Abstract
There is increasing clinical and molecular evidence for the role of hormones and specifically estrogen and its receptor in schizophrenia. A selective estrogen receptor modulator, raloxifene, stimulates estrogen-like activity in brain and can improve cognition in older adults. The present study tested the extent to which adjunctive raloxifene treatment improved cognition and reduced symptoms in young to middle-age men and women with schizophrenia. Ninety-eight patients with a diagnosis of schizophrenia or schizoaffective disorder were recruited into a dual-site, thirteen-week, randomized, double-blind, placebo-controlled, crossover trial of adjunctive raloxifene treatment in addition to their usual antipsychotic medications. Symptom severity and cognition in the domains of working memory, attention/processing speed, language and verbal memory were assessed at baseline, 6 and 13 weeks. Analyses of the initial 6-week phase of the study using a parallel groups design (with 39 patients receiving placebo and 40 receiving raloxifene) revealed that participants receiving adjunctive raloxifene treatment showed significant improvement relative to placebo in memory and attention/processing speed. There was no reduction in symptom severity with treatment compared with placebo. There were significant carryover effects, suggesting some cognitive benefits are sustained even after raloxifene withdrawal. Analysis of the 13-week crossover data revealed significant improvement with raloxifene only in attention/processing speed. This is the first study to show that daily, oral adjunctive raloxifene treatment at 120 mg per day has beneficial effects on attention/processing speed and memory for both men and women with schizophrenia. Thus, raloxifene may be useful as an adjunctive treatment for cognitive deficits associated with schizophrenia.
Introduction
For the majority of those diagnosed with the illness, schizophrenia is considered to be a debilitating mental disorder that often responds inadequately to existing antipsychotic medications.1 One of the characteristics of schizophrenia that is least responsive to pharmacological treatment is cognitive impairment in the domains of memory and attention,2 which are known to limit the vocational prospects and quality of life for people with schizophrenia.3 Despite decades of research into the cognitive deficits of schizophrenia, there are no satisfactory pharmacological agents capable of restoring cognitive function. Thus, there is a great motivation to develop adjunctive agents or additional therapies that can address this unmet clinical need.4 Given that abnormalities of prefrontal cortex and hippocampal function contribute to the cognitive deficits in schizophrenia, agents capable of restoring dysfunctional neuronal processes in these regions may be used to develop novel treatments for cognitive impairment associated with schizophrenia. Sex hormones are known to have beneficial effects in both cortex and hippocampus.
Sex hormones may influence the course of schizophrenia, as the onset of schizophrenia typically occurs in late adolescence.5 We have shown that the adolescent sex hormones can change social interactions, sensory motor gating and hippocampal neurogenesis in nonhuman primates.6, 7, 8 Furthermore, the age of onset, course of the illness, clinical presentation and response to treatment in people with schizophrenia is different in women compared with men.9, 10, 11, 12 Women have a greater likelihood of developing first-episode psychosis or a symptom exacerbation when estrogen levels are low, such as during an estrogen trough in the menstrual cycle, post partum and around menopause.9, 13, 14, 15 Conversely, schizophrenia symptoms can remit during pregnancy when estrogen and progesterone levels are high.16 These observations have led to the hypothesis that estrogen may have a protective role against schizophrenia. In males, testosterone is converted to estrogen in the brain. A previous study found that testosterone was significantly lower in men with schizophrenia than in healthy males and that lower testosterone levels correlated with more severe negative symptoms.17 We found that low normal testosterone levels in men with schizophrenia were related to poor cognitive performance and altered cortical neural activity.18, 19 Thus, both estrogen and testosterone may modulate aspects of schizophrenia in both men and women.
There is a substantial body of scientific literature supporting the beneficial effects of estrogen in the brain that includes preservation of memory and attention.20 In animal studies, restoration or augmentation of endogenous estrogen promotes neuronal growth, stimulates neuronal plasticity, increases synaptic spine density and neurogenesis and improves neuroprotection against excitotoxicity in cerebral cortex and hippocampus.21, 22, 23 We and others have shown that estrogen receptors are localized to both pyramidal and non-pyramidal neurons in the human prefrontal cortex and hippocampus24, 25 and we have identified many different splice variants of the estrogen receptor alpha, which potentially adds considerable diversity to how the human brain may respond to circulating estrogen.26 Importantly, the estrogen receptor is altered in the brains of people with schizophrenia, involving both lower mRNA levels and/or failure to express the fully functional wild-type form of the estrogen receptor.26, 27 Our molecular discoveries support and extend the estrogen hypothesis by showing that the blunted ability of the brain to respond to circulating estrogen may contribute to the pathophysiology of schizophrenia in both men and women. These molecular changes in the estrogen receptor suggest that the brain response to sex hormones in men and women with schizophrenia may be inadequate, a proposal that has been indirectly supported by our in vitro cell culture experiments.27, 28 Our molecular findings coupled with the clinical observations noted above suggest that cognitive function in men and women with schizophrenia may benefit from stimulation of the estrogen signaling pathway in the brain. However, reversal of aging-related memory deficits via estrogen replacement strategies in healthy older females has yielded mixed results.29
The influence of adjuvant estrogen on cognition in people with schizophrenia is generally under explored. One small, preliminary study reported significant improvements in verbal memory with estrogen replacement in postmenopausal women with schizophrenia,30 whereas more recent studies with larger samples demonstrated mixed results of hormone therapy on cognition in premenopausal women with schizophrenia.31, 32 Although studies of the effects of estrogen on cognition in schizophrenia are limited, several studies of estrogen therapy in schizophrenia have demonstrated significant symptom reduction in women with schizophrenia and proof of principle studies suggest that addition of estradiol may also be effective at accelerating symptom reduction in men with schizophrenia.31, 33, 34, 35, 36 These studies are encouraging regarding the potential value of estrogen as an adjunctive treatment for both men and women with schizophrenia. However, estrogen can carry some risks37 and there may be undesirable adverse events of long-term adjuvant estrogen in men. Thus, other treatments targeting the estrogen receptor that can specifically stimulate estrogen action in brain cells and be relatively free of adverse events in both men and women with schizophrenia are needed. One such agent is the selective estrogen receptor modulator raloxifene, which was shown to act as an estrogen receptor agonist in the brain (and bone) and antagonist in other tissues.38
Raloxifene, a second-generation selective estrogen receptor modulator, is approved for use in the treatment of osteoporosis in postmenopausal women and for breast cancer in women and can have beneficial effects on brain function including increased cortical plasticity.39, 40 Studies have reported that raloxifene at a daily dose of 120 mg preserved neural activity during a memory challenge in healthy aging men41 and preserved cognition in postmenopausal women.42 Recent clinical trials and case reports have shown that adjunctive raloxifene at 60 or 120 mg is beneficial for the treatment of positive, negative and general psychopathology symptoms in postmenopausal women with schizophrenia.43, 44, 45 One recent study also suggests that adjunctive raloxifene administration at 60 mg per day improved memory and verbal fluency in a small cohort of postmenopausal women with schizophrenia.46 However, to date, no clinical trials of raloxifene have been reported in young adult to middle-age men and women with schizophrenia. On the basis of our own findings that the action of estrogen receptors in brain may be blunted in males and females with schizophrenia and the previous studies showing beneficial effects of adjunctive raloxifene treatment on cognition in older men and women, we predicted that adjunctive raloxifene treatment at a daily dosage of 120 mg would improve cognitive deficits, particularly in the domain of verbal memory, and reduce symptoms in both men and women with schizophrenia.
Materials and Methods
Participants
People with schizophrenia
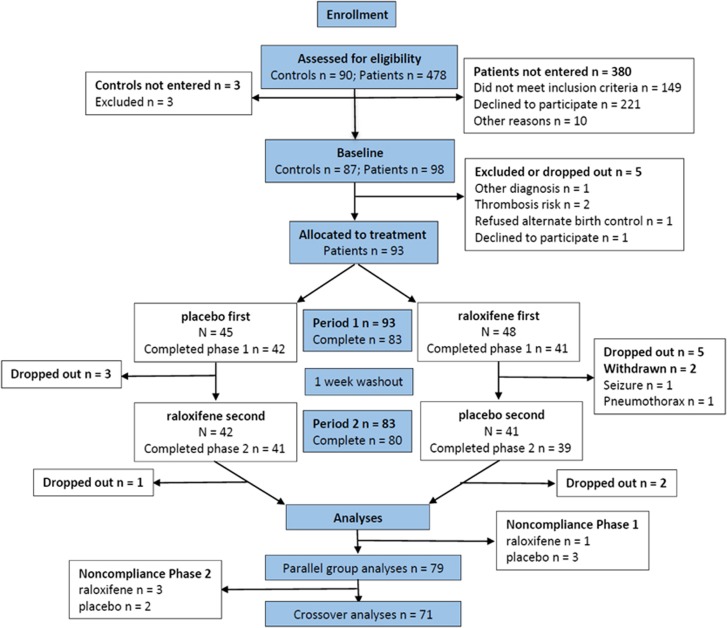
From the 478 potential patients across Australia (either responding to a national television program on schizophrenia research or recruited from local clinics) who were screened for participation in this study, 149 were excluded, 221 declined and 10 were lost to follow-up after completing the telephone screen, leaving a total of 98 patients with schizophrenia or schizoaffective disorder being recruited into two sites: either Neuroscience Research Australia, Randwick, New South Wales, Australia (27 females and 49 males) or the Northern Adelaide Local Health Network Mental Health Service, Adelaide, South Australia, Australia (11 females and 11 males). All participants were between 18 and 51 years of age and had been receiving antipsychotics for at least 1 year before entering the study (see Supplementary Table 1 for the frequency of people receiving each antipsychotic medication at entry into the trial and the parallel group analysis). A diagnosis of schizophrenia or schizoaffective disorder was determined using the Structured Clinical Interview for Diagnostic and Statistical Manual IV-TR Axis I Disorders47 by a clinician trained in administration of the SCID which was confirmed independently by another clinician. Patients with a concurrent Axis I psychiatric diagnosis, a history of substance abuse or dependence (within the past 5 years), head injuries with loss of consciousness, seizures, central nervous system infection, untreated diabetes or hypertension, mental retardation or contraindications to the administration of raloxifene were excluded. Women were excluded if they were currently pregnant or were receiving hormone therapy and refused alternate forms of birth control. See Figure 1 for the CONSORT diagram.
Figure 1.
CONSORT flow diagram.
Healthy comparison group
A group of healthy adults were also recruited for a one-time assessment to provide a baseline comparison group. Exclusion criteria consisted of a personal history of or a first-degree relative with a DSM-IV Axis I psychiatric diagnosis, history of substance abuse or dependence (within the past 5 years), head injuries with loss of consciousness, seizures, central nervous system infection, untreated diabetes or hypertension or mental retardation. Eighty-seven healthy adults (41 females and 46 males) between 20 and 50 years of age met criteria for entry into the comparison group. Nineteen of the total healthy controls were recruited from Adelaide and 68 were recruited from the Sydney area.
All participants provided informed written consent before entering the study, which was conducted under protocols approved by the University of New South Wales (07/121 and 09/187), South Eastern Sydney and Illawarra Area Health Service (07-259) Human Research Ethics Committees and the Queen Elizabeth Hospital Ethics and Human Research Committee, Adelaide (2010188). The trial was registered with the Australian and New Zealand Clinical Trials Registry, registration number: ACTRN12608000461392, with the primary and secondary outcomes of cognitive (immediate and delayed story recall, working memory and verbal fluency) and symptoms measures (positive and negative symptoms), respectively.
Trial design
A 13-week, randomized, double-blind, crossover, placebo-controlled trial was conducted in which patients alternated between receiving adjunctive 120 mg per day of encapsulated raloxifene HCl orally and a placebo (encapsulated lactose) in addition to their currently prescribed antipsychotic medication. Encapsulation of raloxifene and placebo in addition to all quality assessment/control testing (including cleaning validation and International Conference on Harmonization stability trials) of the compound over the duration of the study was performed by IDT Australia, Victoria, Australia. Following the first 6-week period of the trial, all patients entered a 1-week ‘washout' (raloxifene half-life =27.7 h).48 After the washout, all patients then entered the second 6-week period of the trial consisting of the alternate treatment (raloxifene or placebo). Assessments were made at baseline and at the end of weeks 6 and 13 by a psychologist or psychometrician trained in administration and scoring. Patients were monitored throughout the trial for the occurrence of adverse events. All participants and study personnel were blind to the adjunctive treatment status. The Prince of Wales Hospital Pharmacy Clinical Trials Unit used a computer generated randomization schedule to assign patients to the raloxifene-placebo or placebo-raloxifene treatment order conditions.
Treatment compliance and adverse events
At completion of the first and second period of the study, participants returned any remaining pills. Compliance was assessed based on the percentage of tablets returned. All patients with treatment compliance below 80% (total n=9, period 1: 3 placebo, 1 raloxifene; period 2: 3 placebo, 2 raloxifene) were excluded from the analyses (see Figure 1). All adverse events were recorded during the 13 weeks of the trial.
Assessments
Cognitive assessments
At baseline only, all participants were administered a four subtest version of the Wechsler Adult Intelligence Scale-Third Edition (WAIS-III)49 (consisting of Arithmetic, Similarities, Picture Completion and Digit Symbol subtests) as an estimate of current IQ, and the Wechsler Test of Adult Reading (WTAR)50 as an estimate of premorbid intelligence. Additional cognitive assessments were performed at baseline and at the end of 6 and 13 weeks of treatment for all patients. Working memory, verbal fluency, attention/perceptual-motor processing speed and verbal memory were assessed using the WAIS-III Letter-Number Sequencing (LNS), the Controlled Oral Word Association Test (COWAT) letter fluency,51 Form A of the Trail Making Test (TMT-A)52 and Logical Memory I and II (LMI and LMII) of the Wechsler Memory Scale Revised,53 respectively. Identical versions of LNS and TMT-A and alternate versions of the COWAT letter fluency and LMI and II were administered at each assessment. TMT-A was incorporated into the battery after initiation of the trial, which resulted in a lower total number of patients completing this measure.
Symptom, emotional and functional assessments
Symptom severity was assessed in patients at baseline and after 6 and 13 weeks of treatment using the Positive and Negative Syndrome Scale (PANSS).54 Inter-rater reliability for the PANSS scoring was high with an average intraclass correlation coefficient of 0.90. Negative emotional states, daily function and quality of life were assessed with the 21-item version of the Depression Anxiety and Stress Scale (DASS),55 the Short Form 36 Version 2 Health Survey questionnaire (SF-36v2)56 and the Schizophrenia Quality of Life Scale (SQLS),57 respectively.
Whole-blood assays
Fasting peripheral blood was taken between 0900 and 1100 hours to control for alterations in hormone levels due to circadian variations. Immediately following collection, clotted and heparinized blood was delivered on ice to the pathology service at each site. A hormone panel (consisting of follicle-stimulating hormone and luteinizing hormone) and a coagulation panel, consisting of a prothrombin time test, international normalized ratio and the antithrombin III deficiency test, were assayed at baseline in patients and controls and after 6 and 13 weeks of treatment in patients. Blood measures were reviewed by two to three medical doctors for changes in values that were outside the clinically normal range.
Statistical analyses
Data analysis was performed using IBM SPSS 22 for Windows. Baseline demographics were compared between treatment order conditions in patients using t-tests, Wilcoxon rank-sum tests or χ2-tests as appropriate. Where possible, age- and sex-scaled scores were used for the cognitive tests and all cognitive test scores were standardized into z-scores relative to healthy participant means and s.d.
Period effects, defined as a change affecting an entire cohort that is related to a particular period of time (that is, first 6 weeks or second 6 weeks), were assessed using paired t-tests comparing period 1 with period 2 difference scores (week 6 minus baseline versus week 13 minus week 6 for each outcome variable) collapsing across treatment conditions. Potential carryover effects, defined as an effect that is retained or persists from one treatment condition to the other, were determined for each outcome measure using independent t-tests comparing the raloxifene/placebo group to the placebo/raloxifene group on the sum of their period 1 and period 2 difference scores.58
Owing to the evidence of carryover and period effects in our preliminary analyses (see Results), we initially analyzed for primary treatment outcomes using a parallel groups design from baseline to the end of week 6 and then secondarily analyzed using the full crossover design. To assess the treatment effects on cognition in the first 6-week phase only, a mixed multivariate analysis of variance (MANOVA, with LNS, LMI, LMII, and COWAT as dependent variables) were performed with time (baseline and after week 6) as the within-subject factor and treatment condition (raloxifene versus placebo) as the between-subjects factor. As TMT-A was not available in the entire sample, the analysis of treatment effects on TMT-A was performed separately using a mixed ANOVA with TMT-A as the dependent variable. Symptom severity, emotional and functional measures were each separately analyzed for treatment effects using a series of mixed (M)ANOVAs (a mixed MANOVA for PANSS positive, negative and general; a mixed MANOVA for DASS depression, anxiety and stress; a mixed ANOVA for SF-36v2 total and a mixed ANOVA for SQLS total). Post hoc Fisher least significant difference pairwise comparisons were used to identify specific significant effects after obtaining significant overall (M)ANOVA results and correction for multiple comparisons were performed on the cognitive and symptom pairwise comparisons separately using the Holm–Bonferroni method to control the familywise error rate. Effect size calculations were measured as Cohen's d. Given that sex differences in raloxifene treatment was not the main question we set out to address and our study was not designed to assess sex related differences in raloxifene treatment, we did not use sex as a grouping factor in the main analyses; however, we did perform supplementary analyses using sex as a grouping factor in the parallel group design.
To assess the overall crossover design results, difference scores were calculated for each outcome measure for each phase (period 1: week 6 score minus baseline score, period 2: week 13 score minus week 6 score). These difference scores were combined for the raloxifene and placebo conditions, regardless of the period. Treatment effects on cognition were analyzed using a repeated measures MANOVA (with LNS, LMI, LMII and COWAT as dependent variables) and a repeated measures ANOVA (with TMT-A as a dependent variable) with treatment condition (raloxifene versus placebo) as the within-subjects measure. Treatment effects for symptom, emotional and functional measures were analyzed using separate repeated measures MANOVAs (for PANSS and DASS) and repeated measures ANOVAs (for SF36-v2 and SQLS) with treatment condition (raloxifene versus placebo) as the within-subjects factor.
Defining responders
Responder analysis for the cognitive measures from baseline to 6 weeks was performed using the Jacobson–Truax Method of defining clinically reliable change with cutoff formula c.59 Reliable change index measures used healthy control test–retest reliability values from the WAIS-III and WMS-III technical manuals (for LMI, LMII and LNS)49, 53 and from Williams et al.60 (for COWAT and TMT-A). Any patient who met the criteria of the Jacobson–Truax method, which includes a significant change from baseline and meeting or exceeding a calculated threshold, on any of the five cognitive outcome measures was considered a ‘cognitive responder'. For symptom measures, response to treatment was defined as a 20% improvement on any symptom measure score as suggested by Kane et al.61 Patients were grouped into two categories, the ‘symptom responders' with ≥20% symptom severity reduction and ‘symptom non-responders' who showed <20% symptom severity reduction. χ2-tests were run to determine whether the number of patients showing improvements was significantly different in either treatment condition and Number Needed to Treat calculations were used to determine the effectiveness of the intervention.
Results
Demographics and baseline scores
Demographics and baseline scores for the treatment groups based on assignment order (that is, raloxifene-placebo versus placebo-raloxifene) are shown in Table 1. The treatment assignment order groups differed significantly at baseline on age of disease onset and TMT-A scores. However, these differences were relatively small, that is, less than 3 years of age and less than 20% difference in performance, respectively. There were no other significant differences between assignment order groups. Thus, no significant difference between the treatment order groups in relation to PANSS-positive and -negative symptom severity scores and other variables suggests that our study was consistent with the recommendations provided in relation to controlling for potential concurrent changes in symptoms and cognition.62 See Supplementary Table 2 for the means and s.d. in relation to the demographic and cognitive variables in the healthy participant group.
Table 1. Baseline demographics cognitive, symptom and daily function measures for parallel groups analysis.
| Characteristics | N | Placebo first | N | Raloxifene first | P-value |
|---|---|---|---|---|---|
| Age | 39 | 34.0 (8.4) | 40 | 37.4 (7.3) | 0.06 |
| Education | 39 | 12.3 (2.2) | 40 | 12.9 (2.8) | 0.45 |
| Age of disease onset | 39 | 22.1 (6.3) | 40 | 24.1 (4.8) | 0.02 |
| Illness duration | 39 | 12.2 (7.2) | 40 | 13.4 (7.5) | 0.51 |
| Sex (number) | 39 | 40 | χ2=0.19 | ||
| Male | 27 | 22 | |||
| Female | 12 | 18 | |||
| Race (number) | 39 | 40 | χ2=0.36 | ||
| Caucasian | 33 | 35 | |||
| Asian | 3 | 1 | |||
| Caucasian/Asian | 3 | 2 | |||
| Other | 0 | 2 | |||
| CPZ equivalents | 39 | 530.4 (395.7) | 40 | 529.0 (501.8) | 0.98 |
| Premorbid and current IQ | |||||
| WAIS-III | 39 | 90.8 (12.1) | 40 | 91.7 (14.5) | 0.78 |
| WTAR | 39 | 102.4 (8.8) | 40 | 102.7 (8.9) | 0.91 |
| Cognitive tests | |||||
| WAIS-III-LNS | 39 | 7.8 (2.9) | 40 | 8.4 (2.7) | 0.40 |
| WMSR-LMI | 39 | 7.8 (3.6) | 40 | 7.2 (3.2) | 0.44 |
| WMSR-LMII | 39 | 6.1 (3.3) | 40 | 5.9 (3.0) | 0.76 |
| TMT-A | 28 | 35.3 (9.3) | 29 | 41.8 (11.4) | 0.02 |
| COWAT | 39 | 38.2 (10.6) | 40 | 36.0 (11.2) | 0.38 |
| Symptom and daily function | |||||
| PANSS | |||||
| Positive | 39 | 14.9 (4.3) | 40 | 15.1 (5.3) | 0.92 |
| Negative | 39 | 14.6 (7.0) | 40 | 14.7 (5.7) | 0.61 |
| General | 39 | 30.5 (8.1) | 40 | 31.7 (9.7) | 0.76 |
| Total | 39 | 60.0 (16.8) | 40 | 61.4 (17.5) | 0.72 |
| DASS | |||||
| Depression | 39 | 11.6 (10.2) | 40 | 12.2 (8.7) | 0.56 |
| Anxiety | 39 | 10.7 (8.4) | 40 | 9.2 (7.1) | 0.49 |
| Stress | 39 | 14.7 (9.8) | 40 | 13.6 (8.0) | 0.61 |
| SF-36v2 total | 38 | 115.2 (16.5) | 39 | 115.2 (19.5) | 1.00 |
| SQLS total | 37 | 45.1 (16.7) | 39 | 47.6 (16.8) | 0.52 |
Abbreviations: COWAT, Controlled Oral Word Association Test; CPZ, chlorpromazine; DASS, Depression Anxiety and Stress Scale; IQ, intelligence quotient; LNS, letter number sequencing; PANSS, positive and negative syndrome scale; SF-36v2, Short Form 36 Version 2 Health Survey Questionnaire; SQLS, Schizophrenia Quality of Life Scale; TMT-A, trail making test A; WAIS-III, Wechsler Adult Intelligence Scale 3rd Edition; WMSR-LMI, Wechsler Memory Scale Revised Logical Memory I; WMSR- LMII, Wechsler Memory Scale Revised Logical Memory II, WTAR, Wechsler Test of Adult Reading.
Unless otherwise specified, values refer to means and s.d. in parentheses.
General outcomes of blood analyses, compliance and adverse events
Blood analyses revealed statistically significant main effects of treatment, but no clinically relevant differences on the hormone and coagulation panel measures between the raloxifene- and placebo-treated groups (see Supplementary Table 3). Total compliance for period 1 of the trial was 95.2% (n=79) and 88.8% (n=71) for period 2. There were no significant differences between the frequencies of adverse events occurring at greater than or equal to 3% in patients during raloxifene versus placebo treatment phases (see Table 2). Throughout the course of the study, there were no serious adverse events or suspected unexpected serious adverse reactions that were attributed to the study medication. There were two serious adverse events (a pneumothorax and a seizure) that occurred during administration of raloxifene, which resulted in discontinuation from the study for each participant; however, in each case, the primary care treatment team determined that these serious adverse events were unlikely to have resulted from the administration of raloxifene.
Table 2. Adverse events during the 13-week raloxifene/placebo trial.
| Event |
Placebo (n=90) |
Raloxifene (n=89) |
Fisher's exact P-value | ||
|---|---|---|---|---|---|
| Number | Percentage | Number | Percentage | ||
| Symptom typea | |||||
| Gastrointestinal disorders | 8 | 9 | 17 | 19 | 0.06 |
| Abdominal pain NOS | 2 | 2 | 4 | 4 | |
| Constipation | 3 | 3 | 4 | 4 | |
| Dyspepsia | 0 | 0 | 3 | 3 | |
| Nausea | 3 | 3 | 6 | 7 | |
| General disorders | 4 | 4 | 3 | 3 | 1.00 |
| Feeling abnormal | 4 | 4 | 3 | 3 | |
| Metabolism and nutrition disorders | 3 | 3 | 2 | 2 | 1.00 |
| Abnormal weight gain | 3 | 3 | 2 | 2 | |
| Musculoskeletal and connective tissue disorders | 4 | 4 | 5 | 6 | 0.75 |
| Cramps | 4 | 4 | 5 | 6 | |
| Nervous system disorders | 7 | 8 | 8 | 9 | 0.79 |
| Headaches | 3 | 3 | 3 | 3 | |
| Lethargy | 4 | 4 | 5 | 6 | |
| Psychiatric disorders | 20 | 22 | 24 | 27 | 0.49 |
| Depressed mood | 5 | 6 | 7 | 8 | |
| Sleep disturbance | 0 | 0 | 3 | 3 | |
| Panic attack | 2 | 2 | 3 | 3 | |
| Emotional distress | 1 | 1 | 3 | 3 | |
| Psychotic behavior exacerbation | 5 | 6 | 2 | 2 | |
| Paranoia exacerbation | 4 | 4 | 3 | 3 | |
| Hallucinations exacerbation | 3 | 3 | 3 | 3 | |
| Respiratory, thoracic and mediastinal disorders | 3 | 3 | 4 | 4 | 0.72 |
| Common cold | 3 | 3 | 4 | 4 | |
Symptoms occurring in ⩾3% of patients; patients can be accounted for more than once, as they may experience multiple symptoms.
Adverse events were analyzed for the full crossover trial. Occurrences of adverse events were coded into low-level terms and system organ class using the Medical Dictionary for Regulatory Activities (MedDRA). Fisher's exact tests were used to compare the frequency of a given adverse event and system organ class occurrences (⩾3%) between treatment conditions (raloxifene versus placebo) with period I and period II of the crossover trial combined. Blood measure variations over each period were simplified into two categories: ‘abnormal change' (a change deviating from the normal range) or ‘no abnormal change' (no change or changes within the normal range). Periods I and II were combined and the resulting frequencies were compared between raloxifene and placebo condition.
Three patients were withdrawn for acute adverse events that were later determined to be unrelated to treatment and seven individuals discontinued due to feelings of adverse symptomatic changes (four were in the raloxifene condition at the time of discontinuation). There was no significant difference in adverse events that occurred in ⩾3% patients between the raloxifene and placebo condition.
Period and carryover effects
There were significant period effects in the difference scores for the cognitive, symptom and functional measures (see Supplementary Table 4). Difference scores (improvement) in the second 6 weeks (period 2 of the trial were significantly less than during the first 6 weeks (period 1) for LMI, PANSS positive, general, and total, and SF36-v2 total scores. Assessment of the carryover effect amongst individual cognitive, symptom, emotional and functional measures showed significant carryover effects for LMI, LMII and TMT-A (see Supplementary Table 5 and Supplementary Figure 1).
Parallel groups design analysis of cognitive measures
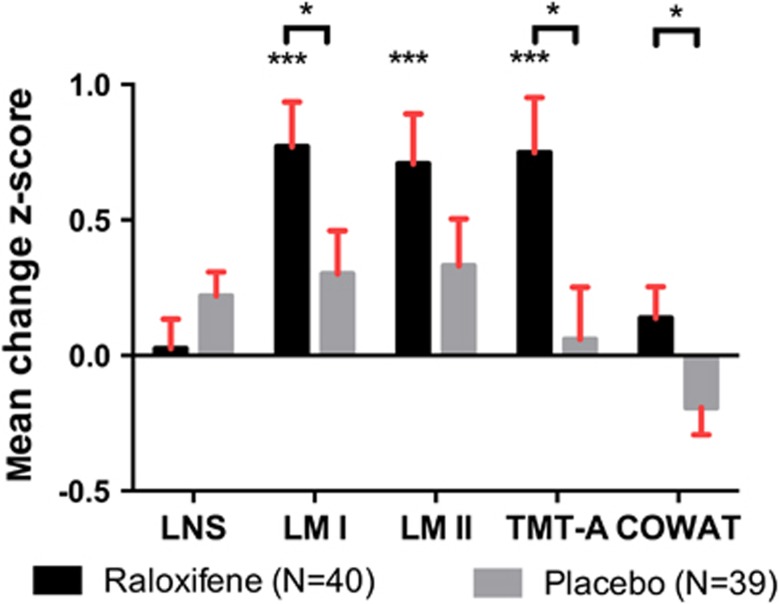
Given that the carryover effects reported above may interfere with attempts to detect treatment effects in the full crossover design analysis, we performed a separate analysis of the treatment outcomes at the end of the first 6-week period in 40 patients receiving raloxifene versus 39 patients receiving placebo using a parallel groups design to determine the effects of raloxifene without the potential confound of carryover or period effects. In this analysis, patients receiving raloxifene showed significant improvement on measures of cognition relative to the placebo group. Results of the mixed (M)ANOVAs for the cognitive test scores showed significant treatment condition by time interactions (combined cognitive tests treatment x time Wilks' Lambda=0.9, F(4,74)=2.7, P=0.04; TMT-A treatment x time Wilks' Lamda = 0.9, F(1,55)=6.0, P=0.02), see Table 3. Follow-up, protected post hoc least significant difference tests with Holm–Bonferroni corrections to control for familywise error rate in Table 3 show significant increases for raloxifene relative to placebo treatment in relation to LMI (P<0.001), LMII (P<0.001) and TMT-A (P<0.001), in which all survived correction for multiple comparisons. Medium to large effect sizes were obtained for raloxifene treatment relative to placebo, with effect sizes of 0.64 for LMI, 0.62 for LMII and 0.59 for TMT-A (see Table 3). Univariate results from the combined cognitive measures MANOVA indicated a significant interaction for the COWAT measure, where the raloxifene treated group improved and the placebo-treated group declined, but nonsignificantly from their own baselines. Changes across all cognitive measures are displayed for the first 6 weeks of the trial in Figure 2. See Supplementary Tables 6 and 7 for the results of our supplemental analyses of the effects of raloxifene on cognition that includes sex as a grouping factor and shows (in addition to confirming our main effects of raloxifene on memory and cognition) a significant interaction between sex and raloxifene treatment on verbal fluency in which females but not males show improvement in verbal fluency with raloxifene.
Table 3. Cognitive and symptom outcomes in parallel groups analyses.
|
Omnibus tests for measure x treatment x visit interaction |
(M)ANOVA results |
Placebo LSD comparisons |
Raloxifene LSD comparisons |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Measure | N | Test value | F-test | P-value | Mean difference (s.e.) | P-value | Cohen's d | Mean difference (s.e.) | P-value | Cohen's d |
| Cognitive outcomes | ||||||||||
| Cognitive tests: condition × time | 79 | W-L 0.9 | (4,74)=2.7 | 0.04 | ||||||
| WAIS-III-LNS | 79 | H-F 0.4 | (1,78)=1.9 | 0.17 | −0.2 (0.1) | 0.03 | 0.23 | −0.0 (0.1) | 0.80 | 0.03 |
| WMSR-LMI | 79 | H-F 2.2 | (1,78)=4.2 | 0.04 | −0.3 (0.2) | 0.07 | 0.26 | −0.8 (0.2) | <0.001a | 0.64 |
| WMSR-LMII | 79 | H-F 1.4 | (1,78)=2.2 | 0.14 | −0.3 (0.2) | 0.07 | 0.30 | −0.7 (0.2) | <0.001a | 0.62 |
| COWAT | 79 | H-F 1.1 | (1,78)=4.6 | 0.03 | 0.2 (0.1) | 0.08 | 0.21 | −0.1 (0.1) | 0.21 | 0.14 |
| TMT-A: condition × time | 57 | W-L 0.9 | (1,55)=6.0 | 0.02 | ||||||
| TMT-A | 0.1 (0.2) | 0.77 | 0.05 | 0.7 (0.2) | <0.001a | 0.59 | ||||
| Symptom outcomes | ||||||||||
| PANSS tests: condition × time | 79 | W-L 1.0 | (3,75)=0.7 | 0.54 | ||||||
| Positive | − | − | − | 1.2 (0.4) | <0.01 | 0.27 | 0.8 (0.4) | 0.05 | 0.16 | |
| Negative | − | − | − | −0.0 (0.6) | 0.96 | 0.00 | 0.9 (0.5) | 0.11 | 0.17 | |
| General | − | − | − | 1.8 (0.7) | 0.01 | 0.22 | 2.0 (0.7) | <0.01 | 0.23 | |
| DASS tests: condition × time | 78 | W-L 1.0 | (3,74)=1.1 | 0.35 | ||||||
| Depression | − | − | − | 1.1 (1.3) | 0.39 | 0.11 | 2.9 (1.3) | 0.03 | 0.34 | |
| Anxiety | − | − | − | 0.8 (1.1) | 0.47 | 0.11 | 1.3 (1.1) | 0.24 | 0.21 | |
| Stress | − | − | − | 2.2 (1.4) | 0.11 | 0.24 | 0.9 (1.4) | 0.52 | 0.11 | |
| SF-36v2 total: condition × time | 77 | W-L 1.0 | (1,75)=0.0 | 0.84 | −4.9 (2.1) | 0.02 | 0.27 | −4.3 (2.1) | 0.04 | 0.24 |
| SQLS total: condition × time | 75 | W-L 1.0 | (1,73)=0.1 | 0.81 | 4.3 (2.2) | 0.05 | 0.25 | 5.1 (2.1) | 0.02 | 0.31 |
Abbreviations: COWAT, Controlled Oral Word Association Test; DASS, depression anxiety and stress scale; H-F, Huynh-Feldt value; LSD, least significant difference; PANSS, positive and negative syndrome scale; SF-36v2, short form 36 version 2 health survey questionnaire; SQLS, Schizophrenia Quality of Life Scale; TMT-A, Trail Making Test A; W-L, Wilk's Lamda; WAIS-III-LNS, Wechsler Adult Intelligence scale 3rd Edition letter number sequencing; WMSR-LMI, Wechsler Memory Scale Revised Logical Memory I; WMSR-LMII, Wechsler Memory Scale Revised Logical Memory II.
Significant after Holm–Bonferroni correction.
Cohen's d calculated as (mean difference)/(s.d. pooled). Cognitive z-scores were used for cognitive analyses.
Mean difference reflects the change from baseline to 6 weeks for each condition, where a negative value is an improvement for LNS, LMI, LMII, COWAT and SF-36v2 and a positive value is an improvement for TMT-A, PANSS positive, negative, general, DASS depression, anxiety, stress and SQLS total.
Figure 2.
Treatment differences across cognitive measures in the parallel groups analyses. *P≤0.05, **P≤0.001. Figure 2 shows significant improvement from baseline to 6 weeks on measures of immediate verbal memory (Wechsler Memory Scale Revised Logical Memory I, LMI), delayed verbal memory (Wechsler Memory Scale Revised Logical Memory II, LMII), and attention/processing speed (TMT-A Trail Making Test A) in the raloxifene treatment condition. TMT-A results are inversed for comparability. Improvement on memory, attention/processing speed, and verbal fluency (COWAT Controlled Oral Word Association Test) were significantly greater in the raloxifene treatment condition relative to the placebo treatment condition (brackets). There was no significant difference between raloxifene and placebo conditions for Wechsler Adult Intelligence Scale 3rd Edition Letter-Number Sequencing (LNS) test.
Parallel groups design analysis of symptom, emotional and functional measures
Results of repeated measures (M)ANOVAs with treatment group as the independent variable and symptom severity, emotional and functional scores as dependent variables did not show any significant effects (see Table 3).
Responders analysis
Of the 40 patients administered raloxifene during the first 6-week period of the trial, 16 (40%) showed clinically reliable change on one or more cognitive measures compared to only 6 out of 39 patients (15%) in the placebo condition. The cognitive measures of Logical Memory I and II showed clinically reliable change with the responders (see Supplementary Table 8). The χ2-test of treatment response between the raloxifene and placebo groups showed a significant difference, χ2 (1)=5.6, P=0.02, with a Number Needed to Treat of 4 needed to improve cognition with raloxifene over 6 weeks.
χ2 comparison did not reveal any significant differences in relation to treatment conditions for patients with ≥20% symptom score reduction versus <20% symptom score reduction (see Supplementary Table 9). χ2-tests comparing responders and non-responders on one or more symptom, emotional and functional measures revealed no significant differences between raloxifene and placebo conditions and the odds ratio for response to raloxifene treatment on the symptom measures was 1.0 (confidence interval=0.3–2.2).
Crossover design analysis results
Treatment effects for the full 13-week crossover trial design revealed a significant treatment effect only on TMT-A, Wilk's Lambda 0.9, (1,47)=4.3, P=0.04, where the raloxifene condition showed a significant benefit, mean difference (s.d.)=−0.5, (1.0), relative to placebo, mean difference (s.d.)=−0.1, (0.7), see Supplementary Table 10. The crossover design analysis did not show any other significant effects of raloxifene in relation to cognitive, symptom, emotional or functional measures.
Discussion
Our primary results based on the parallel group design analysis demonstrates for the first time that adjunctive treatment with raloxifene at 120 mg daily in both men and women with schizophrenia is associated with cognitive improvements in verbal memory and attention/perceptual-motor processing speed. Relative to a placebo group, patients receiving raloxifene at 120 mg daily showed both statistically and clinically significant changes in cognition. These cognitive improvements support the hypothesis that raloxifene can be used as a novel therapeutic agent to ameliorate cognitive deficits in both men and women with schizophrenia.
There have been few drug treatment options to reverse cognitive deficits related to schizophrenia. Cognitive impairment in schizophrenia is an important issue, as it can negatively influence the ability to function socially and maintain employment.3, 63 A recent review of clinical trials conducted before April 2011 for cognitive-enhancing drugs in schizophrenia showed meager findings.64 Of 118 trials analyzed, only 61 were completed and five had interpretable outcomes with sufficient effect sizes to support their findings. Galantamine and minocycline have been the only reported medications to show some cognitive efficacy, although both treatments displayed only small effect sizes in the range of 0.29–0.37.65, 66 These novel treatments for cognitive deficits in schizophrenia do not act as traditional dopamine D2 receptor antagonists. However, galantamine and minocycline are not widely used as there are questions regarding efficacy and safety. Thus, the finding of a beneficial effect of raloxifene on cognitive abilities in both men and women with schizophrenia is of particular interest since it is relatively safe for use, with few adverse events requiring discontinuation as in our sample (see Table 2), when careful screening is performed to minimize the risk of potential severe adverse events. Other studies of postmenopausal women with schizophrenia, non-psychotic premenopausal women and men within the age range of participants in our study have also reported that the use of raloxifene was relatively safe and generally well tolerated.43, 45, 46, 67, 68 Although the potential for developing blood clots is a serious concern with raloxifene treatment, the risk of blood clot with raloxifene would appear to be comparable to the risk of clot with the use of some forms of oral contraceptives, although the risks in males have not been well established.
Estrogen has been associated with improved memory and attention in multiple studies of non-psychotic men and women, although there are exceptions.69, 70 Our results are consistent with findings of estrogen-promoted increases in synaptic spine density in the hippocampus and prefrontal cortex, regions linked to memory and attention.21, 22 Therefore, our findings of cognitive improvement on measures of logical memory, which has been linked to hippocampal integrity, and form A of the trail making test, which has been associated with prefrontal activation,71, 72 have support from both basic neurobiology and from work in other human conditions. The effects of raloxifene on memory and attention are consistent with previous studies of hormone and hormone modulators on cognition and in particular on verbal memory. Our effect size of 0.64 for raloxifene treatment on verbal memory in men and women with schizophrenia was comparable to the effect sizes of 0.74 and 0.69 for long-term recall and continuous long-term recall during a verbal memory test in older men who displayed mild cognitive impairment and received estradiol for 12 weeks.73
Although estrogen therapy has been similarly linked to better performance on verbal fluency tasks74 and raloxifene treatment in particular has been related to better verbal fluency in postmenopausal females with schizophrenia,46 we did not find a significant improvement in the raloxifene condition from baseline to 6 weeks on verbal fluency when examining men and women combined. However, we did find a significant difference in the direction of change in verbal fluency between the raloxifene and placebo group during period 1, with the raloxifene group improving and the placebo group declining. Although placebo group decline is not easily interpreted, it is possible that the decrease in performance in the placebo group, despite a known practice effect, was due to increased difficultly on the alternate COWAT form used at 6 weeks by comparison with the form used at baseline.75 In addition, in our supplemental analysis using sex as a grouping factor, we did show a significant interaction between sex and raloxifene treatment in which females showed a benefit of raloxifene on verbal fluency, but here again the placebo female group showed a decline in fluency.
Despite the improvements in cognition, our study did not find a significant difference between effects of raloxifene and placebo on symptom, emotional or functional measures. Previous studies of postmenopausal women with schizophrenia have shown beneficial effects of adjunctive raloxifene treatment on symptom severity assessed by PANSS.43, 45 Similarly, adjunctive estrogen treatment studies have shown significant symptom reduction primarily in women with schizophrenia, although there was at least one study showing that estrogen administration reduced symptoms in men with schizophrenia.15, 31, 34, 35, 36 The results of our present study do not support a generalized beneficial effect of raloxifene on symptoms in men and women with schizophrenia. Our patient sample was mildly to moderately ill based on PANSS-positive and -negative symptom scores and clearly had room for symptom reduction. However, equal percentages of patients in both raloxifene and placebo conditions showed symptom improvement after 6 weeks of treatment.
There are a number of limitations to our study. One limitation may have been the recruitment of patients displaying mild to moderate symptom severity on the positive and negative symptom assessment, although these patients did have room for further symptom severity reduction. Recruitment of patients without comorbidity would limit the generalizability of our results; however, the aim was to determine the extent to which adjunctive raloxifene improves cognition in schizophrenia and we also wanted to be certain to limit the risk of adverse events. Having a smaller sample size with treatment group baseline differences for the Trail Making Test and period and carryover effects are also potential limitations; however, in spite of all these factors that could have generally worked against finding a significant difference between treatment conditions, we still obtained significant effects in both the parallel group and crossover design analyses. Allowing administration of concomitant medications (for example, benzodiazepines) that may interfere with cognitive function would also be a potential limitation. However, the number of patients receiving this class of medications were relatively few and given that the number of participants receiving this class of medication was larger in the raloxifene treatment first period, the ability to find a significant beneficial effect of treatment should have been diminished in our parallel groups analysis, yet, strong, significant beneficial effects of treatment were still demonstrated. Another limitation may pertain to a concurrent change in symptoms and cognition; however, although mean symptom severity improved (for positive and general symptoms) in the raloxifene treated group, we found there was also the same or a greater degree of mean improvement in the placebo-treated group (as per Table 3). Thus, there did not appear to be an undue influence of symptoms that would be responsible for our observed beneficial effect of raloxifene on cognition. Use of a crossover design was a limitation. Crossover trials are appropriate for studies of populations with a chronic illness, where the treatment effects washout quickly, and the outcome being measured may be quickly ‘reversible.' Although schizophrenia is a chronic illness, raloxifene does have a reasonably short half-life, and cognitive and symptom measures were expected to return to near baseline with discontinuation of treatment in schizophrenia; this seems not to have been the case. Given that raloxifene modulates the hormonal estrogen receptor and hormones may propagate long-term effects such as changing gene expression, which promotes neuronal protection, synaptic growth and reduces neuroinflammation;22, 23 raloxifene may produce longer-term “carryover” effects. In future studies, raloxifene should be assessed in larger parallel group design trials over a longer duration of treatment with continued assessment after discontinuation of treatment. Treatment with raloxifene for a longer duration would be expected to be relatively safe given that the highest risk of deep vein thrombosis has been reported to be during the initial months of treatment as per the package insert.48 Also, studies of raloxifene in first-episode psychosis may be warranted as improving cognitive deficits at an early stage of the illness may improve overall prognosis.
In conclusion, our findings from a relatively large sample of men and women with schizophrenia demonstrate for the first time that adjunctive administration of raloxifene at 120 mg per day can improve cognitive outcomes particularly in the domains of verbal memory and attention in both men and women with schizophrenia. These findings also support the hypothesis of an estrogen-related disease model of schizophrenia and provide a potential novel treatment for cognitive deficits in both men and women with schizophrenia.
Acknowledgments
We thank Loretta Moore, Nick Vella, Merribel Kyaw, Selena Hu, Alice Rothwell, Richard Morris and Beverly Hisee for screening participants, performing cognitive and symptom assessments, data entry, management and monitoring. This work was supported by the University of New South Wales School of Psychiatry, the National Health and Medical Research Council (NHMRC) of Australia Project Grant no. 568807, Neuroscience Research Australia, the Schizophrenia Research Institute utilizing infrastructure funding from NSW Ministry of Health and the Macquarie Group Foundation and the Australian Schizophrenia Research Bank, which is supported by the NHMRC of Australia, the Pratt Foundation, Ramsay Health Care and the Viertel Charitable Foundation. CSW is a recipient of the National Health and Medical Research Council (Australia) Senior Research Fellowship (#1021970). JK has received support for research from: AstraZeneca, Mayne Pharma, Servier, Eli Lilly, Janssen-Cilag; honoraria as a speaker for Jansen-Cilag, Lundbeck, AstraZeneca and Bristol Myers Squib and she is an advisory board member for Janssen-Cilag, Lundbeck, Roche and Pfizer. The research described in this project was not supported by any pharmaceutical company funding. CSW has been a paid consultant for Lundbeck and Roche. PRS has received speaker fees from Janssen-Cilag.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies the paper on the Molecular Psychiatry website (http://www.nature.com/mp)
TWW was responsible for conception of the project, wrote up and revised the protocol and ethics, coordinated the project, supervised the cognitive and symptom assessors and data collection, management, monitoring and analysis, performed SCIDs and wrote and edited the manuscript. DW analyzed the data and wrote and edited the manuscript. RW managed the database, contributed to data analysis and edited the manuscript. RL, SVC, DP, and DL performed SCIDs, reviewed SCID diagnoses, assisted with the recruitment, performed medical exams and edited the manuscript. AV administered cognitive and symptom assessments, performed SCIDs, assisted with data entry and edited the manuscript. MOD, BS and JC performed the medical exams, assisted with recruitment and edited the manuscript. CG supervised the Adelaide site, performed/reviewed SCIDs, assisted with recruitment, performed medical exams and edited the manuscript. RB performed SCIDs, assisted with recruitment, administered cognitive and symptom assessments, assisted with data entry, management and monitoring and edited the manuscript. VJC, JK and PRS assisted with conception of the project and edited the manuscript. CSW was primarily involved in the conception of the project, assisted with protocol and ethics construction, coordinated the project, supervised project in relation to data collection, management, monitoring and analysis and helped to write and edit the manuscript.
Supplementary Material
References
- Levine SZ, Rabinowitz J, Ascher-Svanum H, Faries DE, Lawson AH. Extent of attaining and maintaining symptom remission by antipsychotic medication in the treatment of chronic schizophrenia: evidence from the CATIE study. Schizophr Res. 2011;133:42–46. doi: 10.1016/j.schres.2011.09.018. [DOI] [PubMed] [Google Scholar]
- Weickert TW, Goldberg TE.The course of cognitive impairment in patients with schizophreniaIn: Sharma T, Harvey P (eds). Cognition in Schizophrenia: Impairments, importance and treatment strategies Oxford University Press: New York, NY; 20003–15. [Google Scholar]
- Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia. Am J Psychiatry. 1996;153:321–330. doi: 10.1176/ajp.153.3.321. [DOI] [PubMed] [Google Scholar]
- Hyman SE. Revitalizing psychiatric therapeutics. Neuropsychopharmacology. 2014;39:220–229. doi: 10.1038/npp.2013.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke KC, Burke JD, Jr, Regier DA, Rae DS. Age at onset of selected mental disorders in five community populations. Arch Gen Psychiatry. 1990;47:511–518. doi: 10.1001/archpsyc.1990.01810180011002. [DOI] [PubMed] [Google Scholar]
- Allen KM, Fung SJ, Rothmond DA, Noble PL, Weickert CS. Gonadectomy increases neurogenesis in the male adolescent rhesus macaque hippocampus. Hippocampus. 2014;24:225–238. doi: 10.1002/hipo.22217. [DOI] [PubMed] [Google Scholar]
- Morris RW, Fung SJ, Rothmond DA, Richards B, Ward S, Noble PL, et al. The effect of gonadectomy on prepulse inhibition and fear-potentiated startle in adolescent rhesus macaques. Psychoneuroendocrinology. 2010;35:896–905. doi: 10.1016/j.psyneuen.2009.12.002. [DOI] [PubMed] [Google Scholar]
- Richards AB, Morris RW, Ward S, Schmitz S, Rothmond DA, Noble PL, et al. Gonadectomy negatively impacts social behavior of adolescent male primates. Horm Behav. 2009;56:140–148. doi: 10.1016/j.yhbeh.2009.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hafner H. Gender differences in schizophrenia. Psychoneuroendocrinology. 2003;28:17–54. doi: 10.1016/s0306-4530(02)00125-7. [DOI] [PubMed] [Google Scholar]
- Gur RE, Petty RG, Turetsky BI, Gur RC. Schizophrenia throughout life: sex differences in severity and profile of symptoms. Schizophr Res. 1996;21:1–12. doi: 10.1016/0920-9964(96)00023-0. [DOI] [PubMed] [Google Scholar]
- Goldstein JM, Link BG. Gender and the expression of schizophrenia. J Psychiatr Res. 1988;22:141–155. doi: 10.1016/0022-3956(88)90078-7. [DOI] [PubMed] [Google Scholar]
- Hafner H, Maurer K, Loffler W, Riecher- RA. The influence of age and sex on the onset and early course of schizophrenia. Br J Psychiatry. 1993;162:80–86. doi: 10.1192/bjp.162.1.80. [DOI] [PubMed] [Google Scholar]
- Gattaz WF, Vogel P, Riecher-Rossler A, Soddu G. Influence of the menstrual cycle phase on the therapeutic response in schizophrenia. Biol Psychiatry. 1994;36:137–139. doi: 10.1016/0006-3223(94)91195-9. [DOI] [PubMed] [Google Scholar]
- Hallonquist JD, Seeman MV, Lang M, Rector NA. Variation in symptom severity over the menstrual cycle of schizophrenics. Biol Psychiatry. 1993;33:207–209. doi: 10.1016/0006-3223(93)90141-y. [DOI] [PubMed] [Google Scholar]
- Riecher-Rössler A, Häfner H, Stumbaum M, Maurer K, Schmidt R. Can estradiol modulate schizophrenic symptomatology. Schizophr Bull. 1994;20:203–214. doi: 10.1093/schbul/20.1.203. [DOI] [PubMed] [Google Scholar]
- McNeil TF, Kaij L, Maimquist-Larsson A. Women with nonorganic psychosis: pregnancy's effect on mental health during pregnancy. Acta Psychiatr Scand. 1984;70:140–148. doi: 10.1111/j.1600-0447.1984.tb01191.x. [DOI] [PubMed] [Google Scholar]
- Akhondzadeh S, Rezaei F, Larijani B, Nejatisafa A-A, Kashani L, Abbasi SH. Correlation between testosterone, gonadotropins and prolactin and severity of negative symptoms in male patients with chronic schizophrenia. Schizophr Res. 2006;84:405–410. doi: 10.1016/j.schres.2006.02.008. [DOI] [PubMed] [Google Scholar]
- Vercammen A, Skilleter AJ, Lenroot R, Catts SV, Weickert CS, Weickert TW. Testosterone is inversely related to brain activity during emotional inhibition in schizophrenia. PLoS One. 2013;8:e77496. doi: 10.1371/journal.pone.0077496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore L, Kyaw M, Vercammen A, Lenroot R, Kulkarni J, Curtis J, et al. Serum testosterone levels are related to cognitive function in men with schizophrenia. Psychoneuroendocrinology. 2013;38:1717–1728. doi: 10.1016/j.psyneuen.2013.02.007. [DOI] [PubMed] [Google Scholar]
- Sherwin BB. Estrogen and cognitive functioning in women. Endocr Rev. 2003;24:133–151. doi: 10.1210/er.2001-0016. [DOI] [PubMed] [Google Scholar]
- Hao J, Rapp PR, Janssen WGM, Lou W, Lasley BL, Hof PR, et al. Interactive effects of age and estrogen on cognition and pyramidal neurons in monkey prefrontal cortex. Proc Natl Acad Sci. 2007;104:11465–11470. doi: 10.1073/pnas.0704757104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolley CS, McEwen BS. Estradiol regulates hippocampal dendritic spine density via an N-methyl-D-aspartate receptor-dependent mechanism. J Neurosci. 1994;14:7680–7687. doi: 10.1523/JNEUROSCI.14-12-07680.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Cheng CM, Zhou J, Smith A, Weickert CS, Perlman WR, et al. Estradiol alters transcription factor gene expression in primate prefrontal cortex. J Neurosci Res. 2004;76:306–314. doi: 10.1002/jnr.20076. [DOI] [PubMed] [Google Scholar]
- Perlman WR, Tomaskovic-Crook E, Montague DM, Webster MJ, Rubinow DR, Kleinman JE, et al. Alteration in estrogen receptor alpha mRNA levels in frontal cortex and hippocampus of patients with major mental illness. Biol Psychiatry. 2005;58:812–824. doi: 10.1016/j.biopsych.2005.04.047. [DOI] [PubMed] [Google Scholar]
- Montague D, Weickert CS, Tomaskovic-Crook E, Rothmond DA, Kleinman JE, Rubinow DR. Oestrogen receptor alpha localisation in the prefrontal cortex of three mammalian species. J Neuroendocrinol. 2008;20:893–903. doi: 10.1111/j.1365-2826.2008.01743.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlman WR, Matsumoto M, Beltaifa S, Hyde TM, Saunders RC, Webster MJ, et al. Expression of estrogen receptor alpha exon-deleted mRNA variants in the human and non-human primate frontal cortex. Neuroscience. 2005;134:81–95. doi: 10.1016/j.neuroscience.2005.03.055. [DOI] [PubMed] [Google Scholar]
- Weickert CS, Miranda-Angulo AL, Wong J, Perlman WR, Ward SE, Radhakrishna V, et al. Variants in the estrogen receptor alpha gene and its mRNA contribute to risk for schizophrenia. Hum Mol Genet. 2008;17:2293–2309. doi: 10.1093/hmg/ddn130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong J, Weickert CS. Transcriptional interaction of an estrogen receptor splice variant and ErbB4 suggests convergence in gene susceptibility pathways in schizophrenia. J Biol Chem. 2009;284:18824–18832. doi: 10.1074/jbc.M109.013243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeBlanc ES, Janowsky J, Chan BKS, Nelson HD. Hormone replacement therapy and cognition: systematic review and meta-analysis. JAMA. 2001;285:1489–1499. doi: 10.1001/jama.285.11.1489. [DOI] [PubMed] [Google Scholar]
- Good KP, Kopala LC, Martzke JS, Fluker M, Seeman MV, Parish B, et al. Hormone replacement therapy in postmenopausal women with schizophrenia: preliminary findings. Schizophr Res. 1999.
- Kulkarni J, Gavrilidis E, Wang W, Worsley R, Fitzgerald PB, Gurvich C, et al. Estradiol for treatment-resistant schizophrenia: a large-scale randomized-controlled trial in women of child-bearing age. Mol Psychiatry. 2014. [DOI] [PubMed]
- Ko Y-H, Joe S-H, Cho W, Park J-H, Lee J-J, Jung I-K, et al. Effect of hormone replacement therapy on cognitive function in women with chronic schizophrenia. Int J Psychiatry Clin Pract. 2006;10:97–104. doi: 10.1080/13651500500526235. [DOI] [PubMed] [Google Scholar]
- Begemann MJH, Dekker CF, van Lunenburg M, Sommer IE. Estrogen augmentation in schizophrenia: a quantitative review of current evidence. Schizophr Res. 2012;141:179–184. doi: 10.1016/j.schres.2012.08.016. [DOI] [PubMed] [Google Scholar]
- Kulkarni J, de Castella A, Smith D, Taffe J, Keks N, Copolov D. A clinical trial of the effects of estrogen in acutely psychotic women. Schizophr Res. 1996;20:247–252. doi: 10.1016/0920-9964(96)82949-5. [DOI] [PubMed] [Google Scholar]
- Kulkarni J, de Castella A, Headey B, Marston N, Sinclair K, Lee S, et al. Estrogens and men with schizophrenia: is there a case for adjunctive therapy. Schizophr Res. 2011;125:278–283. doi: 10.1016/j.schres.2010.10.009. [DOI] [PubMed] [Google Scholar]
- Kulkarni J, de Castella A, Fitzgerald PB, Gurvich CT, Bailey M, Bartholomeusz C, et al. Estrogen in severe mental illness: a potential new treatment approach. Arch Gen Psychiatry. 2008;65:955–960. doi: 10.1001/archpsyc.65.8.955. [DOI] [PubMed] [Google Scholar]
- Barrett-Connor E, Stuenkel CA. Hormone replacement therapy (HRT)—risks and benefits. Int J Epidemiol. 2001;30:423–426. doi: 10.1093/ije/30.3.423. [DOI] [PubMed] [Google Scholar]
- Landry M, Lévesque D, Di Paolo T, Eacute R, Egrave S. Estrogenic properties of raloxifene, but not tamoxifen, on D2 and D3 dopamine receptors in the rat forebrain. Neuroendocrinology. 2002;76:214–222. doi: 10.1159/000065951. [DOI] [PubMed] [Google Scholar]
- Khan MM, Wakade C, de Sevilla L, Brann DW. Selective estrogen receptor modulators (SERMs) enhance neurogenesis and spine density following focal cerebral ischemia. J Steroid Biochem Mol Biol. 2014;146:38–47. doi: 10.1016/j.jsbmb.2014.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Burgos I, Rivera-Cervantes MC, Velázquez-Zamora DA, Feria-Velasco A, Garcia-Segura LM. Selective estrogen receptor modulators regulate dendritic spine plasticity in the hippocampus of male rats. Neural Plast. 2011;2012:309494. doi: 10.1155/2012/309494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goekoop R, Duschek EJ, Knol DL, Barkhof F, Netelenbos C, Scheltens P, et al. Raloxifene exposure enhances brain activation during memory performance in healthy elderly males; its possible relevance to behavior. NeuroImage. 2005;25:63–75. doi: 10.1016/j.neuroimage.2004.11.012. [DOI] [PubMed] [Google Scholar]
- Nickelsen T, G Lufkin E, Lawrence Riggs B, A Cox D, H Crook T. Raloxifene hydrochloride, a selective estrogen receptor modulator: safety assessment of effects on cognitive function and mood in postmenopausal women. Psychoneuroendocrinology. 1999;24:115–128. doi: 10.1016/s0306-4530(98)00041-9. [DOI] [PubMed] [Google Scholar]
- Usall J, Huerta-Ramos E, Iniesta R, Cobo J, Araya S, Roca M, et al. Raloxifene as an adjunctive treatment for postmenopausal women with schizophrenia: a double-blind, randomized, placebo-controlled trial. J Clin Psychiatry. 2011;72:1552. doi: 10.4088/JCP.10m06610. [DOI] [PubMed] [Google Scholar]
- Wong J, Seeman MV, Shapiro H. Case report: raloxifene in postmenopausal women with psychosis: preliminary findings. Am J Geriatric Psychiatry. 2003;11:697–698. doi: 10.1176/appi.ajgp.11.6.697. [DOI] [PubMed] [Google Scholar]
- Kulkarni J, Gurvich C, Lee SJ, Gilbert H, Gavrilidis E, de Castella A, et al. Piloting the effective therapeutic dose of adjunctive selective estrogen receptor modulator treatment in postmenopausal women with schizophrenia. Psychoneuroendocrinology. 2010;35:1142–1147. doi: 10.1016/j.psyneuen.2010.01.014. [DOI] [PubMed] [Google Scholar]
- Huerta-Ramos E, Iniesta R, Ochoa S, Cobo J, Miquel E, Roca M, et al. Effects of raloxifene on cognition in postmenopausal women with schizophrenia: a double-blind, randomized, placebo-controlled trial. Eur Neuropsychopharmacol. 2014;24:223–231. doi: 10.1016/j.euroneuro.2013.11.012. [DOI] [PubMed] [Google Scholar]
- First MB. Structured clinical interview for DSM-IV-TR axis I disorders: SCID-I: biometrics research department. New York State Psychiatric Institutute. 2007.
- Raloxifene: Highlights of Prescribing Information: Eli Lilly and Company 2011. Available at http://pi.lilly.com/us/evista-pi.pdf .
- Wechsler D.Wechsler Adult Intelligence Scale3rd ednPyschological Corporation: San Antonio, TX, USA; 2001 [Google Scholar]
- Wechsler D.Wechsler Test of Adult Reading The Psychological Corporation: San Antonio, TX; USA2001 [Google Scholar]
- Lezak M.Neuropsychological Assessment4th ednOxford University Press: New York, NY; 2004 [Google Scholar]
- Reitan RWD. Neuropsychological Press: Tucson, AZ, USA; 1985. The Halstead-Reitan Neuropsychological Test Battery: Therapy and Clinical Interpretation. [Google Scholar]
- Wechsler D.Wechsler Memory Scale-Revised The Psychological Corporation: San Antonio, TX; USA, 1987 [Google Scholar]
- Kay SR, Flszbein A, Opfer LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Lovibond S, Lovibond P.Manual for the Depression Anxiety Stress Scale2nd ednPsychology Foundation: Sydney, Australia; 1995 [Google Scholar]
- Ware JE, Kosinski M, Dewey JE, Gandek B. SF-36 health survey: manual and interpretation guide: Quality Metric Inc. 2000.
- Wilkinson G, Hesdon B, Wild D, Cookson R, Farina C, Sharma V, et al. Self-report quality of life measure for people with schizophrenia: the SQLS. Br J Psychiatry. 2000;177:42–46. doi: 10.1192/bjp.177.1.42. [DOI] [PubMed] [Google Scholar]
- Woods JR, Williams JG, Tavel M. The two-period crossover design in medical research. Ann Int Med. 1989;110:560–566. doi: 10.7326/0003-4819-110-7-560. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol. 1991;59:12. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Williams LM, Simms E, Clark CR, Paul RH, Rowe D, Gordon E. The test-retest reliability of a standardized neurocognitive and neurophysiological test battery:“neuromarker”. Int J Neurosci. 2005;115:1605–1630. doi: 10.1080/00207450590958475. [DOI] [PubMed] [Google Scholar]
- Kane J, Honigfeld G, Singer J, Meltzer H. Clozapine for the treatment-resistant schizophrenic: a double-blind comparison with chlorpromazine. Arch Gen Psychiatry. 1988;45:789. doi: 10.1001/archpsyc.1988.01800330013001. [DOI] [PubMed] [Google Scholar]
- Buchanan RW, Davis M, Goff D, Green MF, Keefe RSE, Leon AC, et al. A summary of the FDA-NIMH-MATRICS workshop on clinical trial design for neurocognitive drugs for schizophrenia. Schizophr Bull. 2005;31:5–19. doi: 10.1093/schbul/sbi020. [DOI] [PubMed] [Google Scholar]
- McGurk SR, Meltzer HY. The role of cognition in vocational functioning in schizophrenia. Schizophr Res. 2000;45:175–184. doi: 10.1016/s0920-9964(99)00198-x. [DOI] [PubMed] [Google Scholar]
- Keefe RSE, Buchanan RW, Marder SR, Schooler NR, Dugar A, Zivkov M, et al. Clinical trials of potential cognitive-enhancing drugs in schizophrenia: what have we learned so far. Schizophr Bull. 2013;39:417–435. doi: 10.1093/schbul/sbr153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levkovitz Y, Mendlovich S, Riwkes S, Braw Y, Levkovitch-Verbin H, Gal G, et al. A double-blind, randomized study of minocycline for the treatment of negative and cognitive symptoms in early-phase schizophrenia. J Clin Psychiatry. 2010;71:138. doi: 10.4088/JCP.08m04666yel. [DOI] [PubMed] [Google Scholar]
- Buchanan R, Conley R, Dickinson D, Ball M, Feldman S, Gold J, et al. Galantamine for the treatment of cognitive impairments in people with schizophrenia. Am J Psychiatry. 2008;165:82–89. doi: 10.1176/appi.ajp.2007.07050724. [DOI] [PubMed] [Google Scholar]
- Eng-Wong J, Reynolds JC, Venzon D, Liewehr D, Gantz S, Danforth D, et al. Effect of raloxifene on bone mineral density in premenopausal women at increased risk of breast cancer. J Clin Endocrinol Metab. 2006;91:3941–3946. doi: 10.1210/jc.2005-2827. [DOI] [PubMed] [Google Scholar]
- Uebelhart B, Herrmann F, Pavo I, Draper MW, Rizzoli R. Raloxifene treatment is associated with increased serum estradiol and decreased bone remodeling in healthy middle-aged men with low sex hormone levels. J Bone Miner Res. 2004;19:1518–1524. doi: 10.1359/JBMR.040503. [DOI] [PubMed] [Google Scholar]
- Boss L, Kang D-H, Marcus M, Bergstrom N. Endogenous sex hormones and cognitive function in older adults a systematic review. West J Nurs Res. 2014;36:388–426. doi: 10.1177/0193945913500566. [DOI] [PubMed] [Google Scholar]
- Salminen EK, Portin RI, Koskinen AI, Helenius HYM, Nurmi MJ. Estradiol and cognition during androgen deprivation in men with prostate carcinoma. Cancer. 2005;103:1381–1387. doi: 10.1002/cncr.20962. [DOI] [PubMed] [Google Scholar]
- Zakzanis KK, Mraz R, Graham SJ. An fMRI study of the Trail Making Test. Neuropsychologia. 2005;43:1878–1886. doi: 10.1016/j.neuropsychologia.2005.03.013. [DOI] [PubMed] [Google Scholar]
- Sass KJ, Sass A, Westerveld M, Lencz T, Novelly RA, Kim JH, et al. Specificity in the correlation of verbal memory and hippocampal neuron loss: dissociation of memory, language, and verbal intellectual ability. J Clin Exp Neuropsychol. 1992;14:662–672. doi: 10.1080/01688639208402854. [DOI] [PubMed] [Google Scholar]
- Sherwin BB, Chertkow H, Schipper H, Nasreddine Z. A randomized controlled trial of estrogen treatment in men with mild cognitive impairment. Neurobiol Aging. 2011;32:1808–1817. doi: 10.1016/j.neurobiolaging.2009.11.002. [DOI] [PubMed] [Google Scholar]
- Yonker JE, Adolfsson R, Eriksson E, Hellstrand M, Nilsson L-G, Herlitz A. Verified hormone therapy improves episodic memory performance in healthy postmenopausal women. Aging Neuropsychol Cogn. 2006;13:291–307. doi: 10.1080/138255890968655. [DOI] [PubMed] [Google Scholar]
- Barry D, Bates ME, Labouvie E. FAS and CFL forms of verbal fluency differ in difficulty: a meta-analytic study. Appl Neuropsychol. 2008;15:97–106. doi: 10.1080/09084280802083863. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.