Abstract
Health care transition (HCT) from pediatric to adult-focused systems is a key milestone for youth. Developing self-care skills and HCT planning are key elements. In a survey at 4 pediatric specialty clinics to 79 youth aged 16 to 25 years and 52 parents, skill-based HCT readiness was assessed using the Transition Readiness Assessment Questionnaire (TRAQ). Multivariable logistic regression evaluated the association between TRAQ scores and self-care beliefs. In all, 70% of youth and 67% of parents believed that they/their child could manage their care. Only 38% of youth and 53% of parents reported thinking about HCT; only 18% of youth and 27% of parents reported having a HCT plan. Youth with higher TRAQ scores were more likely to believe they could manage their care, controlling for age and gender (adjusted odds ratio = 4.0, 95% confidence interval = 1.7–9.5). Transition readiness skills are associated with self-care beliefs. However, a mismatch exists between high reported self-care beliefs and low levels of transition planning.
Keywords: health care transition, adolescent
Introduction
Many more adolescents with chronic medical conditions of childhood onset are now surviving into adulthood.1 As a result, health care transition (HCT), broadly defined as the process of shifting from pediatric to adult-focused care, is an increasingly important issue facing the health care system.2 The process of preparing such youth for the eventual move to adult health care often starts in early adolescence and requires individualized planning and ongoing skills development.3–5 Despite efforts to improve HCT over the past decade, national surveys of parents and youth have repeatedly shown that HCT planning is often lacking.6,7
Clinical guidelines for HCT call for routine use of structured transition readiness assessments and development of transition care plans.5 Preparation for HCT is a challenge because the youth's expected role in disease self-management often increases during a period of heightened developmental and psychosocial risk. In addition to specific self-care skills, the HCT process needs to empower youth to develop confidence in their abilities to manage their health care. For many youth, HCT is challenging because of a variety of factors, including emotional and cognitive development, lack of social supports, increased behavioral risks inherent to adolescence, poor coordination of care between pediatric and adult health systems, and gaps in health insurance at the age of transition.8–10 In addition, there often are differences between the concerns and beliefs of parents and youth around issues of self-care skill building and planning for the future.11 In particular, youth may be overconfident and overestimate skills, or conversely, parents may under-estimate their child's abilities.
In developmental terms, an increased confidence in self-care should translate into action through a set of skills indicating transition readiness. As such, many HCT programs have developed mechanisms to actively support and teach youth transition readiness skills.5,12 However, it is not known whether HCT readiness skills and belief in one's ability to manage one's care correlate. Since building skills and boosting confidence may require different types of instruction and coaching within an HCT preparation program, understanding this association is important. Similarly, it is not clear whether skill building occurs in parallel with clinical discussions around preparation for eventual transfer of care in adulthood.
In this study, we sought to understand associations among self-care beliefs, HCT readiness skills, and reports of HCT preparation among adolescents/young adults receiving care from an adolescent-focused or pediatric specialty care clinic. We investigated these constructs as reported by patients and by parents of patients, measuring concordance between parent and youth reports, and associations among beliefs about self-management, skill-based measures of readiness and preparation for HCT. We hypothesized that youth with higher levels of HCT readiness skills would be more likely to report believing they could manage their own care.
Methods
Study Sample and Measures
Subjects were English-speaking patients or parents of a youth aged 16 to 25 years receiving care at 1 of 4 specialty clinics at Boston Children's Hospital (BCH): Adolescent Medicine, Cystic Fibrosis, Diabetes, and Myelodysplasia/Spina Bifida. The Boston Children's Hospital Institutional Review Board reviewed and approved the study.
Study data are aggregated from 2 surveys administered to Boston Children's Hospital patients and parents of patients between 2009 and 2011. Survey 1 was given to a convenience sample of 36 youth and 21 parents who were participating in narrative research on patient-centered health information technology (response rate 100%). Survey 2 was given to 74 respondents (43 patient and 31 parents), recruited through targeted mailings and in-clinic outreach (response rate 34.9%). We pooled data from surveys 1 and 2, for a total sample of 79 youth and 52 parents, including a subset of 32 youth-parent dyads. Basic demographic information (age, sex, and race) on survey 2 nonrespondents was collected through medical chart review.
Transition Readiness
The core of both surveys was the Transition Readiness Assessment Questionnaire (TRAQ),13 a validated 29-item scale that measures skills involved in HCT. Following survey 1, we removed 6 items from the original TRAQ that had little variability within and across youth-parent groups, using a modified TRAQ with 23 items for survey 2. All parents were surveyed using TRAQ questions with language modified to elicit reports about their child's skills.
Transition Readiness Assessment Questionnaire response categories were scaled 1 to 5, with higher numbers corresponding to higher transition readiness for each individual skill (1 = I do not know how to do this, 2 = I do not know how, but I want to learn, 3 = I am learning how to do this, 4 = I have started doing this, 5 = I always do this when I need to), consistent with prior validation efforts.13 We averaged TRAQ responses across the 23 questions common to both surveys to create a total average TRAQ score for each respondent.
Self-Care Beliefs, HCT Preparation, and Health Information Sources
Both surveys contained yes/no questions about beliefs regarding self-care readiness. For youth, the question read: “Do you think you could manage your health care mainly on your own?” and this wording was modified in the parent survey to elicit reports about their belief their child could manage their care mainly on their own. Survey 2 was expanded to include additional items about specific HCT preparation, including questions concerning experience thinking about changing primary and specialty care, discussing transition with the health care team, and developing a plan for transitioning care. All survey respondents were asked to report on their primary sources of health information, including parents/doctors and outside sources such as books, Web sites, or other patients.
Data Analysis
We used descriptive statistics to characterize the demographics of the study population. Comparisons of study respondents against nonrespondents to the second administration of the survey, and of transition readiness by demographics were calculated using the χ2 test, and the 2-sample t test. Correlation and analysis of variance were used to compare TRAQ scores across patient/parent groups. Comparisons of TRAQ scores for patient/ parent dyads were performed using the paired t test. Multivariable logistic regression was used to examine associations between TRAQ score and patient/parent global beliefs about patient self-care abilities. In the model, TRAQ score was included as a continuous variable. The dependent variables for the analyses were the dichotomized responses to the questions on self-care beliefs and transition preparation activities. All models were adjusted for respondent age and gender. All analyses were performed in SAS version 9.3.
Results
Demographics and Health Information
Mean respondent age was 19.8 years (SD = 2.8 years) and did not differ by clinic; 72.4% were female (Table 1). There were no differences in age or gender between youth with and without an enrolled parent/guardian. There were no nonresponders for survey 1; for Survey 2, respondents did not differ from nonresponders in terms of age or race but were more likely to be female.
Table 1.
Youth Respondent Characteristics and Sources of Health Information.
| Total Sample; n (%) | Survey 1; n (%) | Survey 2; n (%) | |
|---|---|---|---|
| Total | 79(100.0) | 36 (45.6) | 43 (54.4) |
| Demographics | |||
| Average age in years (SD) | 19.8(2.8) | 19.5(2.9) | 20 (2.6) |
| Female | 55 (72.4) | 27 (75) | 28 (70) |
| White racea | – | – | 29 (76.3) |
| Clinic | |||
| Adolescent | 19(24.1) | 3 (8.3) | 16(37.2) |
| Cystic fibrosis | 18(22.8) | 13(36.1) | 5(11.6) |
| Diabetes | 29 (36.7) | 16 (44.4) | 13 (30.2) |
| Myelodysplasia | 13(16.5) | 4(11.1) | 9 (20.9) |
| Sources of health information | |||
| Doctor | 70 (88.6) | 36(100) | 34 (85.0) |
| Parents | 46 (60.5) | 20 (55.6) | 26 (65.0) |
| Web sites | 34 (44.7) | 18(50.0 | 16 (40.0) |
| Materials from health care provider | 29 (38.2) | 14(38.9) | 15(37.5) |
| Other patients or support groups | 15(19.7) | 5(13.9) | 4(10.0) |
| Books | 9(11.8) | 2 (5.6) | 7(17.5) |
Total N = 43, race available only for survey 2 respondents.
The majority of respondents reported receiving health information from their doctors (89%) or their parents (60%). Web sites were listed as sources of health information by 45%, and only a minority reported receiving information from other sources.
Self-Care Beliefs and Preparations for HCT
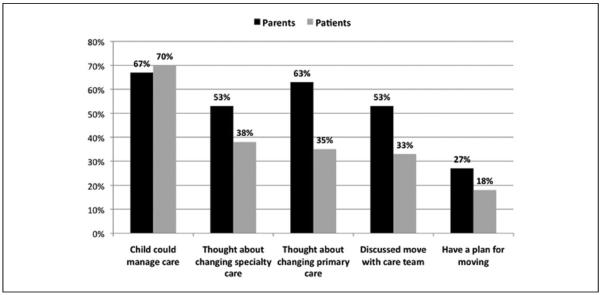
A majority of youth and parents reported that they thought they or their child could manage their health care on their own (70% and 67%, respectively; Figure 1). However, reported rates of actual HCT preparatory processes and planning were much lower. Among the total sample, proportionally fewer youth than parents had thought about changing their primary or specialty care from a pediatric to an adult care setting (respectively, 38% vs 53%, and 35% vs 63%), discussed HCT with their health care providers (33% vs 53%), or reported developing a plan for HCT (18% vs 27%).
Figure 1.
Parent and youth assessment of child self-care beliefs, health care transition readiness and preparation.
Sample is N = 79 patients and N = 52 parents for the first item (assessed in both surveys 1 and 2); sample N = 40 patients and N = 30 parents for the remaining items, assessed only in survey 2
Compared with those from the 3 specialty care clinics, participants from the adolescent medicine clinic were less likely to report having discussed HCT with a provider (12.5% vs 45.8%, odds ratio [OR] = 5.9, 95% confidence interval [CI] = 1.1, 31.9, P = .027). There were no differences between the 2 groups in believing they could manage their own care and reporting having a plan for HCT.
Transition Readiness Assessment
The total average TRAQ score for the patient sample was 3.6. Females had significantly higher scores than males (3.8 vs 3.3, P = .02) and TRAQ score was positively correlated with respondent age (r = 0.28, P = .013). There was no significant difference in mean TRAQ score by clinic; however, compared with the group of youth recruited from the other 3 specialty care clinics, participants from the adolescent medicine clinic had a higher average TRAQ score (4.0 vs 3.5, P = .005). Comparisons of individual item and total average TRAQ scores from youth and parents are shown in Table 2. The total average TRAQ score was higher among youth compared with parents (3.6 vs 3.2, P = .015), but this difference was not seen among the patient/parent dyad subgroup (n = 32; 3.3 vs 3.3, P = .5). Although the 2 groups did not differ in age, TRAQ scores among youth with an enrolled parent/guardian (n = 32 patients) were significantly lower than those of patients without an enrolled parent/guardian (n = 47 patients; 3.3 vs 3.8, P = .01). For both youth and parent groups, readiness levels for discrete skills assessed using the TRAQ varied, with higher scores evident on skills reflecting daily self-management tasks such as those pertaining to knowledge and behavior regarding medications, and to communication with providers during a visit (Table 2). Readiness levels for youth and parents diminish for skills pertaining to longer term disease management tasks such as arranging payment for care, understanding health insurance, ordering prescriptions, and procuring community services or accommodations.
Table 2.
Comparison of Youth and Parent Transition Readiness Assessment Questionnaire (TRAQ) Scores.
| All Respondents |
Parent/Youth Dyads |
|||
|---|---|---|---|---|
| Youth (n = 79) | Parents (n = 52) | Youth (n = 32) | Parents (n = 32) | |
| Total average TRAQ scorea | 3.6 | 3.2 | 3.3 | 3.3 |
| Child Report TRAQ items (Parent report items begin “Does your child …”) | ||||
| Do you answer questions that are asked by the doctor, nurse or clinic staff? | 4.9 | 4.6 | 4.8 | 4.8 |
| Do you ask questions of the doctor, nurse, or clinic staff (eg, What medications or treatments are best for you)? | 4.6 | 4.0** | 4.6 | 4.1* |
| Do you take your prescription medications correctly and on your own? | 4.3 | 4.2 | 4.0 | 4.2 |
| Do you fill out the medical history form, including a list of your allergies? | 4.2 | 3.6* | 4.0 | 3.8 |
| Do you know the side effects or bad reactions of each medication you take? | 4.1 | 3.8 | 3.5 | 4.0 |
| Do you help plan or prepare meals/food? | 4.0 | 3.8 | 3.9 | 4.0 |
| Do you keep a calendar or list of medical and other appointments? | 3.9 | 3.4 | 3.5 | 3.6 |
| Do you know what to do if you are having a bad reaction or side effect? | 3.8 | 4.3 | 3.5 | 4.3 |
| Do you fill a prescription if you need to? | 3.8 | 3.1* | 3.2 | 3.3 |
| Do you reorder medications before they run out? | 3.8 | 2 9*** | 3.5 | 3.1 |
| Do you arrange for your ride to medical appointments? | 3.8 | 2.9** | 3.6 | 3.1* |
| Do you call the doctor about unusual changes in your health (eg, allergic reactions)? | 3.8 | 2.9** | 3.4 | 3.1 |
| Do you apply for a job or work or vocational services? | 3.7 | 3.4 | 3.4 | 3.4 |
| Do you call the doctor's office to make an appointment? | 3.6 | 2.7** | 2.9 | 2.7 |
| Do you follow-up on any referral for tests or checkups or labs? | 3.6 | 2.5*** | 3.0 | 2.5* |
| Do you know what your health insurance covers? | 3.4 | 2.7** | 3.0 | 3.0 |
| Do you manage your money and budget household expenses (eg, use checking/debit card)? | 3.4 | 2.9 | 3.3 | 3.1 |
| Do you request the accommodations & support you need at school or work? | 3.3 | 3.7 | 3.0 | 3.9* |
| Do you pay or arrange payments for your medications? | 3.0 | 2.4* | 2.5 | 2.4 |
| Do you make a list of questions before the doctor's visit? | 2.6 | 3 | 2.5 | 3.1* |
| Do you get financial help with school or work? | 2.6 | 2.0 | 2.4 | 2.1 |
| Do you call on and use community support services (eg, after-school programs) and advocacy services (eg, legal services) when you need them? | 2.5 | 2.1 | 1.6 | 2.3 |
| Do you apply for health insurance if you lose your current coverage? | 2.3 | 1.7* | 2.0 | 1.8 |
Cronbach's α for the TRAQ in both parents and patients was high (parent .94, patient .90). Average TRAQ score (5 = always do this, 4 = have started doing this, 3 = learning to do this, 2 = don't know but want to learn, 1 = do not need to).
P < .05,
P < .01,
P < .001, using paired t test.
Among youth, a higher total average TRAQ score was associated with increased odds of believing that one is able to manage one's own care (OR = 3.2, 95% CI = 1.6–6.7). This relationship persisted in a multivariable logistic regression model adjusted for age and gender (adjusted odds ratio [AOR] = 4.0, 95% CI = 1.7–9.5). In this model, each 1 point increase in total average TRAQ score was associated with a 4-fold increase in the likelihood of believing one could manage one's own care. In the multivariable model, age and gender were not associated with belief in one's ability to manage one's own care. Among youth, total average TRAQ score was not associated with a report of having thought about, discussed or planned to change from a pediatric specialty to an adult health care setting. Older age was positively associated with discussing transition with the health care team (OR = 1.7, 95% CI = 1.2–2.4) and having a transition plan (OR = 1.5, 95% CI = 1.0–2.2). The small sample size for these items (drawn from survey 2 participants only) precludes analyses that control for patient age and gender.
Among parents, there was a positive association between higher total average TRAQ score and belief that one's child could manage his or her own care (adjusted for child age and gender; (AOR = 2.4, 95% CI = 1.03–5.6, P = .04). In the parent model, youth age and gender were not associated with parental report of their child's ability to manage their own care. Higher total average TRAQ score as reported by parents, and older age of child were both associated with parent report of discussing transition with the health care team, but not with parent report of having a HCT plan.
Discussion
Youth receiving care in pediatric specialty or adolescent-focused settings and their parents reported moderate readiness to transition to adult care using a skill-based readiness assessment measure. HCT readiness skills were associated with the belief in the ability of youth to manage their own care. However, high confidence in self-care espoused by youth and parents was belied by low reported readiness to manage many of the discrete tasks necessary for autonomous care, and by exceedingly low levels of preparation and planning for transition. This disconnect between self-care beliefs, transition readiness skills, and preparation and planning is consistent with national surveys of parents/guardians of children with special health care needs in which approximately 50% of respondents report having discussed HCT with their adolescent's physician14,15 despite only 30% reporting having a plan for addressing transition needs.10 Similarly, in the national Survey of Adult Transition and Health, only 24% of respondents aged 19 to 23 years reported receiving core transition counseling services.6
Although there is a paucity of evidence linking HCT preparation strategies with improved outcomes after transfer of care,16 consensus guidelines have outlined expectations for HCT preparation that could be incorporated into clinical practice, including regular assessment of HCT readiness.5 In our study, we used the TRAQ to measure HCT readiness skills.13 Similar to the initial TRAQ validation study, older youth and females had higher TRAQ scores, likely due to increased developmental maturity in these youth. Adjusting for these factors, high TRAQ scores were strongly associated with high beliefs in self-care abilities among youth. This supports a link between self-care beliefs and transition skills and further validates the TRAQ as a measure for assessing HCT readiness. Longitudinal studies are needed to determine whether efforts to strengthen transition readiness skills improve HCT-related outcomes, particularly for youth with chronic disease. Future research is also needed to ascertain correspondence between HCT readiness beliefs and reports about skills and objective readiness measures such as consistency and timeliness of prescription refills and adherence to appointments and self-care regimens.
Prior work has found that parents may report higher levels of transition preparation and planning than adolescents.11 We found that youth ratings of HCT readiness skills were higher than those of parents for the total sample; but, readiness assessments did not differ between groups where patients and parents were both enrolled. Results suggest that general surveys of parents may lead to underestimation of patient HCT readiness, while surveys of patients may overestimate readiness. Interestingly, greater percentages of parents than youth reported having thought about and discussed HCT with clinicians, suggesting that HCT efforts in clinics may be effectively targeting parents but may be missing youth. Although further research with a larger number of youth-parental dyads is needed, concrete preparatory activities for both patients and parents/caregivers are needed as are education and HCT planning efforts aimed at adolescents and efforts to foster parent/patient communication.17
Failure of HCT preparatory and planning processes can result in situations where youth are precipitously discharged out of pediatric care without the skills and knowledge needed to succeed in an adult-oriented system.8 Viewed in light of low levels of self-management skill pertaining to organizing/obtaining insurance, payment and community services reported by respondents, the need for improved HCT preparation is clear. An important component of HCT planning is dissemination of health-related information to transitioning youth. In our survey, the vast majority of youth reported receiving health information from their doctors or parents, emphasizing the need for HCT programs to incorporate counseling through health care providers and families as a primary mechanism for disseminating information and skills. A substantial percentage of youth also reported accessing the Internet for health information. Using Web-based platforms for HCT information, planning, and skill development may be a potential mechanism for improving transition care programs.18
Our study has several limitations. This was a single center study with a small sample, particularly for youth-parent dyads. Youth from the diabetes, cystic fibrosis, and myelodysplasia populations typify youth requiring structured HCT services19–22; however, as a cross-sectional convenience sample that opted in to the study, they may disproportionately reflect youth who are active in their care and disease management. Given the small sample size for each particular medical condition in our sample, we did not examine the relationship between self-care beliefs, transition readiness, and markers of disease-specific severity or outcomes. Finally, our data are based on self-report, and transition readiness could not be validated by external measures of health behavior.
In summary, the strong observed association between HCT readiness skills and self-care beliefs was inconsistent with the low report of HCT preparation activities in the care settings of our sample. Belief in self-care abilities may be inflated relative to actual transition preparation and skills. Targeted planning efforts to effectively support health care transition, particularly focusing on preparation for transfer of care, are needed.
Acknowledgments
Funding The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by research grants to Dr Weitzman from the Boston Children's Hospital Program for Patient Safety and Quality, award 220376 from the Center for Integration of Medicine and Innovative Technology, award 8UL1TR000170-05 and collaboration award No. 027343.386541.05230 from the Harvard Catalyst. Dr Sawicki is also supported by a grant from the National Heart, Lung, and Blood Institute (1K23HL105541-01A1).
Footnotes
Portions of these data were presented in a poster presentation at the Pediatric Academic Societies Annual Meeting in May 2012.
Declaration of Conflicting Interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Perrin JM, Bloom SR, Gortmaker SL. The increase of childhood chronic conditions in the United States. JAMA. 2007;297:2755–2759. doi: 10.1001/jama.297.24.2755. [DOI] [PubMed] [Google Scholar]
- 2.Rosen DS, Blum RW, Britto M, Sawyer SM, Siegel DM. Transition to adult health care for adolescents and young adults with chronic conditions: position paper of the Society for Adolescent Medicine. J Adolesc Health. 2003;33:309–311. doi: 10.1016/s1054-139x(03)00208-8. [DOI] [PubMed] [Google Scholar]
- 3.American Academy of Pediatrics; American Academy of Family Physicians. American College of Physicians–American Society of Internal Medicine A consensus statement on health care transitions for young adults with special health care needs. Pediatrics. 2002;110(6 pt 2):1304–1306. [PubMed] [Google Scholar]
- 4.Blum RW. Transition to adult health care: setting the stage. J Adolesc Health. 1995;17:3–5. doi: 10.1016/1054-139X(95)00073-2. [DOI] [PubMed] [Google Scholar]
- 5.Cooley WC, Sagerman PJ. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011;128:182–200. doi: 10.1542/peds.2011-0969. [DOI] [PubMed] [Google Scholar]
- 6.Sawicki GS, Whitworth R, Gunn L, Butterfield R, Lukens-Bull K, Wood D. Receipt of health care transition counseling in the National Survey of Adult Transition and Health. Pediatrics. 2011;128:e521–e529. doi: 10.1542/peds.2010-3017. [DOI] [PubMed] [Google Scholar]
- 7.McManus MA, Pollack LR, Cooley WC, et al. Current status of transition preparation among youth with special needs in the United States. Pediatrics. 2013;131:1090–1097. doi: 10.1542/peds.2012-3050. [DOI] [PubMed] [Google Scholar]
- 8.Reiss J, Gibson R. Health care transition: destinations unknown. Pediatrics. 2002;110(6 pt 2):1307–1314. [PubMed] [Google Scholar]
- 9.Reiss JG, Gibson RW, Walker LR. Health care transition: youth, family, and provider perspectives. Pediatrics. 2005;115:112–120. doi: 10.1542/peds.2004-1321. [DOI] [PubMed] [Google Scholar]
- 10.Scal P, Ireland M. Addressing transition to adult health care for adolescents with special health care needs. Pediatrics. 2005;115:1607–1612. doi: 10.1542/peds.2004-0458. [DOI] [PubMed] [Google Scholar]
- 11.Knapp C, Huang IC, Hinojosa M, Baker K, Sloyer P. Assessing the congruence of transition preparedness as reported by parents and their adolescents with special health care needs. Matern Child Health J. 2013;17:352–358. doi: 10.1007/s10995-012-0980-4. [DOI] [PubMed] [Google Scholar]
- 12.van Staa A, van der Stege HA, Jedeloo S, Moll HA, Hilberink SR. Readiness to transfer to adult care of adolescents with chronic conditions: exploration of associated factors. J Adolesc Health. 2011;48:295–302. doi: 10.1016/j.jadohealth.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 13.Sawicki GS, Lukens-Bull K, Yin X, et al. Measuring the transition readiness of youth with special health-care needs: validation of the TRAQ—Transition Readiness Assessment Questionnaire. J Pediatr Psychol. 2011;36:160–171. doi: 10.1093/jpepsy/jsp128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lotstein DS, Inkelas M, Hays RD, Halfon N, Brook R. Access to care for youth with special health care needs in the transition to adulthood. J Adolesc Health. 2008;43:23–29. doi: 10.1016/j.jadohealth.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 15.Lotstein DS, McPherson M, Strickland B, Newacheck PW. Transition planning for youth with special health care needs: results from the National Survey of Children with Special Health Care Needs. Pediatrics. 2005;115:1562–1568. doi: 10.1542/peds.2004-1262. [DOI] [PubMed] [Google Scholar]
- 16.Bloom SR, Kuhlthau K, Van Cleave J, Knapp AA, Newacheck P, Perrin JM. Health care transition for youth with special health care needs. J Adolesc Health. 2012;51:213–219. doi: 10.1016/j.jadohealth.2012.01.007. [DOI] [PubMed] [Google Scholar]
- 17.Lemly DC, Weitzman ER, O'Hare K. Advancing health care transitions in the medical home: tools for providers, families and adolescents with special health care needs. Curr Opin Pediatr. 2013;25:439–446. doi: 10.1097/MOP.0b013e3283623d2f. [DOI] [PubMed] [Google Scholar]
- 18.Weitzman ER, Kaci L, Quinn M, Mandl KD. Helping high-risk youth move through high-risk periods: personally controlled health records for improving social and health care transitions. J Diabetes Sci Technol. 2011;5:47–54. doi: 10.1177/193229681100500107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Woodward JF, Swigonski NL, Ciccarelli MR. Assessing the health, functional characteristics, and health needs of youth attending a noncategorical transition support program. J Adolesc Health. 2012;51:272–278. doi: 10.1016/j.jadohealth.2011.12.016. [DOI] [PubMed] [Google Scholar]
- 20.Tuchman LK, Schwartz LA, Sawicki GS, Britto MT. Cystic fibrosis and transition to adult medical care. Pediatrics. 2010;125:566–573. doi: 10.1542/peds.2009-2791. [DOI] [PubMed] [Google Scholar]
- 21.Garvey KC, Wolpert HA, Rhodes ET, et al. Health care transition in patients with type 1 diabetes: young adult experiences and relationship to glycemic control. Diabetes Care. 2012;35:1716–1722. doi: 10.2337/dc11-2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.de Beaufort C, Jarosz-Chobot P, Frank M, de Bart J, Deja G. Transition from pediatric to adult diabetes care: smooth or slippery? Pediatr Diabetes. 2010;11:24–27. doi: 10.1111/j.1399-5448.2009.00524.x. [DOI] [PubMed] [Google Scholar]