation and therefore potentially less pain.28 In our study, as far as muscular atrophy is concerned, all patients had retraction of the involved muscles with fatty replacement (three and above, by Goutallier score), observed in preoperative MRI and confirmed at the time of surgery, which was not reversed based on MRI postoperatively.4,14 Preoperatively patients were symptomatic, with pain, mainly nocturnal and decreased ROM of the affected shoulder, being unable to perform their daily activities, hobbies and work. The postoperative evaluation of all patients that participated in our study, revealed significant improvement in scores, mainly in pain relief, nocturnal sleep without discomfort, but mainly patient's satisfaction, because they were able now to perform daily and leisure activities and finally a very good ROM, including flexion, abduction, internal and external rotation of their shoulder. A significant complication, such as infection or rejection of the graft was not evidenced, which confirms the biocompatibility of the fascia lata allograft. However, our study has some weaknesses. The postoperative MRI was of limited diagnostic quality, because of the relative poor resolution, without being able to assess clearly the graft integrity.13 Furthermore, many patients did not wish to undergo MRI because of their claustrophobia. Therefore, we believe that better quality MRI and the use of arthrography may offer more information about the grafts. There is much controversy in the orthopedic literature regarding the efficacy of MRI in the evaluation of postoperative shoulders and especially re-tears of the repair site with graft interposition4 On the other hand, ultrasound seems to be more accurate for graft interpretation, but not all patients willing to undergo further examinations, because they were satisfied with the clinical outcome. However, all 68 patients were measured with a constant score preoperatively, 4 and 12 months postoperatively, and the results were in line with their clinical status. In summary, based on the results of our study, it appears that fascia lata allograft used to repair the massive r-c tear acts as a substitute and may offer a useful tool in situations in which repair would be otherwise impossible, offering a different strategy in this intractable problem.10,12,17,24 The scaffold materials may provide initial mechanical and later biological support via its incorporation,23 as investigated in animal models, without any immune response and the morbidity of tendon transfers or arthroplasty.18,19
To conclude, based on results from our clinical study, we consider that fascia lata allograft is a viable and easy to perform treatment option in this complex, not uncommon problem of irreparable massive rotator cuff tears.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Warner JJ. Management of massive irreparable rotator cuff tears: The role of tendon transfer. Instr Course Lect. 2001;50:63–71. [PubMed] [Google Scholar]
- 2.Neri BR, Chan KW, Kwon YW. Management of massive and irreparable rotator cuff tears. J Shoulder Elbow Surg. 2009;18:808–18. doi: 10.1016/j.jse.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 3.Nho SJ, Delos D, Yadav H, Pensak M, Romeo AA, Warren RF, et al. Biomechanical and biologic augmentation for the treatment of massive rotator cuff tears. Am J Sports Med. 2010;38:619–29. doi: 10.1177/0363546509343199. [DOI] [PubMed] [Google Scholar]
- 4.Sclamberg SG, Tibone JE, Itamura JM, Kasraeian S. Six-month magnetic resonance imaging followup of large and massive rotator cuff repairs reinforced with porcine small intestinal submucosa. J Shoulder Elbow Surg. 2004;13:538–41. doi: 10.1016/j.jse.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 5.Bond JL, Dopirak RM, Higgins J, Burns J, Snyder SJ. Arthroscopic replacement of massive, irreparable rotator cuff tears using a GraftJacket allograft: Technique and preliminary results. Arthroscopy. 2008;24:403–9.e1. doi: 10.1016/j.arthro.2007.07.033. [DOI] [PubMed] [Google Scholar]
- 6.Cole BJ, Gomoll AH, Yanke A, Pylawka T, Lewis P, Macgillivray JD, et al. Biocompatibility of a polymer patch for rotator cuff repair. Knee Surg Sports Traumatol Arthrosc. 2007;15:632–7. doi: 10.1007/s00167-006-0187-6. [DOI] [PubMed] [Google Scholar]
- 7.Santoni BG, McGilvray KC, Lyons AS, Bansal M, Turner AS, Macgillivray JD, et al. Biomechanical analysis of an ovine rotator cuff repair via porous patch augmentation in a chronic rupture model. Am J Sports Med. 2010;38:679–86. doi: 10.1177/0363546510366866. [DOI] [PubMed] [Google Scholar]
- 8.Nicholson GP, Breur GJ, Van Sickle D, Yao JQ, Kim J, Blanchard CR. Evaluation of a cross-linked acellular porcine dermal patch for rotator cuff repair augmentation in an ovine model. J Shoulder Elbow Surg. 2007;16:S184–90. doi: 10.1016/j.jse.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 9.Derwin KA, Codsi MJ, Milks RA, Baker AR, McCarron JA, Iannotti JP. Rotator cuff repair augmentation in a canine model with use of a woven poly-L-lactide device. J Bone Joint Surg Am. 2009;91:1159–71. doi: 10.2106/JBJS.H.00775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aurora A, McCarron J, Iannotti JP, Derwin K. Commercially available extracellular matrix materials for rotator cuff repairs: State of the art and future trends. J Shoulder Elbow Surg. 2007;16:S171–8. doi: 10.1016/j.jse.2007.03.008. [DOI] [PubMed] [Google Scholar]
- 11.Ide J, Kikukawa K, Hirose J, Iyama K, Sakamoto H, Mizuta H. Reconstruction of large rotator-cuff tears with acellular dermal matrix grafts in rats. J Shoulder Elbow Surg. 2009;18:288–95. doi: 10.1016/j.jse.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 12.Malcarney HL, Bonar F, Murrell GA. Early inflammatory reaction after rotator cuff repair with a porcine small intestine submucosal implant: A report of 4 cases. Am J Sports Med. 2005;33:907–11. doi: 10.1177/0363546504271500. [DOI] [PubMed] [Google Scholar]
- 13.Badhe SP, Lawrence TM, Smith FD, Lunn PG. An assessment of porcine dermal xenograft as an augmentation graft in the treatment of extensive rotator cuff tears. J Shoulder Elbow Surg. 2008;17:35S–9. doi: 10.1016/j.jse.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 14.Audenaert E, Van Nuffel J, Schepens A, Verhelst M, Verdonk R. Reconstruction of massive rotator cuff lesions with a synthetic interposition graft: A prospective study of 41 patients. Knee Surg Sports Traumatol Arthrosc. 2006;14:360–4. doi: 10.1007/s00167-005-0689-7. [DOI] [PubMed] [Google Scholar]
- 15.Davidson PA, Rivenburgh DW. Rotator cuff repair tension as a determinant of functional outcome. J Shoulder Elbow Surg. 2000;9:502–6. doi: 10.1067/mse.2000.109385. [DOI] [PubMed] [Google Scholar]
- 16.Zalavras CG, Gardocki R, Huang E, Stevanovic M, Hedman T, Tibone J. Reconstruction of large rotator cuff tendon defects with porcine small intestinal submucosa in an animal model. J Shoulder Elbow Surg. 2006;15:224–31. doi: 10.1016/j.jse.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 17.Barber FA, Herbert MA, Coons DA. Tendon augmentation grafts: Biomechanical failure loads and failure patterns. Arthroscopy. 2006;22:534–8. doi: 10.1016/j.arthro.2005.12.021. [DOI] [PubMed] [Google Scholar]
- 18.Labbé MR. Arthroscopic technique for patch augmentation of rotator cuff repairs. Arthroscopy. 2006;22:1136.e1–6. doi: 10.1016/j.arthro.2006.03.022. [DOI] [PubMed] [Google Scholar]
- 19.Wong I, Burns J, Snyder S. Arthroscopic GraftJacket repair of rotator cuff tears. J Shoulder Elbow Surg. 2010;19:104–9. doi: 10.1016/j.jse.2009.12.017. [DOI] [PubMed] [Google Scholar]
- 20.Moore DR, Cain EL, Schwartz ML, Clancy WG., Jr Allograft reconstruction for massive, irreparable rotator cuff tears. Am J Sports Med. 2006;34:392–6. doi: 10.1177/0363546505281237. [DOI] [PubMed] [Google Scholar]
- 21.Sano H, Kumagai J, Sawai T. Experimental fascial autografting for the supraspinatus tendon defect: Remodeling process of the grafted fascia and the insertion into bone. J Shoulder Elbow Surg. 2002;11:166–73. doi: 10.1067/mse.2002.120808. [DOI] [PubMed] [Google Scholar]
- 22.Funakoshi T, Majima T, Suenaga N, Iwasaki N, Yamane S, Minami A. Rotator cuff regeneration using chitin fabric as an acellular matrix. J Shoulder Elbow Surg. 2006;15:112–8. doi: 10.1016/j.jse.2005.05.012. [DOI] [PubMed] [Google Scholar]
- 23.Snyder SJ, Arnoczky SP, Bond JL, Dopirak R. Histologic evaluation of a biopsy specimen obtained 3 months after rotator cuff augmentation with GraftJacket Matrix. Arthroscopy. 2009;25:329–33. doi: 10.1016/j.arthro.2008.05.023. [DOI] [PubMed] [Google Scholar]
- 24.Derwin KA, Aurora A, Iannotti JP. Allograft fascia lata as an augmentation device for musculoskeletal repairs. Conference Paper. Cleveland Clinic, Cleveland OH. Google–Article; Dec. 2008 [Google Scholar]
- 25.Neviaser JS, Neviaser RJ, Neviaser TJ. The repair of chronic massive ruptures of the rotator cuff of the shoulder by use of a freeze-dried rotator cuff. J Bone Joint Surg Am. 1978;60:681–4. [PubMed] [Google Scholar]
- 26.Kimura A, Aoki M, Fukushima S, Ishii S, Yamakoshi K. Reconstruction of a defect of the rotator cuff with polytetrafluoroethylene felt graft. Recovery of tensile strength and histocompatibility in an animal model. J Bone Joint Surg Br. 2003;85:282–7. doi: 10.1302/0301-620x.85b2.12823. [DOI] [PubMed] [Google Scholar]
- 27.Adams JE, Zobitz ME, Reach JS, Jr, An K-N, Steinmann SP. Rotator cuff repair using an acellular dermal matrix graft: An in vivo study in a canine model. Arthroscopy. 2006;22:700–9. doi: 10.1016/j.arthro.2006.03.016. [DOI] [PubMed] [Google Scholar]
- 28.Burkhart SS, Johnson TC, Wirth MA, Athanasiou KA. Cyclic loading of transosseous rotator cuff repairs: Tension overload as a possible cause of failure. Arthroscopy. 1997;13:172–6. doi: 10.1016/s0749-8063(97)90151-1. [DOI] [PubMed] [Google Scholar]


