Abstract
Background:
The incidence of acetabular fractures in India has increased over the past years but so has the operating skills of pelvi-acetabular trauma surgeons. The outcomes of surgical management need to be assessed so as to be able to devise proper treatment plan and execute the same during and after surgery, which in turn requires assessment of quality of life indices as well as functional scores. While there are studies assessing Harris Hip scores (HHS) and world health organization quality of life BREF (WHOQOL BREF) in the western population there is no study which assesses the same in Indian population. We designed this study to evaluate and define reference values for use of WHOQOL BREF Hindi scores in QOL Assessment in patients with acetabular fractures and to assess the relationship between it and HHS.
Materials and Methods:
118 patients with acetabular fractures who were treated surgically were included in this retrospective study. Assessment of reduction quality (Matta's radiological criteria), clinical outcome (HHS) and functional outcome (WHOQOL-BREF score) were done. The affect of age, gender, fracture displacement, hip dislocation, delay in surgery and associated injury on the clinical and functional outcome was evaluated.
Results:
The mean HHS was 90.65 (42–100) which showed an overall good to excellent outcome in 78.8% cases. WHOQOL-BREF Hindi score of domain-one was 63.06 ± 20.31 (13–94), of domain-two was 58.22 ± 19.57 (13–100), of domain-three was 70.49 ± 17.92 (13–100) and of domain-four was 64.48 ± 18.46 (13–100), which showed significant functional deficit in domain-one (P = 0.0001) and domain-two (P = 0.0001) but not in domain-three (P = 0.458) and domain-four (P = 0.722) when compared to score of general healthy population. The domain scores of general population norms were achieved in 59.3%, 61.9%, 69.5% and 66.1% cases in domain one, two, three and four respectively.
Conclusions:
Based on these results one can conclude that WHOQOL-Hindi questionnaire is good enough for assessment of QOL in addition to clinical measures in acetabular fracture patients.
Keywords: Acetabular fractures, Matta's radiological criteria, Merle d’Aubgne and Harris hip score, World Health Organization quality of life-BREF Hindi score
MeSH terms: Hip, acetabulum, fracture, quality of life
INTRODUCTION
Quality of life (QOL) is becoming an important component of overall assessment in health care setting so the clinical outcome measures (Merle d’Aubgne and Harris hip score [HHS]) should be accompanied by a functional outcome assessment that focuses on the whole individual from the patient's point of view, and these QOL parameters provides measurement of functioning and well-being rather than of diseases and disorders.1,2,3,4
Over past decade various functional scoring systems have been used for acetabular fracture patients (Musculoskeletal Function Assessment score, short form (SF)-36, SF-12 score, EQ-5D score and World Health Organization-QOL (WHOQOL) score5,6,7,8,9,10,11,12,13 but most were devised in the developed countries and their cross-cultural compatibility has not been demonstrated.14 Quality of life assessment is extremely rare in India and one of the important reasons for this is nonavailability of a suitable instrument.14
The WHOQOL-BREF arises from 10 years of development research on QOL and health care. It is a person centered, multilingual instrument for subjective assessment and is designed for generic use as a multidimensional profile, so enabling a wide range of diseases and conditions to be compared and it is a cross-culturally valid assessment of well-being, as reflected by its four domains: Physical, psychological, social and environmental14,15,16,17,18 and its Hindi version, The WHOQOL-Hindi appears to be a suitable instrument for comprehensively evaluating the QOL in health care settings in India.14,15
Because of increasing trend toward using functional outcome scores beside the clinical scores in outcome analysis of acetabular fractures, the present study was designed to provide needed experience and to put reference values for use of WHOQOL-BREF Hindi score in QOL assessment in patients with acetabular fractures and to analyze the dependence of the clinical and functional outcome on multiple factors, including age, sex, the degree of initial displacement, fracture pattern, delay in surgery, and quality of the reduction, which were known to affecting the clinical outcomes.
MATERIALS AND METHODS
159 skeletally mature patients with acetabular fractures treated surgically in our institution between 1998 and 2010 by a single surgeon (RKS) were called. All patients were called for followup for research purpose. A total 135 patients came for followup, patients whose preoperative X-rays were not available and patients with <2 year followup were excluded from the study and hence 118 patients left for outcome analysis. Of these ten patients had undergone total hip replacement and were included in poor clinical and functional outcome groups. Data regarding the demographic profile, mechanism of injury, associated injuries, delay in surgery (categorized as <2 weeks or more than 2 weeks) were obtained.
On the basis of age, patients were classified into two groups (55 years or less and more than 55 years). To assess the effect of initial displacement, fractures were also categorized in two groups (less or equal to 20 mm or more than 20 mm).
Preoperative radiographs, including anteroposterior and Judet views, as well as computerized tomography scans, were obtained to assess and classify all fractures according to the classification of Judet et al.19
Assessment of reduction quality was done in immediate postoperative radiograph by using Matta's radiological criteria3 and reduction was classified into three groups; anatomical, congruent and incongruent on the basis of displacement of femoral head arc and acetabular arc in the region of weight bearing dome. The reduction was categorized as anatomical if all fracture gaps and steps had been corrected intraoperatively and postoperative films showed restoration of all five anatomical lines (ilio-inguinal, ilio-pectineal, dome, posterior wall and anterior wall) with the head centered and parallel beneath the acetabular roof. A congruent reduction is best judged on the anteroposterior film, which is useful in assessing the hip with reference to both the congruency and anatomy of the contralateral normal joint. Patients with poor restoration of the five pelvic lines, inward subluxation of the hip and loss of parallelism were included in the incongruent group.
Analysis of clinical outcome was done by using HHS (0–100). The results were categorized as excellent 90–100, good 80–89, fair 70–79 and poor if <70. These were further compiled into 2 groups (good to excellent and poor to fair) for clinical outcome assessment.
The WHOQOL-BREF Hindi questionnaires were completed by patients themselves after they had received required instructions. Patients with more than 20% missing values were excluded from the analysis according the rule of the WHOQOL Group (the WHOQOL Group, 1995; World Health Organization, 1996).
The obtained raw score was converted in transformed score by using SPSS syntax, which directly converts the raw score into transformed domains score (the scores are transformed on a scale from 0 to 100 to enable comparisons to be made between domains composed of unequal numbers of items). Due to the unavailability of appropriate reference values, we compared our results with general population norms.15
Statistical analysis
We used SPSS software (version 20, SPSS Inc., Chicago, IL, USA). Descriptive statistics (mean, standard deviation, skewness, and kurtosis etc.) were used to describe the patients’ variables and clinical and functional outcomes. The relationship of the functional outcome was analyzed and related to the fracture pattern, the time gap between injury and surgery and quality of reduction. Summary statistics (mean, standard deviation, skewness, and kurtosis etc.) were used to describe the clinical characteristics and functional and radiological outcome. Bi-variate association was studied using Pearson Chi-square test. Various comparisons were made either using t-test or analysis of variance.
RESULTS
Of the 159 patients, 41 patients were excluded from the study because of lack of followup more than 2 years and unavailability of complete data. So a total of 118 patients were included in the study.
It was observed that acetabular injuries were predominantly affecting the younger individuals; with a mean age of 38.75 ± 13.6 years (range 17–65 years). There was a male preponderance 99 (83.9%). 59 patients had acetabular fractures of the right side, 56 patients had fracture of the left side while 3 patients had bilateral acetabular fractures. Most common mode of injury was road side accident (n = 99). While in 58 cases, the acetabular fracture was the only injury sustained, 32 cases had associated lower limb with or without pelvic injuires. Sciatic nerve injury was seen in 10 patients. Average delay in surgery was 10.82 days (range 1–90 days), delay in admission and associated injuries were a major contributor to this delay.
The mean HHS was 90.65 (42–100) of available 108 patients (we excluded 10 total hip replacement patients). Of these patients excellent outcome was seen in 62.7% cases while good, fair and poor outcomes were seen in 16.1%, 6.8% and 14.4% of cases respectively.
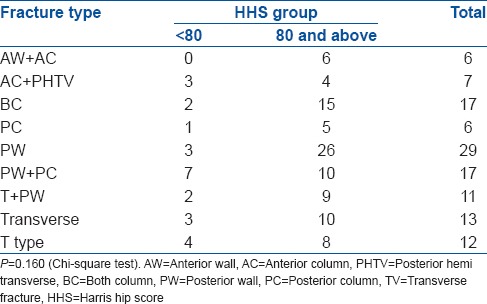
The clinical outcome was significantly affected by the degree of initial displacement (P = 0.001), presence of dislocation at the time of initial injury (P = 0.0001), presence of associated injuries (P = 0.046), delay in surgery (P = 0.003) and quality of reduction (P = 0.002) but not by age (P = 0.550), sex (P = 0.080) and fracture type (P = 0.160) [Tables 1 and 2].
Table 1.
Factors affecting clinical outcome
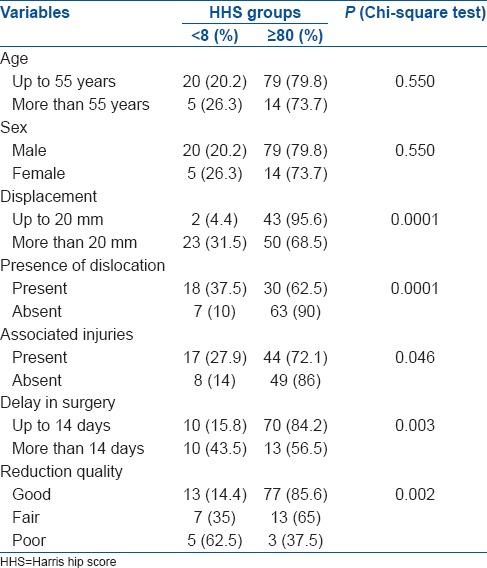
Table 2.
Distribution of HHS in different fracture type
On analysis of functional outcome using WHOQOL-BREF Hindi questionnaire, the mean score of domain one was 63.06 (range 13-94; SD 20.31), of domain two was 58.22 (range 13-100; SD 19.57), of domain three was 70.49 (range 13-100; SD 17.92) and of domain four was 64.48 (range 13-100; SD 18.46), which showing significant functional deficit in domain one (P = 0.0001) and domain two (P = 0.0001) but not in domain three (P = 0.458) and domain four (P = 0.722) when compared to score of general healthy population.15 The Domain scores of General population norms were achieved in 59.3, 61.9, 69.5 and 66.1% cases in domain one, two, three and four respectively.
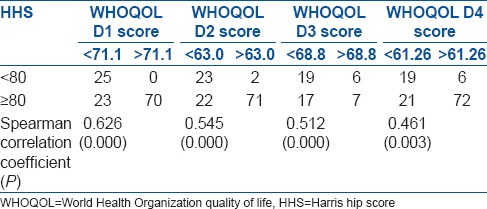
On analyzing the factors affecting the functional outcome, it was observed that the presence of dislocation, degree of initial displacement, associated injuries, and delay in surgery and reduction quality was significant variables [Tables 3 and 4]. On comparison of functional outcome by WHOQOL score with HHS, strong correlation [Table 5].
Table 3.
Factors affecting WHOQOL-BREF Hindi score
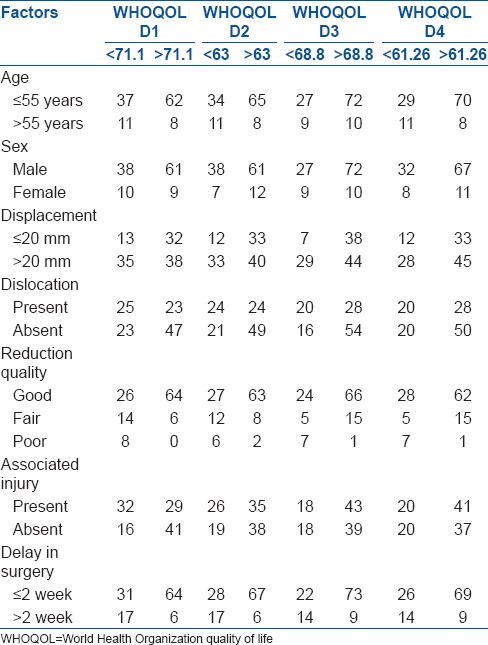
Table 4.
WHOQOL-BREF domains score in different type of fractures
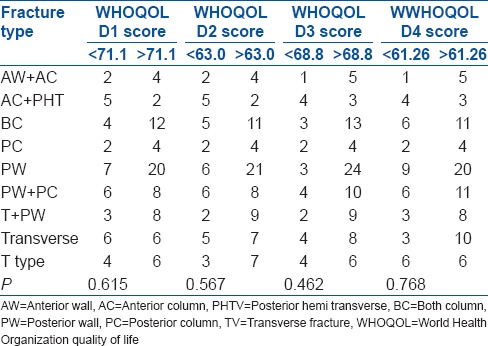
Table 5.
Distribution of WHOQOL-BREF score domains in two HHS groups
Another aspect which needs to be considered is that 17 (14.4%) cases had a poor clinical result, and ten of these had been converted into total hip arthroplasty. Remaining seven patients had not had an additional operation at the time of writing but had been offered a total hip replacement or arthrodesis.
DISCUSSION
Increasingly, health care planners recognize that measures of disease alone are insufficient determinants of health status. Over the past few decades, two classes of complementary health status measures have emerged to fill the information gap – objective measures of functional health status and subjective measures of health and well being. These measures are multilevel and multi dimensional. There are many published QOL measures, but there is still a lack of consensus among researchers about its definition and this is reflected in the choice of items for their instruments.1 In measuring QOL. Therefore, the WHOQOL Group takes the view that it is important to know how satisfied or bothered people are by important aspects of their life and this interpretation will be a highly individual matter. WHOQOL assessment – the WHOQOL-score is a cross-culturally valid assessment of well-being and is available in most of the words major languages.20
This study had evaluated the functional outcome scores beside the clinical scores for QOL assessment using WHOQOL-BREF Hindi score in acetabular fractures outcome assessment because and it showed its competence in the assessment of patients with hip fracture. Previously, Yao et al.21 have shown the usefulness of hip specific items in quality of life questionnaire for patients with hip fractures.
Our study has analyzed data from a well-defined catchment population over a period of 14 years in order to evaluate medium to long term clinical and functional outcome of operatively treated acetabular fractures by a single surgeon (RKS) at a tertiary referral center.
Demographic profile, injury profile, fracture types, surgical approaches and clinical outcome of our study were found comparable to other previous large studies.12,13,19,22,23
Assessment of clinical outcome was done with the use of HHS, which indicate good to excellent clinical outcomes similar to previous studies3,13 favoring operative treatment as the gold standard for displaced acetabular fractures. The HHS in our study was good or excellent in 78.8% cases and poor or fair in 21.2% cases. These results are comparable to those of Giannoudis et al.,13 in which the HHS was graded as good or excellent in 73.2% cases and poor or fair in 26.8% cases.
Comparison with previously published series by Matta et al.,3 Mayo et al,23 Madhu et al.24 and Briffa et al.25 clearly shows that clinical results, duration of followup and number of patients in present series is adequate to make useful assessments regarding clinical and functional outcome in patients with acetabular fractures. Even though the number of cases reported by Matta et al.3 and Madhu et al.24 is higher than that reported by us, the followup duration and the outcomes are almost identical.
On analysis of factors affecting clinical outcomes, we observed that presence of dislocation, degree of initial displacement, associated injuries, delay in surgery and quality of reduction were the main determinant of clinical outcome and these were comparable with previous studies.3,7,13,20,23,26
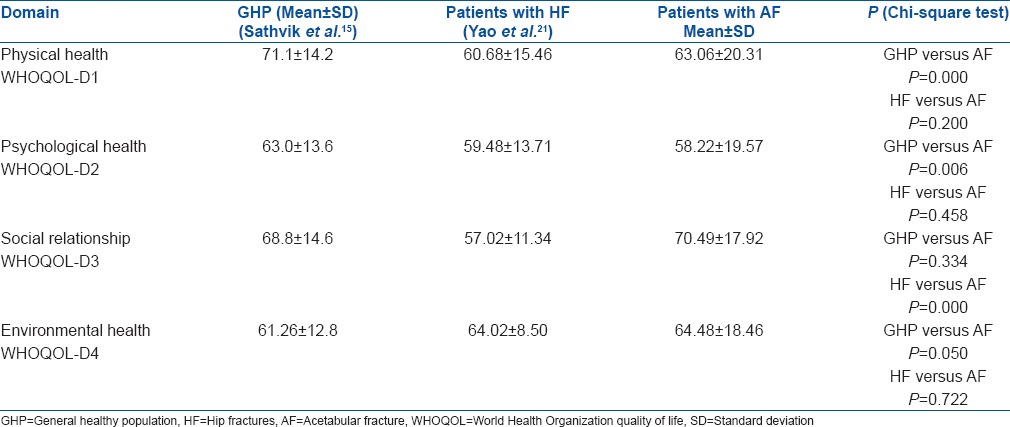
In our study the mean WHOQOL-BREF domain one, domain two, domain three and domain four score were 63.06 ± 20.31, 58.22 ± 19.57, 70.49 ± 17.92 and 64.48 ± 18.46 respectively, showing lack in physical (domain one) and psychological (domain two) scores but not in social (domain three) and environmental (domain four) scores when compared to general population norms [Table 6].15 Our results were comparable to the results of fracture around hip in the study by Yao et al.21 in all domains except in the social domain in which our results were significantly better than theirs [Table 6]. Domain scores of General population norms were achieved in 59.3, 61.9, 69.5 and 66.1% cases in domain one, two, three and four respectively, indicating positive functional outcome and making these patients as a functional member of society and supporting operative treatment for displaced acetabular fractures.
Table 6.
Comparison of WHOQOL-BREF domains score of GHP and patients with HF with AF patients
There are a few limitations of our study and we believe that they include the retrospective study design, attrition on followup and nonblinded assessors at followup.
Based on these results one can conclude that WHOQOL-Hindi questionnaire is good enough for the assessment of QOL in addition to clinical measures in acetabular fracture patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Skevington SM, Lotfy M, O’Connell KA, WHOQOL Group. The World Health Organization's WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res. 2004;13:299–310. doi: 10.1023/B:QURE.0000018486.91360.00. [DOI] [PubMed] [Google Scholar]
- 2.Letournel E. Acetabulum fractures: Classification and management. Clin Orthop Relat Res. 2004;13:299–310. [PubMed] [Google Scholar]
- 3.Matta JM. Fractures of the acetabulum: Accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78:1632–45. [PubMed] [Google Scholar]
- 4.Mears DC, Velyvis JH, Chang CP. Displaced acetabular fractures managed operatively: Indicators of outcome. Clin Orthop Relat Res. 2003:173–86. doi: 10.1097/00003086-200302000-00026. [DOI] [PubMed] [Google Scholar]
- 5.Engelberg R, Martin DP, Agel J, Obremsky W, Coronado G, Swiontkowski MF. Musculoskeletal function assessment instrument: Criterion and construct validity. J Orthop Res. 1996;14:182–92. doi: 10.1002/jor.1100140204. [DOI] [PubMed] [Google Scholar]
- 6.Engelberg R, Martin DP, Agel J, Swiontkowski MF. Musculoskeletal function assessment: Reference values for patient and non-patient samples. J Orthop Res. 1999;17:101–9. doi: 10.1002/jor.1100170116. [DOI] [PubMed] [Google Scholar]
- 7.Moed BR, Yu PH, Gruson KI. Functional outcomes of acetabular fractures. J Bone Joint Surg Am. 2003;85-A:1879–83. doi: 10.2106/00004623-200310000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Saterbak AM, Marsh JL, Nepola JV, Brandser EA, Turbett T. Clinical failure after posterior wall acetabular fractures: The influence of initial fracture patterns. J Orthop Trauma. 2000;14:230–7. doi: 10.1097/00005131-200005000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Borrelli J, Jr, Ricci WM, Anglen JO, Gregush R, Engsberg J. Muscle strength recovery and its effects on outcome after open reduction and internal fixation of acetabular fractures. J Orthop Trauma. 2006;20:388–95. doi: 10.1097/00005131-200607000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Engsberg JR, Steger-May K, Anglen JO, Borrelli J., Jr An analysis of gait changes and functional outcome in patients surgically treated for displaced acetabular fractures. J Orthop Trauma. 2009;23:346–53. doi: 10.1097/BOT.0b013e3181a278cc. [DOI] [PubMed] [Google Scholar]
- 11.Kreder HJ, Rozen N, Borkhoff CM, Laflamme YG, McKee MD, Schemitsch EH, et al. Determinants of functional outcome after simple and complex acetabular fractures involving the posterior wall. J Bone Joint Surg Br. 2006;88:776–82. doi: 10.1302/0301-620X.88B6.17342. [DOI] [PubMed] [Google Scholar]
- 12.Magill P, McGarry J, Queally JM, Morris SF, McElwain JP. Minimum ten-year follow-up of acetabular fracture fixation from the Irish tertiary referral centre. Injury. 2012;43:500–4. doi: 10.1016/j.injury.2011.12.028. [DOI] [PubMed] [Google Scholar]
- 13.Giannoudis PV, Nikolaou VS, Kheir E, Mehta S, Stengel D, Roberts CS. Factors determining quality of life and level of sporting activity after internal fixation of an isolated acetabular fracture. J Bone Joint Surg Br. 2009;91:1354–9. doi: 10.1302/0301-620X.91B10.22572. [DOI] [PubMed] [Google Scholar]
- 14.Saxena S, Chandiramani K, Bhargava R. WHOQOL-Hindi: A questionnaire for assessing quality of life in health care settings in India. World Health Organization Quality of Life. Natl Med J India. 1998;11:160–5. [PubMed] [Google Scholar]
- 15.Sathvik BS, Parthasarathi G, Narahari MG, Gurudev KC. An assessment of the quality of life in hemodialysis patients using the WHOQOL-BREF questionnaire. Indian J Nephrol. 2008;18:141–9. doi: 10.4103/0971-4065.45288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pacian A, Kulik TB, Pacian J, Chrusciel P, Zolnierczuk-Kieliszek D, Jarosz MJ. Psychosocial aspect of quality of life of Polish women with breast cancer. Ann Agric Environ Med. 2012;19:509–12. [PubMed] [Google Scholar]
- 17.Khosravi A, Ramezani MA, Toghianifar N, Rabiei K, Jahandideh M, Yousofi A. Association between hypertension and quality of life in a sample of Iranian adults. Acta Cardiol. 2010;65:425–30. doi: 10.2143/AC.65.4.2053901. [DOI] [PubMed] [Google Scholar]
- 18.de Oliveira PP, Sandrin CC, Batista PH, Marinheiro LP, Wender MC, Roisenberg F. Relationship between quality of life and vertebral fracture in older women living in Southern Brazil. Rev Bras Ginecol Obstet. 2011;33:231–7. [PubMed] [Google Scholar]
- 19.Judet R, Judet J, Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction. Preliminary report. J Bone Joint Surg Am. 1964;46:1615–46. [PubMed] [Google Scholar]
- 20.The World Health Organization Quality of Life assessment (WHOQOL): Position paper from the World Health Organization. Soc Sci Med. 1995;41:1403–9. doi: 10.1016/0277-9536(95)00112-k. [DOI] [PubMed] [Google Scholar]
- 21.Yao KP, Lee HY, Tsauo JY. Are hip-specific items useful in a quality of life questionnaire for patients with hip fractures? Int J Rehabil Res. 2009;32:245–50. doi: 10.1097/MRR.0b013e32832bb10c. [DOI] [PubMed] [Google Scholar]
- 22.Laird A, Keating JF. Acetabular fractures: A 16-year prospective epidemiological study. J Bone Joint Surg Br. 2005;87:969–73. doi: 10.1302/0301-620X.87B7.16017. [DOI] [PubMed] [Google Scholar]
- 23.Mayo KA. Open reduction and internal fixation of fractures of the acetabulum. Results in 163 fractures. Clin Orthop Relat Res. 1994:31–7. [PubMed] [Google Scholar]
- 24.Madhu R, Kotnis R, Al-Mousawi A, Barlow N, Deo S, Worlock P, et al. Outcome of surgery for reconstruction of fractures of the acetabulum. The time dependent effect of delay. J Bone Joint Surg Br. 2006;88:1197–203. doi: 10.1302/0301-620X.88B9.17588. [DOI] [PubMed] [Google Scholar]
- 25.Briffa N, Pearce R, Hill AM, Bircher M. Outcomes of acetabular fracture fixation with ten years’ followup. J Bone Joint Surg Br. 2011;93:229–36. doi: 10.1302/0301-620X.93B2.24056. [DOI] [PubMed] [Google Scholar]
- 26.Meena UK, Tripathy SK, Sen RK, Aggarwal S, Behera P. Predictors of postoperative outcome for acetabular fractures. Orthop Traumatol Surg Res. 2013;99:929–35. doi: 10.1016/j.otsr.2013.09.004. [DOI] [PubMed] [Google Scholar]


