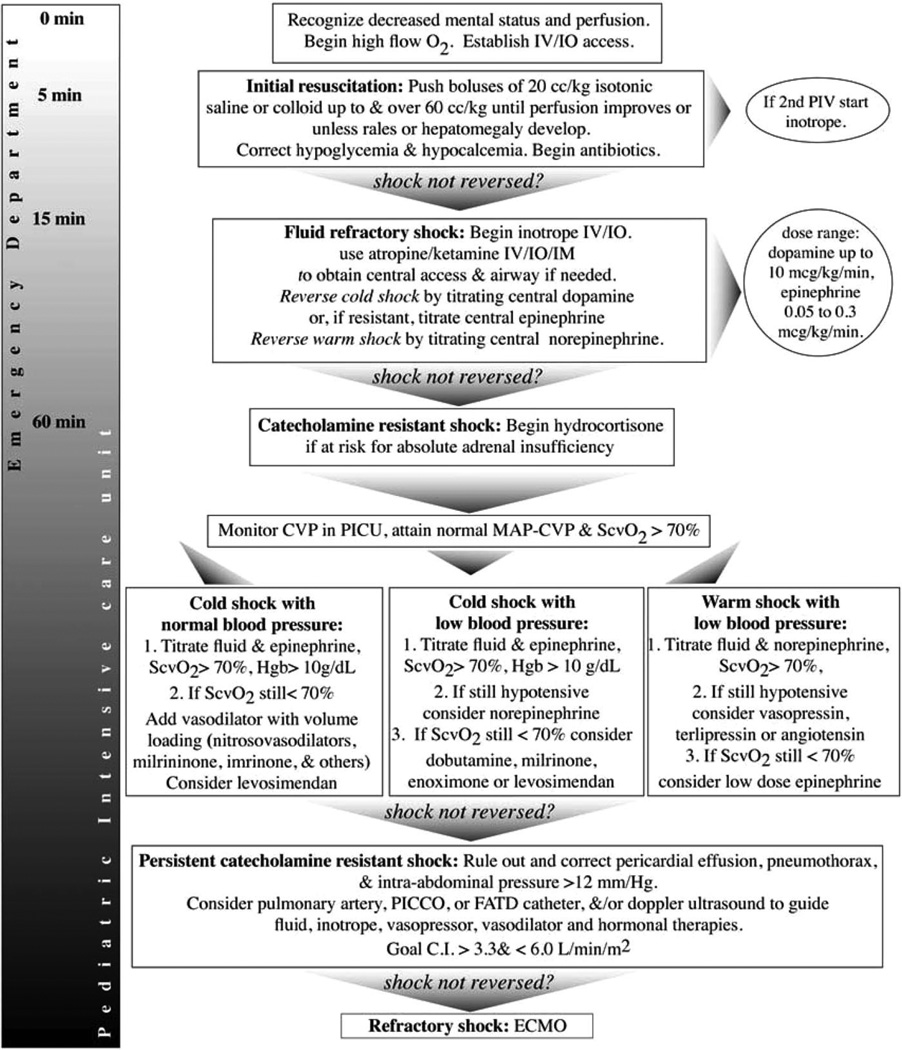
Figure 1.
Algorithm for time sensitive, goal-directed stepwise management of hemodynamic support in infants and children. Proceed to next step if shock persists. 1) First hour goals—Restore and maintain heart rate thresholds, capillary refill ≤2 sec, and normal blood pressure in the first hour/emergency department. Support oxygenation and ventilation as appropriate. 2) Subsequent intensive care unit goals—If shock is not reversed, intervene to restore and maintain normal perfusion pressure (mean arterial pressure [MAP]-central venous pressure [CVP]) for age, central venous O2 saturation >70%, and CI >3.3, <6.0 L/min/m2 in pediatric intensive care unit (PICU). Hgb, hemoglobin; PICCO, pulse contour cardiac output; FATD, femoral arterial thermodilution; ECMO, extracorporeal membrane oxygenation; CI, cardiac index; CRRT, continuous renal replacement therapy; IV, intravenous; IO, interosseous; IM, intramuscular.