Abstract
Objective
To test the effectiveness of a work-focused intervention (WFI) on the work outcomes of employed adults with dysthymia.
Method
This subgroup analysis from a randomized controlled trial compares an initial sample of 167 employees (age ≥ 45 years), screened for dysthymia using the PC-SAD without current major depressive disorder randomized to WFI (n=85) or usual care (UC) (n=82). Study sites included 19 employers and five additional organizations. Telephone-based WFI counseling (eight, twice monthly 50-minute sessions) provided work coaching and modification, care coordination and cognitive-behavioral therapy (CBT). Adjusted mixed effects models compared the WFI versus UC group pre-intervention to four-month post-intervention change in at-work limitations measured by the Work Limitations Questionnaire. Secondary outcome analysis compared the change in self-reported absences and depression symptom severity (PHQ-9 scores).
Results
Work productivity loss scores improved 43.0% in the WFI group vs. 4.8% in UC (difference in change P < 0.001). Absence days declined by 58.3% in WFI vs. 0.0% in UC (difference in change P = .09). Mean PHQ-9 depression symptom severity declined 44.2% in WFI vs. 5.3% in UC (difference in change P < 0.001).
Conclusion
At four months, the WFI was more effective than UC on two of the three outcomes. It could be an important mental and functional health improvement resource for the employed dysthymic population.
Keywords: Dysthymia, Outcome Studies, Work Productivity, Economic Issues, Occupational Psychiatry, Mood Disorder
1. Introduction
Individuals with a range of persistent subthreshold depressive symptoms include those formerly labeled dysthymia and in the DSM-5 as persistent depressive disorder (PPD) [1]. These are common chronic condition associated with a range of depression symptoms and limitations in social and occupational functioning [1–7]. While its symptoms are less severe than those associated with major depressive disorder (MDD), most individuals (50–75%) with dysthymia also experience recurrent episodes of MDD as well as having functional impairments [2–6, 8, 9]. The DSM revisions reflect both the difficulty involved in classifying individuals with chronic depression who do not meet criteria for MDD and establishing a definition that captures the specific burden this condition places on patients. In this study, which was conducted prior to the DSM-5 revisions, the term dysthymia is used to study individuals who screened positive for dysthymia symptom criteria but who were not currently experiencing MDD.
Research has already demonstrated that, among working age adults in the United States, MDD is a leading source of work disability and diminished work productivity exacting a large cost in quality of life and the nation’s economy [10–12]. Compared to the evidence concerning the relationship between depression symptoms and work outcomes for individuals with MDD [13–15], a sparse literature exists regarding individuals with chronic depressive symptoms, much of it focused on dysthymia. In studies comparing individuals with dysthymia to non-depressed control patients, dysthymics have higher levels of unemployment and work outcomes, such as job loss and turnover, similar to those associated with MDD [3]. There is a greater likelihood of comorbid psychiatric diagnoses and problems with substance abuse, which can make it difficult to obtain and retain employment [3, 5, 6, 16, 17]. Additionally, compared to healthy control employees, adults with dysthymia have significantly more unstable job histories and lower current earnings [12, 18]. Observational studies have found these individuals have more work productivity loss, disability days and chronic restriction of activity [14, 19]. Experimental studies have shown that, compared to employed controls without dysthymia, those with dysthymia have poorer work performance and at-work productivity [12, 18, 20–23].
Despite the availability of effective treatments for dysthymia and the condition’s known adverse psychosocial consequences, including those affecting employment, patients with dysthymia are frequently undertreated [3, 24]. Conflicting findings regarding the effectiveness of medications and psychotherapeutic approaches for improving symptoms remains a barrier to care. Thase [25] found that antidepressant medication was more effective than placebo in treating depression symptoms in patients with dysthymia [25] and a meta-analysis investigating the efficacy of antidepressant medication for MDD and dysthymia found it effective for both, with a greater margin of efficacy for those with dysthymia vs. MDD [26]. Contrary to these findings, a meta-analysis found that the effectiveness of antidepressant medication was positively correlated to depression symptom severity with little to no benefit for patients at mild or moderate depression symptom levels [27]. Several small RCTs found promising treatment results for combined antidepressant and psychotherapeutic interventions [7, 28–31]. Studies testing Internet and telephonic-based psychotherapeutic interventions (e.g., CBT for dysthymia) have shown modest improvements in depression symptoms [32, 33].
Few studies have addressed the effectiveness of either antidepressant medication or psychotherapy for achieving improvements in functioning, including functioning in employment among individuals with chronic depressive symptoms without current MDD. A focus on this outcome is important because research on treating depressive disorders has shown that functioning may fail to improve despite improvements in depression symptom severity [34, 35], suggesting that treating symptoms alone may not be adequate for restoring functioning in employment. Influenced by research on chronic health problems and work disability, such as musculoskeletal pain [36], in which return to effective functioning is regarded as an important goal, and research addressing employment supports for adults with chronic and severe mental illness [37], we considered that employees with probable dysthymia may also benefit from work-focused care addressing the medical, psychosocial, and environmental dimensions of functioning in employment. We developed a novel multi-component work-focused intervention (WFI) program, for employees with depression. Previously, a pilot randomized controlled trial (RCT) of the WFI demonstrated its superiority over usual care (UC) for reducing absenteeism, presenteeism, and depression symptom severity for individuals with MDD [38]. In a subsequent large-scale RCT for a sample screened for MDD and/or dysthymia, the WFI was superior to UC in reducing presenteeism (at work productivity loss), absenteeism, and depression symptom severity for the total treatment population [39].
The present study is a subgroup analysis of data from the large-scale RCT (which was not specified in the original trial registration: NCT01163890). This analysis focuses on study participants screened for dysthymia not meeting criteria for current MDD. This study tested the WFI in employed adults age 45 years of age or older who may be especially vulnerable to the disabling effects of chronic illness [40]. The primary hypothesis is that the WFI is superior to UC for reducing at work productivity loss. A secondary hypothesis is that the WFI is superior for reducing absenteeism and depression symptom severity.
2. Methods
2.1 Design Overview
Between 2010 and 2013 a population-based RCT enrolled eligible, consenting employed adults screened for MDD and/or dysthymia, randomizing to either the experimental WFI or UC group. Eligibility criteria included: age 45 years or older; employed; current MDD using the PHQ-9 as a screener [41], dysthymia using the PC-SAD as a screener [42], or double depression (both MDD and dysthymia); with work limitations [39]. In this subgroup analysis, study participants screened for dysthymia and no MDD were included (N = 167).
Dysthymia was defined as a minimum of two out of six DSM-IV persistent depressive symptoms lasting two years or longer, according to the PC-SAD questionnaire [42]. The PC-SAD has a sensitivity of 87% and specificity of 95%, comparable to the diagnostic accuracy associated with other depression screeners [42]. Work limitations were signified by an at-work productivity loss of score of >= 5% from the Work Limitations Questionnaire (WLQ), a validated measurement tool [12, 43–45]. The WLQ, used in a variety of healthcare and employment settings, measures the degree to which physical and/or mental health problems (such as depression) interfere with a person’s performance of common job tasks and work productivity. A 5% score is consistent with work limitations approximately 20% of the time over the course of two weeks. All questionnaires have been validated specifically for depressed groups including the PHQ-9 [41], which was used for determining depressive symptom severity [38, 39]. Exclusions were made for psychosis, bipolar disorder, current alcohol abuse [46], non-English speaking, and severe physical limitations indicated by an SF-12 Physical Component Score (PCS) of ≤ 35 [47].
As described elsewhere in more detail [39], eligibility screening on a privacy protected website was offered in 24 sites: 13 private sector employers, six public sector employers, and five employee benefits organizations with access to employed populations. Each site disseminated primarily electronic study advertisements inviting employees (and, at some sites, adult dependents) to access the screener, which could be completed at any time convenient to the individual. Screening was voluntary and anonymous and immediate personalized electronic feedback about depression symptom severity and at-work limitation levels was given
Enrollment required the completion of an electronic informed consent form a self-report baseline (pre-intervention) questionnaire and contact information. Randomization to the WFI or UC group occurred next using an automated 1:1 scheme for the overall sample; sample sizes were comparable (85 vs. 82) for the subgroup. All participants were given web links to depression information and care resources (e.g. EAP, primary care or behavioral health) through their affiliated study site [38, 45]. During the study, participants were not restricted from using other services. The final post-intervention questionnaire was administered online on the study’s website four months after the baseline. Employees were offered small monetary incentives for completing both questionnaires. The Tufts Medical Center/Tufts University Institutional Review Board reviewed and approved the study protocol.
2.2 Experimental Intervention
The WFI is an eight session, 50-minute twice monthly telephonic intervention provided by masters-level counselors with EAP experience (four month total duration). A team of 11 EAP counselors, employed by Optum, a health services provider headquartered in Eden Prairie, MN, participated in the study and received specialized WFI training and supervision from the study’s multidisciplinary team. Counselors documented the WFI care process in the study’s electronic information system, which the research team monitored.
The WFI has three integrated modalities. Each one addresses a specific barrier to effective functioning and stresses the acquisition of self-care strategies through a combination of “homework” assignments, counselor feedback, and motivational interviewing to optimize functional outcomes using vocational, medical, and psychological strategies.
2.2.1 Work Coaching and Modification
Work coaching/modification reflects disability theory and addresses barriers to functioning due to imbalances between the characteristics of the worker and those within the job and work environment [48]. Specific job performance difficulties related to depression are targeted, guiding the employee to change modifiable aspects of work methods and/or work conditions with no direct counselor contact with the workplace. Guided by the WLQ questions and knowledge of work organization, the WFI counselor assesses work performance problems, barriers to effective functioning, and available resources and supports. Using ideas adapted from diverse fields (e.g., disability management, vocational rehabilitation, supported employment and management), the counselor offers specific recommendations for changing work behaviors, work processes and/or environmental conditions, and, in some cases, for adopting compensatory skills or behaviors. Work modifications are informal, not requiring employer approval or formal accommodation.
2.2.2 Care Coordination
Care coordination addresses barriers to functional improvement related to a misalignment of goals and expectations among the individual with depression, his or her regular provider and the counselor. Drawing from the collaborative care model [49], counselors provide psycho-education (filling in gaps in knowledge of depression, treatment and work) and motivational enhancement (promoting active engagement in care). The counselor promotes three-way participant-provider-counselor communication by assessing depression symptom severity, medication effectiveness, emerging medication side effects or adherence issues, and work limitations monthly and sharing results. Counselors outreach to the employee and his or her primary care physician (PCP) or prescribing provider to promote adherence to already prescribed antidepressants and the use of evidence-based depression treatment (including clinical follow-up for inadequate antidepressant response).
2.2.3 Work-Focused CBT
Work-focused cognitive behavioral therapy (CBT) strategies, based on Beck and others [50, 51], addresses psychological barriers to functional improvement. With counselor guidance and a workbook, participants learn to identify the thoughts, feelings and behaviors that are eroding work functioning and respond using more effective coping strategies. This process is guided by Creating a Balance [52], a manual providing behavioral and cognitive homework exercises for improving coping skills, which was modified to include work examples. In the WFI, the counselor and employee co-create a care plan for dealing with each functional problem and review specific assignments and progress at each session.
2.3 Measures
The primary endpoint is a presenteeism measure, the WLQ at-work productivity loss (PL) score, measured at baseline and four-month follow-up. PL quantifies the estimated difference in health-related at-work productivity loss between a person (or group) completing the WLQ and an external benchmark sample of healthy workers. The WLQ is a validated self-report survey tool for assessing the impact of health problems, including depression, on at-work performance (presenteeism) and productivity loss [12, 43]. The WLQ generates four at-work performance scale scores reflecting the percentage of time in the prior two weeks that emotional and/or physical health problems limited ability to perform specific job tasks: time management, performance of physical tasks, mental-interpersonal tasks, and output tasks (e.g., handling the workload and finishing work on time). Scores range from 0% (limited none of the time) to 100% (limited all of the time). To compute PL, scores from each of the four WLQ work performance scales are multiplied by a specific weight and the products are summed. Weights were obtained from validation research in which each WLQ scale score was regressed on objective work output [43]. Hence, weights are regression coefficients obtained from modeling the relationship of WLQ scale scores to actual productivity. The PL score corresponds to the estimated work productivity loss attributable to health problems.
Health-related absenteeism in the past two weeks, a secondary endpoint of the study, was measured using the WLQ Time Loss Module. Productivity loss due to absences (APL) is the ratio of hours missed due to health or medical care divided by the number of hours usually spent working.
Depression symptom severity is a secondary endpoint measured by the PHQ-9 [41, 53]. Although designed to measure symptoms of MDD and other depressive syndromes, individuals with dysthymia experience depressive symptoms the severity of which can also be evaluated by the PHQ-9 [41].
The main independent variable is the treatment group indicator. Covariates include baseline (pre-intervention) demographics (e.g., age, gender, education, race/ethnicity, marital status, and annual earnings), job descriptors (e.g., occupation), self-reported chronic medical comorbidities, number of medical and mental health provider visits in the past four months, current and past antidepressant medication usage and study site.
2.4 Statistical Analysis
Prior to hypothesis-testing, data quality was assessed and descriptive statistics were computed including means, standard deviations (SDs), medians, inter-quartile ranges (IQRs), frequencies, and percentages. Tests included chi-square, t-test, and analysis of variance (ANOVA) as appropriate. Power analysis was conducted at the overall sample level but not at the subgroup level.
Based on recommendations of Lane [54] and others [55], mixed effects modeling was used to assess the baseline to follow-up change in each study outcome by assuming a person-level random effect. The models take the form of yij= xijβ + uj + εij where yij is the outcome of jth individual at ith time (baseline or follow-up); β is a vector of the fixed effects including a fixed intercept; xij is the design matrix of observables including the intention-to-treat (ITT) treatment indicator, time indicator, baseline value of the outcome variable, study site indicators and all other covariates such as baseline age, gender, race/ethnicity, marital status, occupation, number of physical comorbidities, and full-time or part-time employment; uj is a normally distributed random intercept for jth individual with mean zero and variance of ψ2; and εij is random error with mean zero and variance σ2 Adjusted means, confidence intervals, P values and effect sizes are reported. Effect sizes for changes within treatment group were defined as the average change within group divided by the SD of baseline scores. An effect size of 0.8 or more was considered large (large enough to be observable for each subject) whereas an effect size of 0.2 or less was defined as small [56]. A sensitivity analysis was done on drop-out using a more conservative approach by conducting the last observation carried forward (LOCF). An additional analysis was done testing the sensitivity of the results of individuals with a PHQ-9 severity score of ≤9 versus a PHQ-9 severity score of 10 or more. STATA 9.0 [57] was used for all analyses.
3. Results
Of 18,102 employees screened for the larger study, 1,227 (6.8%) were eligible and 431 of those eligible (35.1%) consented to the larger study [39].
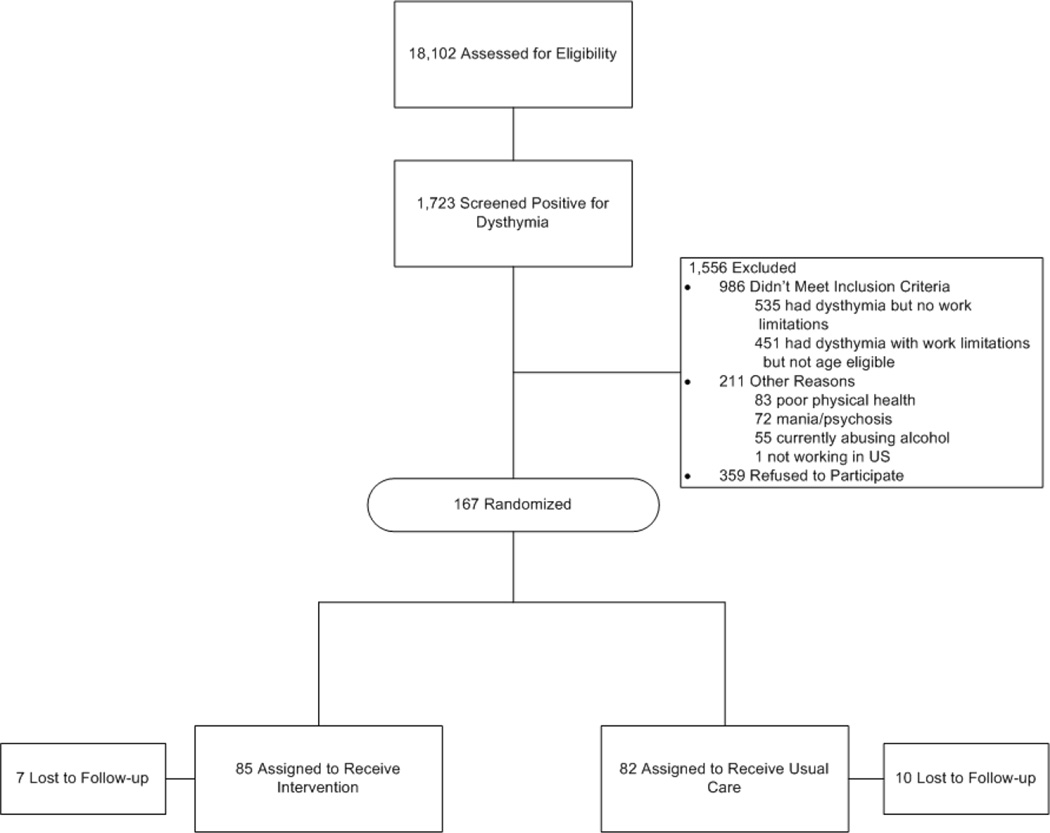
The analysis for this study includes the 167 participants screened for dysthymia (WFI = 85 and UC = 82); (Figure 1). Seven (8%) employees in the WFI group and 10 (12%) of the UC group did not complete the self-report follow-up questionnaire and were considered lost to follow-up. Although the randomization was not designed to minimize WFI vs. UC differences at the subgroup level there were no significant baseline differences either between those participants with or without a final questionnaire or between the WFI and UC groups, except that the UC group initially had a higher mean number of chronic comorbid medical conditions than the WFI group (3.2 vs. 2.6, respectively; P = .03; Table 1).
Figure 1.
CONSORT Diagram for Randomized Controlled Trial (RCT) of an Experimental Work-Focused Intervention for Employed Adults with Depression and Work Limitations
Table 1.
Starting Sample Baseline Characteristics Comparing Employed Adults with Dysthymia and Work Limitations in Experimental Work-Focused Intervention vs. Usual Care
| Characteristics | Total (n=167) |
Work- Focused Intervention (n=85) |
Usual Care (n=82) |
P | |||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| Age, y (M±SD) | 54.6±6.0 | 54.3±5.2 | 55.0±6.7 | .46 | |||
| Female | 123 | 73.7 | 61 | 71.8 | 62 | 75.6 | .58 |
| White non-Hispanic | 145 | 87.3 | 78 | 91.8 | 67 | 82.7 | .08 |
| Marital Status | |||||||
| Married | 83 | 49.7 | 40 | 47.1 | 43 | 52.4 | .49 |
| Not married | 84 | 50.3 | 45 | 52.9 | 39 | 47.6 | |
| Education | |||||||
| Less than high school | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | .13 |
| High school graduate | 9 | 5.4 | 2 | 2.4 | 7 | 8.5 | |
| Some college, no degree | 26 | 15.6 | 9 | 10.6 | 17 | 20.7 | |
| Associate's degree | 11 | 6.6 | 6 | 7.1 | 5 | 6.1 | |
| Bachelor's degree | 49 | 29.3 | 27 | 31.8 | 22 | 26.8 | |
| Post-bachelor’s degree | 72 | 43.1 | 41 | 48.2 | 31 | 37.8 | |
| Annual income, median (Median±IQR) | 60000±38472 | 58192±38109 | 64808±37246 | .38 | |||
| Works 35 hours/week or more | 148 | 88.6 | 77 | 90.6 | 71 | 86.6 | .42 |
| Weekly hours (M±SD) | 42.6±10.8 | 43.6±10.7 | 41.5±10.9 | .20 | |||
| Occupation | |||||||
| White collar | 123 | 73.7 | 65 | 76.5 | 58 | 70.7 | .18 |
| Blue collar | 5 | 3.0 | 4 | 4.7 | 1 | 1.2 | |
| Sales, support and service | 39 | 23.4 | 16 | 18.8 | 23 | 28.0 | |
| In job for five years or longer | 97 | 58.1 | 47 | 55.3 | 50 | 61.0 | .46 |
| Union member | 43 | 25.7 | 21 | 24.7 | 22 | 26.8 | .76 |
| Self-employed | 8 | 4.8 | 4 | 4.7 | 4 | 4.9 | .96 |
| Depression, (M±SD) | |||||||
| Symptom severity score, PHQ-9a | 9.5±2.6 | 9.5±2.7 | 9.4±2.5 | .72 | |||
| Comorbid condition | |||||||
| Comorbidity presentb | 150 | 89.8 | 75 | 88.2 | 75 | 91.5 | .49 |
| No. of comorbidities, (M±SD) | 2.9±1.9 | 2.6±1.8 | 3.2±1.9 | .03 | |||
| Depression treatment history | |||||||
| Ever had antidepressant | 137 | 82.0 | 70 | 82.4 | 67 | 81.7 | .92 |
| Antidepressant in past month | 101 | 60.5 | 53 | 62.4 | 48 | 58.5 | .62 |
| Healthcare providers seen past four months | |||||||
| Primary care provider | 44 | 26.5 | 21 | 25.0 | 23 | 28.0 | .66 |
| Psychiatrist/psychiatric nurse | 50 | 29.9 | 25 | 29.4 | 25 | 30.5 | .88 |
| Other mental health providerc | 45 | 26.9 | 23 | 27.1 | 22 | 26.8 | .98 |
| Percent time with work limitations past two weeks, (M±SD)d | |||||||
| Time management | 34.3±18.4 | 35.0±17.9 | 33.5±19.1 | .61 | |||
| Physical tasks | 17.9±17.3 | 18.9±17.6 | 16.8±16.8 | .45 | |||
| Mental-interpersonal tasks | 30.8±13.4 | 30.3±13.1 | 31.4±13.8 | .63 | |||
| Output tasks | 34.8±20.3 | 36.4±19.8 | 33.1±20.7 | .31 | |||
| Percentage at-work productivity loss | 8.5±3.6 | 8.6±3.4 | 8.4±3.8 | .69 | |||
| Absences due to health or medical care (M±SD)e | |||||||
| Days missed per 2 weeks | 1.1±1.7 | 1.2±2.0 | 1.1±1.5 | .72 | |||
| Percentage productivity loss due to absence | 10.6±15.8 | 10.4±17.0 | 10.8±14.6 | .88 |
Abbreviations: IQR = interquartile range; PHQ-9 = Patient Health Questionnaire; WLQ = Work Limitations Questionnaire.
Symptom severity score was assessed using the PHQ-9. Possible scores on the PHQ-9 range from 0 to 27. Higher scores indicate more severe depressive symptoms.
Based on a chronic condition checklist including up to 12 conditions.
Nurse, psychologist, social worker and/or mental health counselor.
Based on responses to the Work Limitations Questionnaire (WLQ). Scale scores indicate the percent of time limited in the past two weeks in ability to perform job tasks (e.g., time management). Possible scale scores range from 0 to 100, with higher scores indicating greater percentage of time limited in the past two weeks in ability to perform job tasks. Possible productivity loss scores range from 0 to 27, with higher scores indicating greater productivity loss.
Based on responses to the WLQ Time Loss Module. Productivity loss is the mean percentage of hours missed in the past two weeks divided by the total number of hours usually worked in that time period. Possible days missed range from 0 to 14. Possible percent productivity loss due to absenteeism ranges from 0 to 100, with higher scores indicating greater productivity loss.
In the sample, the mean age was 54.6 years old (SD = 6.0), 73.7% (N = 123) were female, 87.3% (N = 145) were White, non-Hispanic, 72.4% (N = 121) earned a bachelor’s degree or higher, and median annual earnings was $60,000 (IQR = 38,472). A majority (88.6%; N = 148) worked full-time and 73.7% had white collar occupations (N = 123). The mean number of hours worked per week was 42.6 (SD = 10.8). More than half (58.1%, N = 97) had their jobs for five years or more, 25.7% (N = 43) had union positions, and 4.8% (N = 8) were self-employed. (Table 1)
The average baseline PHQ-9 depression symptom severity was mild at 9.5 (SD = 2.6), nonetheless 82% (N = 137) reported a history of antidepressant medication use and 60.5% (N = 101) had a prescribed antidepressant at baseline. In the four months prior to baseline, 26.5% had seen a primary care physician, 29.9% visited a psychiatrist or psychiatric nurse specialist, and 26.9% visited another mental health counselor for an emotional problem; (Table 1).
Both the WFI and UC groups had similar levels of baseline at-work performance and work absences, as measured by the four WLQ scale scores (0.31 ≤ P ≤ .63), PL scores (P = .69), work absences (P = .72), and APL (P = .88). The mean amount of time that participants were limited in their ability to perform work tasks was: 34.3% of the time (SD = 18.4) for time management; 17.9% (SD = 17.3) for physical tasks; 30.8% (SD = 13.4) for mental-interpersonal tasks; and 34.8% (SD = 20.3) for output tasks. Mean PL was 8.5% (SD = 3.6). Also during this period, participants missed a mean 1.1 workdays (SD = 1.7). Mean APL was 10.6% (SD = 15.8); (Table 1).
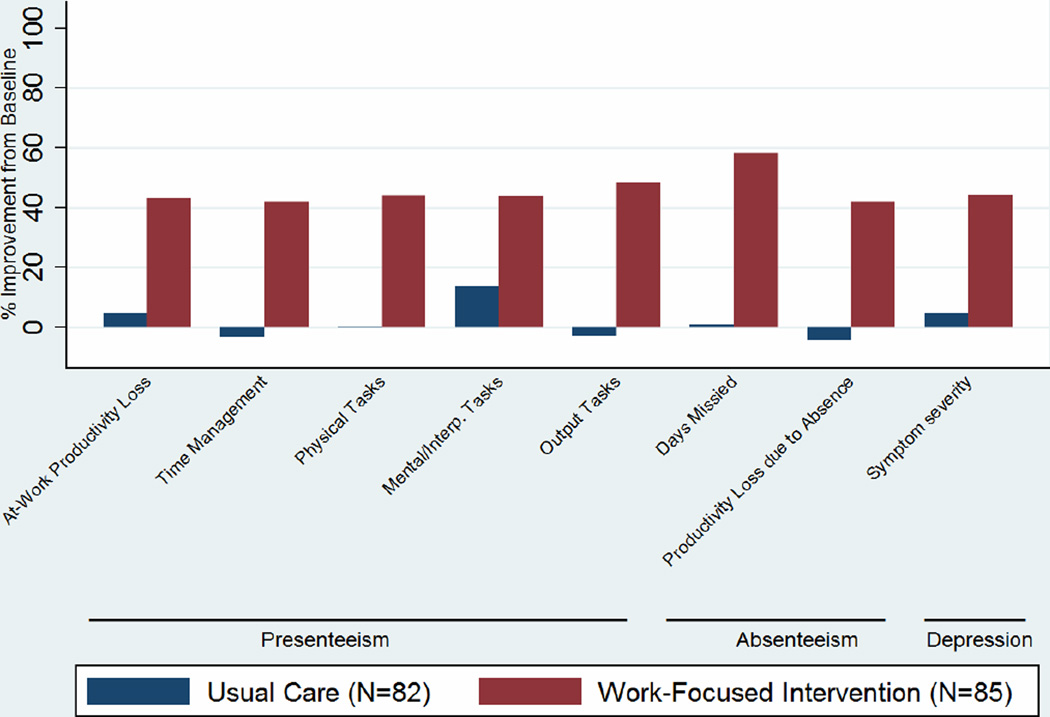
By the four-month follow-up, based on mixed effects models, between-group testing demonstrated significant improvements in the WFI group vs. UC group (which showed no improvement) on three of the four WLQ scales as well as the PL score. Differences were not statistically significant for the WLQ physical tasks scale (difference in change: P = .17); self-reported absences (difference in change: P = .09); and APL (difference in change: P = .16). Additionally, the WFI group improved significantly on all four within-group outcomes tested (P < .01 for all outcomes) whereas the UC group only improved significantly on the mental-interpersonal tasks scale (P = .02); (Table 2, Figure 2, percent improvement from baseline).
Table 2.
Dysthymia Presenteeism, Absenteeism and Depression Symptom Severity Outcomes: Mixed Effects Modelsa
| Experimental Intervention | Usual Care | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-Up | Change | Baseline | Follow-Up | Change | ||||||||||
| n=85 | n=78 | n=82 | n=72 | Difference in Change Scores | |||||||||||
| Mean | SD | Mean | SD | Mean | Effect Sizee |
Mean | SD | Mean | SD | Mean | Effect Sizee |
Change (95% CI) |
Effect Sizee |
P | |
| Presenteeismb | |||||||||||||||
| Percent at-work productivity loss (0–27) | 8.6 | 3.4 | 4.9 | 3.7 | −3.7 | −1.09 | 8.4 | 3.8 | 8.0 | 4.0 | −0.4 | −0.11 |
−3.3 (−4.6, −2.0) |
−0.91 | <.001 |
| Percent time with at-work limitations by task | |||||||||||||||
| Time management (0– 100) | 35.0 | 17.9 | 20.3 | 18.5 | −14.8 | −0.83 | 33.5 | 19.1 | 34.6 | 19.9 | 1.1 | 0.06 |
−15.2 (−21.7, −8.7) |
−0.68 | <.001 |
| Physical tasks (0–100) | 18.9 | 17.6 | 10.5 | 17.9 | −8.3 | −0.47 | 16.8 | 16.9 | 16.8 | 16.5 | 0.0 | 0.00 | −4.3 (−10.4, 1.8) |
−0.29 | .17 |
| Mental-Interpersonal tasks (0–100) | 30.3 | 13.1 | 17.0 | 12.7 | −13.3 | −1.02 | 31.4 | 13.8 | 27.1 | 14.6 | −4.3 | −0.31 |
−11.2 (−15.7, −6.6) |
−0.83 | <.001 |
| Output tasks (0–100) | 36.4 | 19.8 | 18.8 | 19.1 | −17.6 | −0.89 | 33.1 | 20.7 | 34.1 | 21.9 | 1.0 | 0.05 |
−17.5 (−24.4, − 10.5) |
−0.86 | <.001 |
| Absences Due to Health or Medical Carec | |||||||||||||||
| Days missed (0–80) | 1.2 | 2.0 | 0.5 | 0.9 | −0.7 | −0.35 | 1.1 | 1.5 | 1.1 | 2.1 | −0.0 | −0.00 | −0.5 (−1.1, 0.1) |
−0.31 | .09 |
| Percent productivity loss due to absence (0–100) | 10.4 | 17.0 | 6.0 | 15.6 | −4.4 | −0.26 | 10.8 | 14.6 | 11.3 | 21.6 | 0.5 | 0.03 | −4.0 (−9.7, 1.6) |
−0.23 | .16 |
| Depressiond | |||||||||||||||
| Symptom severity (0–27) | 9.5 | 2.7 | 5.3 | 3.9 | −4.2 | −1.56 | 9.4 | 2.5 | 8.9 | 4.4 | −0.5 | −0.20 |
−3.8 (−5.0, −2.6) |
−0.89 | <.001 |
| Sensitivity Analysis (LOCF) | |||||||||||||||
| Percent at-work productivity loss (0–27) | 8.6 | 3.4 | 5.4 | 4.1 | −3.2 | −0.94 | 8.4 | 3.8 | 8.1 | 4.0 | −0.3 | −0.08 |
−3.0 (−4.0, −2.0) |
−0.88 | <.001 |
| Depression symptom severity (0–27) | 9.5 | 2.7 | 5.8 | 4.2 | −3.7 | −1.37 | 9.4 | 2.5 | 9.2 | 4.2 | −0.2 | −0.08 |
−3.4 (−4.7, −2.2) |
−0.83 | <.001 |
Models are adjusted for recruitment site, participant mean age, percent male, percent White, percent married, percent white collar occupation, mean number of co-morbidities, percent full time employed at baseline, and baseline mean scores of model dependent variable.
Based on responses to the Work Limitations Questionnaire (WLQ). Scale scores indicate the percent of time limited in the past two weeks in ability to perform job tasks (e.g., time management). Possible scale scores range from 0 to 100, with higher scores indicating greater percentage of time limited in the past two weeks in ability to perform job tasks. Possible productivity loss scores range from 0 to 27, with higher scores indicating greater productivity loss.
Based on responses to the WLQ Time Loss Module. Productivity loss is the mean percentage of hours missed in the past two weeks divided by the total number of hours usually worked in that time period. Possible days missed range from 0 to 14. Possible percent productivity loss due to absenteeism ranges from 0 to 100, with higher scores indicating greater productivity loss.
Symptom severity score was assessed using the PHQ-9. Possible scores on the PHQ-9 range from 0 to 27. Higher scores indicate more severe depressive symptoms.
Effect size was computed as the ratio of the difference of change score and the pooled standard deviation of baseline scores for both groups.
Figure 2.
Percentage Change in Presenteeism, Absenteeism and Depression Symptom Severity: Pre-Intervention to Post-Interventiona,b
a Models are adjusted for study site, baseline mean age, percent male, percent White, percent married, percent white collar occupation, mean number of comorbidities, percent full-time employed, and mean scores of model dependent variable.
b The differences in the percent improvement from baseline between the Work-Focused Intervention and Usual Care were all significant at the p<0.001 level, except for the Productivity Loss Due to Absence, which was significant at the p<0.01 level.
The WFI resulted in large and significant improvements in presenteeism. PL score improved 43.0% (P < 0.001) in the WFI group compared to 4.8% in UC (P = .41); (difference in change: P < 0.001). Although the between-group test for the physical tasks scale was not significant, between-group tests were significant in favor of the WFI vs. UC for the other three performance scales (difference in change: P < 0.001). Within the WFI group, scale scores improved 42.3% to 48.4% (P < 0.001 for all scales). Within the UC group, scale scores had 0% change to 3.3% non-significant worsening on time management, physical, and output tasks (P > .05) but a 13.7% significant improvement on mental-interpersonal tasks (P = .02); (Table 2, Figure 2). All of the significant improvements in the WFI group represented moderate to large effects.
Although work absences declined by 58.3% in WFI (P < 0.001) vs. 0% change in UC (P = .97), there was no significant difference between the groups. Similarly, even though APL improved in WFI group by 42.3% (P = .01) vs. 4.6% worsening in the UC group (P = .85), the difference did not reach statistical significance; (Table 2).
At follow-up, PHQ-9 depression severity scores also significantly declined within the WFI group but not within the UC group. Mean depression symptom severity scores fell 44.2% (P < 0.001) for WFI vs. 5.3% (P = .39) for UC, which resulted in a significant difference between the groups (difference in change: P < 0.001); (Table 2, Figure 2).
Sensitivity analyses of at-work productivity loss and depression symptom severity results supported the findings. LOCF models, comparing the difference in outcome change between the groups, yielded slightly smaller, significant effect sizes. For PL the effect size changed from −.91 in the original model to −.88 for the LOCF model. For PHQ-9 depression symptom severity, the parallel change in effect size was −0.89 to −0.83 (data not shown).
Further analyses of the sample were conducted using PHQ-9 severity score cut-points of <=9 (N=82) to assess the impact of the WFI on depressive symptom levels below those of participants with MDD in the larger sample (95% of the depressed sample from the larger study had a PHQ=>13) as well as using the PHQ-9 >=10 (N=85). This yielded slightly larger significant effect sizes with the between group comparisons and essentially identical results (data not shown).
4. Discussion
Chronic depressive symptoms have a negative impacted on ability to function in important social roles and activities, including employment [1, 3, 5, 6, 8, 17, 20]. This study identified a new telephone-based intervention for achieving functional recovery (including at-work performance, at-work productivity loss, and depression severity) in individuals screened for dysthymia. For this subgroup analysis, dysthymia was defined as chronic depressive symptoms lasting two or more years and not meeting current symptom criteria for MDD. With a PHQ-9 symptom severity of 9.5 (in the mild range) the impact on work functioning at baseline was substantial (mean baseline at work productivity loss=8.5% and absences=10.6%). For employers who are aware of the impact of depression on their employees work functioning [33, 35] this intervention provides a new tool for improving mental health and work outcomes.
The original power analysis was based on the ability to detect differences between the WFI and UC groups for the overall sample, rather than for subgroups [39]. Nevertheless, the outcomes obtained in this study, showing moderate to large effect sizes, are both statistically significant and clinically meaningful. By the four-month follow-up, the WFI was significantly more effective than UC on five out of the eight between-group work outcomes, with the exception of the WLQ physical tasks scale, self-reported absences and productivity loss due to absences (APL). These between group differences are a result of significant gains within the WFI group and lack of change in the UC group unrelated to power. Despite an absolute difference of 4.3 between WFI and UC in mean WLQ physical tasks, 0.5 days in absences and 4.0 in APL, the differences were not statistically significant due to the large standard deviation of the measure. Furthermore, the WFI improved significantly on all within-group outcomes whereas UC only improved on the WLQ mental-interpersonal tasks scale. In addition, depression severity, as measured by the PHQ-9, also declined in the intervention group by 44% (from 9.5 to 5.3) while not at all in the UC group.
Study strengths include a randomized design with rigorous recruitment and follow-up methods, widely used validated measurement tools, a monitored protocoldriven intervention with careful documentation, participation of multiple employer groups and a conceptual model for the WFI program. The present study meets recommended criteria for using subgroup analysis (though it was not specified a prior in the trial registration) [58], and the subgroup effects consistent across two studies are unlikely to be due to chance alone. Study limitations include a brief, single follow-up period, the sample size, the lack of administrative work data (e.g., objectively measured productivity and disability claims), the absence of a diagnosis based on clinical interview (or data about occurrences of major depressive disorder within the first two years of a dysthymia diagnosis). Screening using the PC-SAD rather than a structured diagnostic interview yielded a sample with probable dysthymia; nonetheless this sample with persistent subthreshold depressive symptoms responded significantly to the intervention. For some endpoints with large standard deviations there was not adequate power. To minimize response bias all evaluations were completed on line rather than by in person interview; however it is possible that study participants who received the WFI were positively biased in their reporting. They were neither blinded to the intervention and the UC group received no direct contact from a study provider. Additionally, the WFI did not address organizational-level changes, which may contribute to a psychologically-healthy workplace [59].
Work limitations are both a sign and outcome of depressive disorders including dysthymia. The severity and chronicity of depressive symptoms in individuals with dysthymia is well known [2, 3, 5, 6, 8–10, 16, 17, 20, 21, 23–27, 32]. The extent of work difficulty associated with depressive symptoms observed in this study reminds us of the importance of recognizing and addressing the impact of such a persistent condition on the lives of working individuals. This new intervention holds promise for helping this group of employees, whose milder symptoms are sometimes overlooked and whose work problems may not be widely recognized. Accessible and adequate treatment by the health care system is an essential first step in this process. The challenge remains to develop practical interventions for employees with chronic health issues in general, and those with chronic depressive symptoms in particular, to help them manage their work limitations and sustain their productivity.
5. Conclusions
The WFI offers a potential contribution to the collaborative care model seeking to help employed individuals by providing comprehensive, patient-centered care. In addition to advancing employment outcomes and functional improvement research, the study results further support the role for technology-enabled methods for providing effective treatment care that may be accessed from any computer or telephone [60, 61]. In the future, employees may be able to access it through physician referral, the workplace, or independently. While up to now the picture for helping individuals with chronic depressive symptoms has been bleak, we have taken a first step to help them better manage their work limitations.
Dysthymia Highlights.
Dysthymia is a chronic condition associated with a range of functional limitations.
We developed a novel multi-component work focused intervention (WFI) program.
WFI is superior to Usual Care (UC) for reducing depression symptom severity.
In an RCT we found the WFI is superior to UC for reducing work productivity loss.
The WFI is a functional improvement resource for the employed dysthymic population.
Acknowledgments
This study was supported by a grant from the National Institute on Aging (NIA) (R01AG033125; No. NCT01163890 http://clinicaltrials.gov/ct2/show/NCT01163890). Drs. Lerner, Adler and Rogers contributed to obtaining funding for the research and its study design, conception of the intervention, design and implementation of site recruitment and data acquisition, analysis and interpretation. Drs. Lerner and Adler were responsible for training and supervising the counselors and collecting, analyzing and interpreting counselor data. Dr. Rogers and Ms. Greenhill designed and implemented the study website and information system. Dr. Chang and Ms. Greenhill were responsible for monitoring data collection, managing the databases and performing statistical analyses. Dr. Azocar who as lead investigator for Optum, Inc. was responsible for designing and implementing site recruitment. Dr. Adler and Mr. Visco were responsible for the literature review. Dr. Cymerman was involved in training and supervising the counselors. All co-authors were involved in drafting and revising the manuscript. We wish to acknowledge Evette J. Ludman, PhD for her contributions to the CBT strategies training and Ms. Doris Hernandez for her assistance in preparing this manuscript. We dedicate this manuscript in memorium to our dear colleague Wayne Katon, the father of Collaborative Care and a longtime supporter of our shared mission of improving the functional outcomes of patients.
Drs. Lerner, Adler and Rogers had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. The study results have not been published previously in print or electronic format nor submitted for publication elsewhere.
Drs. Lerner and Rogers co-developed the Work Limitations Questionnaire (WLQ), which is used in this study. Dr. Rogers and Adler co-developed the PC-SAD, which is used in this study. Neither individual receives royalties directly from the licensure of either survey instrument.
The NIA had no role in the design and conduct of the study, in the collection, analysis, and interpretation of the data, and in the preparation, review, or approval of the manuscript, or in the decision to submit the manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
There are no other conflicts of interest to report.
Contributor Information
David A. Adler, Email: dadler@tuftsmedicalcenter.org.
Debra Lerner, Email: dlerner@tuftsmedicalcenter.org.
Zachary L. Visco, Email: zvisco@tuftsmedicalcenter.org.
Annabel Greenhill, Email: agreenhill@tuftsmedicalcenter.org.
Hong Chang, Email: hchang@tuftsmedicalcenter.org.
Elina Cymerman, Email: ecymerman@tuftsmedicalcenter.org.
Francisca Azocar, Email: francisca.azocar@optum.com.
William H. Rogers, Email: whrogers@tuftsmedicalcenter.org.
Reference List
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Publishing; [Google Scholar]
- 2.Angst J, Sellaro R, Merikangas KR. Depressive spectrum diagnoses. Compr Psychiatry. 2000;41:39–47. doi: 10.1016/s0010-440x(00)80007-3. [DOI] [PubMed] [Google Scholar]
- 3.Blanco C, Okuda M, Markowitz JC, Liu SM, Grant BF, Hasin DS. The epidemiology of chronic major depressive disorder and dysthymic disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2010;71:1645–1656. doi: 10.4088/JCP.09m05663gry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Keller MB, Klein DN, Hirschfeld RM, Kocsis JH, McCullough JP, Miller I, et al. Results of the DSM-IV mood disorders field trial. Am J Psychiatry. 1995;152:843–849. doi: 10.1176/ajp.152.6.843. [DOI] [PubMed] [Google Scholar]
- 5.Klein DN, Santiago NJ. Dysthymia and chronic depression: introduction, classification, risk factors, and course. J Clin Psychol. 2003;59:807–816. doi: 10.1002/jclp.10174. [DOI] [PubMed] [Google Scholar]
- 6.Klein DN, Schwartz JE, Rose S, Leader JB. Five-year course and outcome of dysthymic disorder: A prospective, naturalistic follow-up study. Am J Psychiatry. 2000;157:931–939. doi: 10.1176/appi.ajp.157.6.931. [DOI] [PubMed] [Google Scholar]
- 7.Ravindran AV, Anisman H, Merali Z, Charbonneau Y, Telner J, Bialik RJ, et al. Treatment of primary dysthymia with group cognitive therapy and pharmacotherapy: clinical symptoms and functional impairments. Am J Psychiatry. 1999;156:1608–1617. doi: 10.1176/ajp.156.10.1608. [DOI] [PubMed] [Google Scholar]
- 8.Klein DN, Shankman SA, Rose S. Ten-year prospective follow-up study of the naturalistic course of dysthymic disorder and double depression. Am J Psychiatry. 2006;163:872–880. doi: 10.1176/ajp.2006.163.5.872. [DOI] [PubMed] [Google Scholar]
- 9.Steiner M, Bell B, Browne G, Roberts J, Gafni A, Byrne C, et al. Prevalence of dysthymic disorder in primary care. J Affect Disord. 1999;54:303–308. doi: 10.1016/s0165-0327(98)00189-x. [DOI] [PubMed] [Google Scholar]
- 10.Berndt ER, Finkelstein SN, Greenberg PE, Howland RH, Keith A, Rush AJ, et al. Workplace performance effects from chronic depression and its treatment. J Health Econ. 1998;17:511–535. doi: 10.1016/s0167-6296(97)00043-x. [DOI] [PubMed] [Google Scholar]
- 11.Goetzel RZ, Hawkins K, Ozminkowski RJ, Wang S. The health and productivity cost burden of the "top 10" physical and mental health conditions affecting six large U.S. employers in 1999. J Occup Environ Med. 2003;45:5–14. doi: 10.1097/00043764-200301000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Lerner D, Amick BC, III, Lee JC, Rooney T, Rogers WH, Chang H, et al. Relationship of employee-reported work limitations to work productivity. Med Care. 2003;41:649–659. doi: 10.1097/01.MLR.0000062551.76504.A9. [DOI] [PubMed] [Google Scholar]
- 13.Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 14.Stewart WF, Ricci JA, Chee E, Hahn SR, Morganstein D. Cost of lost productive work time among US workers with depression. JAMA. 2003;289:3135–3144. doi: 10.1001/jama.289.23.3135. [DOI] [PubMed] [Google Scholar]
- 15.Wang PS, Patrick A, Avorn J, Azocar F, Ludman E, McCulloch J, et al. The costs and benefits of enhanced depression care to employers. Arch Gen Psychiatry. 2006;63:1345–1353. doi: 10.1001/archpsyc.63.12.1345. [DOI] [PubMed] [Google Scholar]
- 16.Hellerstein DJ. Dysthymic Disorder: Integrating Research Findings into Clinical Treatment. Journal of Psychiatric Practice. 2001;7:298–309. doi: 10.1097/00131746-200109000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Keller MB. Dysthymia in clinical practice:course, outcome and impact on the community. Acta Psychiatr Scand Suppl. 1994;383 doi: 10.1111/j.1600-0447.1994.tb05880.x. 24-34:24-34. [DOI] [PubMed] [Google Scholar]
- 18.Adler DA, McLaughlin TJ, Rogers WH, Chang H, Lapitsky L, Lerner D. Job performance deficits due to depression. Am J Psychiatry. 2006;163:1569–1576. doi: 10.1176/appi.ajp.163.9.1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Broadhead WE, Blazer DG, George LK, Tse CK. Depression, disability days, and days lost from work in a prospective epidemiologic survey. JAMA. 1990;264:2524–2528. [PubMed] [Google Scholar]
- 20.Adler DA, Irish J, McLaughlin TJ, Perissinotto C, Chang H, Hood M, et al. The work impact of dysthymia in a primary care population. Gen Hosp Psychiatry. 2004;26:269–276. doi: 10.1016/j.genhosppsych.2004.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beck A, Crain AL, Solberg LI, Unutzer J, Glasgow RE, Maciosek MV, et al. Severity of depression and magnitude of productivity loss. Ann Fam Med. 2011;9:305–311. doi: 10.1370/afm.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Katon W. The impact of depression on workplace functioning and disability costs. Am J Manag Care. 2009;15:S322–S327. [PubMed] [Google Scholar]
- 23.Martin JK, Blum TC, Beach SR, Roman PM. Subclinical depression and performance at work. Soc Psychiatry Psychiatr Epidemiol. 1996;31:3–9. doi: 10.1007/BF00789116. [DOI] [PubMed] [Google Scholar]
- 24.Shelton RC, Davidson J, Yonkers KA, Koran L, Thase ME, Pearlstein T, et al. The undertreatment of dysthymia. J Clin Psychiatry. 1997;58:59–65. doi: 10.4088/jcp.v58n0202. [DOI] [PubMed] [Google Scholar]
- 25.Thase ME, Fava M, Halbreich U, Kocsis JH, Koran L, Davidson J, et al. A placebocontrolled, randomized clinical trial comparing Sertraline and Imipramine for the treatment of dysthymia. Arch Gen Psychiatry. 1996;53:777–784. doi: 10.1001/archpsyc.1996.01830090023004. [DOI] [PubMed] [Google Scholar]
- 26.Levkovitz Y, Tedeschini E, Papakostas GI. Efficacy of antidepressants for dysthymia: a meta-analysis of placebo-controlled randomized trials. J Clin Psychiatry. 2011;72:509–514. doi: 10.4088/JCP.09m05949blu. [DOI] [PubMed] [Google Scholar]
- 27.Fournier JC, Derubeis RJ, Hollon SD, Dimidjian S, Amsterdam JD, Shelton RC, et al. Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA. 2010;303:47–53. doi: 10.1001/jama.2009.1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Browne G, Steiner M, Roberts J, Gafni A, Byrne C, Dunn E, et al. Sertraline and/or interpersonal psychotherapy for patients with dysthymic disorder in primary care: 6-month comparison with longitudinal 2-year follow-up of effectiveness and costs. J Affect Disord. 2002;68:317–330. doi: 10.1016/s0165-0327(01)00343-3. [DOI] [PubMed] [Google Scholar]
- 29.de Mello MF, Myczcowisk LM, Menezes PR. A randomized controlled trial comparing moclobemide and moclobemide plus interpersonal psychotherapy in the treatment of dysthymic disorder. J Psychother Pract Res. 2001;10:117–123. [PMC free article] [PubMed] [Google Scholar]
- 30.Markowitz JC, Kocsis JH, Bleiberg KL, Christos PJ, Sacks M. A comparative trial of psychotherapy and pharmacotherapy for "pure" dysthymic patients. J Affect Disord. 2005;89:167–175. doi: 10.1016/j.jad.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 31.von WA, Holzel LP, Westphal A, Harter M, Kriston L. Selective serotonin reuptake inhibitors and tricyclic antidepressants in the acute treatment of chronic depression and dysthymia: a systematic review and meta-analysis. J Affect Disord. 2013;144:7–15. doi: 10.1016/j.jad.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 32.Spek V, Nyklicek I, Smits N, Cuijpers P, Riper H, Keyzer J, et al. Internet-based cognitive behavioural therapy for subthreshold depression in people over 50 years old: a randomized controlled clinical trial. Psychol Med. 2007;37:1797–1806. doi: 10.1017/S0033291707000542. [DOI] [PubMed] [Google Scholar]
- 33.Wang PS, Simon GE, Avorn J, Azocar F, Ludman EJ, McCulloch J, et al. Telephone screening, outreach, and care management for depressed workers and impact on clinical and work productivity outcomes: a randomized controlled trial. JAMA. 2007;298:1401–1411. doi: 10.1001/jama.298.12.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McKnight PE, Kashdan TB. The importance of functional impairment to mental health outcomes: a case for reassessing our goals in depression treatment research. Clin Psychol Rev. 2009;29:243–259. doi: 10.1016/j.cpr.2009.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Trivedi MH, Morris DW, Wisniewski SR, Lesser I, Nierenberg AA, Daly E, et al. Increase in work productivity of depressed individuals with improvement in depressive symptom severity. Am J Psychiatry. 2013;170:633–641. doi: 10.1176/appi.ajp.2012.12020250. [DOI] [PubMed] [Google Scholar]
- 36.Costa-Black KM, Loisel P, Anema JR, Pransky G. Back pain and work. Best Pract Res Clin Rheumatol. 2010;24:227–240. doi: 10.1016/j.berh.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 37.Drake RE, Frey W, Bond GR, Goldman HH, Salkever D, Miller A, et al. Assisting social security disability insurance beneficiaries with schizophrenia, bipolar disorder, or major depression in returning to work. Am J Psychiatry. 2013;170:1433–1441. doi: 10.1176/appi.ajp.2013.13020214. [DOI] [PubMed] [Google Scholar]
- 38.Lerner D, Adler D, Hermann RC, Chang H, Ludman EJ, Greenhill A, et al. Impact of a work-focused intervention on the productivity and symptoms of employees with depression. J Occup Environ Med. 2012;54:128–135. doi: 10.1097/JOM.0b013e31824409d8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lerner D, Adler DA, Rogers WH, Chang H, Greenhill A, Cymerman E, et al. A multi-site randomized clinical trial of a telephone-based intervention to reduce presenteeism and absenteeism among employees with depression. Psychiatr Serv. 2014 doi: 10.1176/appi.ps.201400350. [In Press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Baltes P, Baltes M. Successful aging: Perspectives from the Behavioral Sciences. New York: Cambridge University Press; 1990. [Google Scholar]
- 41.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rogers WH, Wilson IB, Bungay KM, Cynn DJ, Adler DA. Assessing the performance of a new depression screener for primary care (PC-SAD(c)) J Clin Epidemiol. 2002;55:164–175. doi: 10.1016/s0895-4356(01)00430-9. [DOI] [PubMed] [Google Scholar]
- 43.Lerner D, Amick BC, Rogers WH, Malspeis S, Bungay K, Cynn D. The Work Limitations Questionnaire. Med Care. 2001;39:72–85. doi: 10.1097/00005650-200101000-00009. [DOI] [PubMed] [Google Scholar]
- 44.Lerner D, Reed JI, Massarotti E, Wester LM, Burke TA. The Work Limitations Questionnaire's validity and reliability among patients with osteoarthritis. J Clin Epidemiol. 2002;55:197–208. doi: 10.1016/s0895-4356(01)00424-3. [DOI] [PubMed] [Google Scholar]
- 45.Lerner D, Adler DA, Rogers WH, Chang H, Lapitsky L, McLaughlin T, et al. Work performance of employees with depression: the impact of work stressors. Am J Health Promot. 2010;24:205–213. doi: 10.4278/ajhp.090313-QUAN-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bush B, Shaw S, Cleary P, Delbanco TL, Aronson MD. Screening for alcohol abuse using the CAGE questionnaire. Am J Med. 1987;82:231–235. doi: 10.1016/0002-9343(87)90061-1. [DOI] [PubMed] [Google Scholar]
- 47.Ware JE, Jr., Kosinski M, Keller SD. SF-12: How to Score the SF-12 Physical & Mental Health Summary Scales. 2nd ed. Boston MA: The Health Institute, New England Medical Center; 1995. [Google Scholar]
- 48.Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- 49.Katon W, Von Korff M, Lin E, Walker E, Simon GE, Bush T, et al. Collaborative management to achieve treatment guidelines. Impact on depression in primary care. J Am Med Assoc. 1995;273:1026–1031. [PubMed] [Google Scholar]
- 50.Beck AT. Cognitive Therapy and the Emotional Disorders. New York: International University Press; 1979. [Google Scholar]
- 51.Lewinsohn P, Antonuccio D, Steinmetz J, Teri L. The coping with depression course: a psychoeducational intervention for unipolar depression. Eugene, OR: Castalia Press; 1984. [Google Scholar]
- 52.Simon LE, Ludman E, Tutty S. Creating a Balance: A Step-by-step approach to managing stress and lifting your mood. Victoria BC: Trafford Press; 2006. [Google Scholar]
- 53.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 54.Lane P. Handling drop-out in longitudinal clinical trials: a comparison of the LOCF and MMRM approaches. Pharm Stat. 2008;7:93–106. doi: 10.1002/pst.267. [DOI] [PubMed] [Google Scholar]
- 55.Siddiqui O, Ali MW. A comparison of the random-effects pattern mixture model with last-observation-carried-forward (LOCF) analysis in longitudinal clinical trials with dropouts. J Biopharm Stat. 1998;8:545–563. doi: 10.1080/10543409808835259. [DOI] [PubMed] [Google Scholar]
- 56.Cohen J. A power primer. Psychol Bull. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 57.StataCorp. Stata Reference Manual Release 9. 9th ed. College Station, TX: Stata Press; 2005. [Google Scholar]
- 58.Sun X, Ioannidis JP, Agoritsas T, Alba AC, Guyatt G. How to use a subgroup analysis: users' guide to the medical literature. JAMA. 2014;311:405–411. doi: 10.1001/jama.2013.285063. [DOI] [PubMed] [Google Scholar]
- 59.Black DC. [Accessed July 22, 2014];Working for a healthier tomorrow. 2008 Available at: https://www govuk/government/uploads/system/uploads/attachment_data/file/209782/hwwb-working-for-a-healthier-tomorrow pdf.
- 60.Andersson G, Cuijpers P. Internet-based and other computerized psychological treatments for adult depression: a meta-analysis. Cogn Behav Ther. 2009;38:196–205. doi: 10.1080/16506070903318960. [DOI] [PubMed] [Google Scholar]
- 61.Mohr DC, Ho J, Duffecy J, Reifler D, Sokol L, Burns MN, et al. Effect of telephone-administered vs face-to-face cognitive behavioral therapy on adherence to therapy and depression outcomes among primary care patients: a randomized trial. JAMA. 2012;307:2278–2285. doi: 10.1001/jama.2012.5588. [DOI] [PMC free article] [PubMed] [Google Scholar]