Abstract
PURPOSE
We aimed to assess reliability of the evaluation of osteophytes and subchondral cysts on tomosynthesis images when read by radiologists with different levels of expertise.
MATERIALS AND METHODS
Forty subjects aged >40 years had both knees evaluated using tomosynthesis. Images were read by an “experienced” reader (musculoskeletal radiologist with prior experience) and an “inexperienced” reader (radiology resident with no prior experience). Readers graded osteophytes from 0 to 3 and noted the presence/absence of subchondral cysts in four locations of the tibiofemoral joint. Twenty knees were randomly selected and re-read. Inter- and intrareader reliabilities were calculated using overall exact percent agreement and weighted κ statistics. Diagnostic performance of the two readers was compared against magnetic resonance imaging readings by an expert reader (professor of musculoskeletal radiology).
RESULTS
The experienced reader showed substantial intrareader reliability for graded reading of osteophytes (90%, κ=0.93), osteophyte detection (95%, κ=0.86) and cyst detection (95%, κ=0.83). The inexperienced reader showed perfect intrareader reliability for cyst detection (100%, κ=1.00) but intrareader reliability for graded reading (75%, κ=0.79) and detection (80%, κ=0.61) of osteophytes was lower than the experienced reader. Inter-reader reliability was 61% (κ=0.72) for graded osteophyte reading, 91% (κ=0.82) for osteophyte detection, and 88% (κ=0.66) for cyst detection. Diagnostic performance of the experienced reader was higher than the inexperienced reader regarding osteophyte detection (sensitivity range 0.74–0.95 vs. 0.54–0.75 for all locations) but diagnostic performance was similar for subchondral cysts.
CONCLUSION
Tomosynthesis offers excellent intrareader reliability regardless of the reader experience, but experience is important for detection of osteophytes.
Tomosynthesis is a digital X-ray imaging technique that allows acquisition of tomographic information (1). In the literature, its use has been reported for imaging of lungs (1–4), breast (5–7), and head and neck region (8–10); for visualization of kidneys through intravenous pyelogram (11); for localization of an endorectal balloon for prostate image-guided radiation therapy (12); and for evaluation of aortic arch calcification (13), and bone and joint pathologies (14–21). While its clinical use has become common in chest and breast imaging, its clinical application in arthritis imaging is scarcely documented in the literature (14, 15, 22).
In a recent study, we reported that tomosynthesis had higher sensitivity for detection of osteophytes and subchondral cysts compared to conventional radiography, using magnetic resonance imaging (MRI) findings as the reference standard (15). In that study, the readings were performed by a single expert musculoskeletal radiologist, and the intrareader reliability for this reader was reported as excellent (weighted κ=1.00 for osteophytes and 0.86 for subchondral cysts). Although it is known that reader experience is important for high reliability in radiographic assessment of knee osteoarthritis (23), it is not known whether excellent reliability can be achieved when tomosynthesis images are read by radiologists with different levels of experience.
Tomosynthesis is a potentially useful tool in osteoarthritis research and might be used more frequently in the future because of its advantages over radiography. For its use to become more widespread, however, we need to understand whether reader experience affects the reliability of scoring osteoarthritis features on tomosynthesis, as it does with conventional radiography. It is possible that tomosynthesis can provide high reliability even with inexperienced readers because of the tomographic nature of the acquired images.
The aim of this study was to determine the intrareader and inter-reader reliability for semiquantitative scoring of osteophytes and subchondral cyst detection using tomosynthesis, when read by radiologists with different levels of experience.
Materials and methods
Recruitment of study participants
Forty subjects over the age of 40 were recruited for this study. They were all patients, with or without knee pain or knee osteoarthritis, at the rheumatology outpatient clinic at our institution between July 2009 and November 2009. Demographic information included height, weight, age, gender, and race. Exclusion criteria were a history of rheumatoid arthritis, gout, systemic lupus erythematosus, Paget disease, other inflammatory knee disorders, or major knee trauma and/or surgery, or any contra-indication for MRI including the use of cardiac pacemaker and claustrophobia. Written informed consent was obtained from all participants. The local institutional review board approved the study protocol.
Conceptualization of the present study took place after the completion and publication of our previously published study (15). While that study analyzed the diagnostic performance of tomosynthesis compared to MRI as the reference, reader experience and reliability of readings was not in the focus and would have been far beyond the scope of the manuscript. As tomosynthesis might potentially offer advantages over radiography, such as improved reliability due to superior visualization of osteoarthritis features, it appeared worthwhile designing an additional study. Although the same database was used for the two studies, the aim of the present study is distinctly different from our previous study.
Acquisition of tomosynthesis images
All 40 participants had both knees (total 80 knees) imaged using the VolumeRADTM imaging apparatus (GE Healthcare, Milwaukee, Wisconsin, USA) in a weight-bearing fixed-flexion position with the aid of the SynaFlexerTM positioning frame (CCBR-Synarc, Newark, New Jersey, USA) (24, 25). Thirty-nine reconstructed coronal section tomosynthesis images were acquired with a nominal section thickness of 1 mm without any overlap. All images were acquired at 70 kVp and 1.21 mAs, as described previously (15). The mean total radiation dose per patient was 0.16 mGy. The mean effective dose was estimated to be 0.0076 mSv using the method described by Sabol (26).
Interpretation of tomosynthesis images
The tibiofemoral joint of the knee was subdivided into four locations (Fig. 1): lateral femur, medial femur, lateral tibia, and medial tibia. All images were read by two readers. In each of these locations, marginal osteophytes were semiquantitatively scored according to the Osteoarthritis Research Society International (OARSI) atlas: grade 0, absent; grade 1, small; grade 2, medium; grade 3, large (27). In addition, the graded readings were then dichotomized into either “present” (grade >0) or “absent” (grade 0) to enable calculation of reliability for both graded and dichotomous outcomes. The presence (score 1) or absence (score 0) of subchondral cysts in each location were also noted. Semiquantitative scoring for the cysts was not performed because the OARSI atlas does not include subchondral cysts.
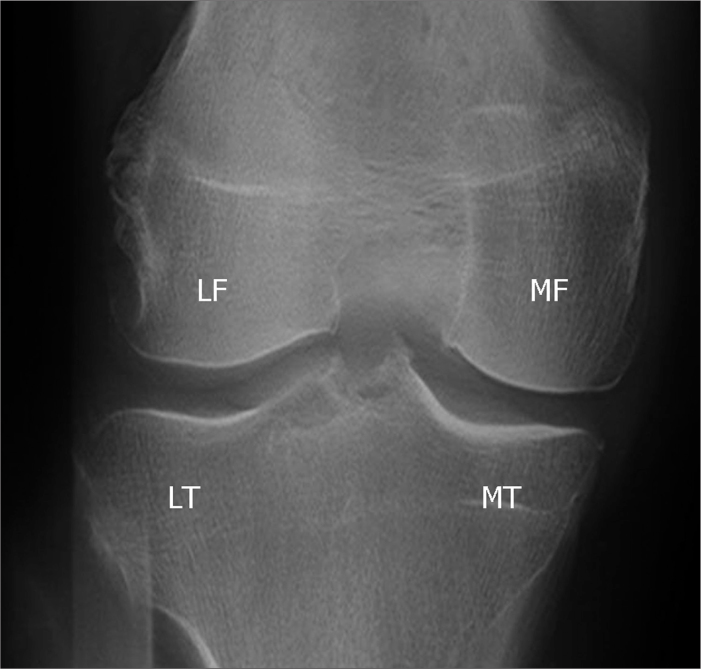
Figure 1.
Tomosynthesis image of a right knee showing the four locations of the tibiofemoral joint: LF, lateral femur; LT, lateral tibia; MF, medial femur; MT, medial tibia.
The first (“experienced”) reader is a board-certified musculoskeletal radiologist (L.X.) with five years of clinical experience as well as one-year research fellowship in musculoskeletal radiology which included training and validation for radiologic semiquantitative scoring of osteoarthritis features using the OARSI atlas (27), and intensive involvement in osteoarthritis research studies as a reader of radiologic images. The second (“inexperienced”) reader was a first-year resident (J.G.) in diagnostic radiology with no prior research or clinical experience in musculoskeletal radiology.
These two readers received training lasting for approximately three hours for interpretation of tomosynthesis images by a professor of musculoskeletal radiology (A.G.), who is an expert at radiologic semiquantitative scoring of osteoarthritis features with 13 years of experience. During the training session, the trainees received guidance by the trainer, on a one-to-one basis, on how to use the OARSI atlas grading scheme for the osteophytes and how to identify subchondral cysts on tomosynthesis images. Trainees then read 10 tomosynthesis images of the knee, graded osteophytes and noted the presence of subchondral cysts with regular reference to the atlas images, and had the opportunity to give their own answers. The trainer reviewed their answers and corrected them as necessary, and provided guidance about possible pitfalls of interpretation. Such training and validation were carried out since both trainees had no prior experience reading tomosynthesis images and it was deemed necessary for the trainees to be able to read the tomosynthesis images in a standardized manner so that the results of their readings can be meaningfully analyzed statistically to assess diagnostic performance/reliability of tomosynthesis. Both the experienced reader and the inexperienced reader completed the first reading of all images within two weeks of completing training. To test intrareader reliability, two readers performed a second reading of 20 randomly selected knees more than a month after the first reading.
To characterize the study participants, the expert reader read all tomosynthesis images using the Kellgren and Lawrence (KL) grading scale. KL grade ≥2 was defined as radiographic knee osteoarthritis (15). All images were read using commercially available digital imaging software (eFilm Work-station, version 3.0.0; Merge Healthcare, Milwaukee, Wisconsin, USA). All readers were allowed to adjust window width and level, and to use the pan and zoom functions.
MRI acquisition and interpretation
Both knees of all subjects were imaged using a 3 Tesla system (Intera; Philips Medical Systems, Andover, Massachusetts, USA). For the purpose of this study, we used the coronal proton density-weighted fat-suppressed sequence with the following parameters: repetition time 9000 ms, echo time 10 ms, one signal acquired, 2.5 mm section thickness, 2.5 mm interval, echo train length of eight, 256×256 matrix, and 140 mm field of view).
The expert reader (A.G.) read MR images and recorded the dichotomous outcome (presence or absence) of marginal osteophytes and subchondral cysts using the coronal images, based on the same anatomical subdivision as the radiographic reading (Fig. 1) to make the readings comparable. Further details have been described previously (15). The expert reader’s MRI readings were used as the reference standard against which to compare the diagnostic performance of the other two readers.
Statistical analysis
Inter- and intrareader reliabilities were assessed by means of the overall exact percentage agreement and weighted kappa (κ), interpreted as: <0, less than chance agreement; 0.01–0.20, slight agreement; 0.21–0.40, fair agreement; 0.41–0.60, moderate agreement; 0.61–0.80, substantial agreement; 0.81–0.99, almost perfect agreement; 1.00, perfect agreement (28). Tomosynthesis readings by the experienced and inexperienced readers were compared against the expert’s MRI reading, which was considered as the reference standard, to assess the diagnostic performance (i.e., sensitivity, specificity, and accuracy) of these two readers. All statistical calculations were performed with SAS software (version 9.1 for Windows; SAS Institute, Cary, North Carolina, USA).
Results
The mean age of all subjects was 57±10.8 years. Ten subjects (25%) were men, 35 (88%) were white, and 31 (78%) had a body mass index of ≥25 kg/m2. Twenty-six knees (33%) were KL grade 0, nine knees (11%) were grade 1, 16 knees (20%) were grade 2, 22 knees (28%) were grade 3, seven knees (9%) were grade 4, and 45 knees (57%) were grade ≥2 (i.e., had radiographic knee osteoarthritis).
Agreement between the experienced and inexperienced reader for osteophyte assessment on tomosynthesis images is presented in Table 1. Of 320 observations (80 knees, 4 locations in each knee), two readers gave the same grading in 199 observations. Overall, the inexperienced reader had a tendency to assign lower grades in regard to osteophyte size compared to the experienced reader. In terms of reliability, the experienced reader demonstrated “almost perfect” to “perfect” intrareader agreement for osteophytes and subchondral cysts (Table 2). The inexperienced reader had perfect intrareader agreement for subchondral cysts and substantial agreement for osteophytes (Table 2). Inter-reader agreement between the experienced and the inexperienced readers was substantial for graded osteophytes reading and detection of cysts and almost perfect for detection of osteophytes (Table 2, Fig. 2).
Table 1.
Agreement of osteophyte scoring based on the OARSI grading between the experienced reader and the inexperienced reader
| Grades by the experienced reader | Grades by the inexperienced reader | ||||
|---|---|---|---|---|---|
|
| |||||
| 0 | 1 | 2 | 3 | Total | |
| 0 | 142 | 4 | 6 | 1 | 153 |
| 1 | 31 | 12 | 5 | 1 | 49 |
| 2 | 10 | 16 | 12 | 2 | 40 |
| 3 | 10 | 5 | 30 | 33 | 78 |
| Total | 193 | 37 | 53 | 37 | 320 |
Eighty knees were observed at four locations (lateral femur, medial femur, lateral tibia, medial tibia) per knee, totaling 320 observations per reader. One score was assigned for each location. In case of a single osteophyte in a location, the score is based on that osteophyte. In case of multiple osteophytes in a location, only the score of the largest osteophyte was recorded.
Table 2.
Intrareader reliability of the experienced and inexperienced readers for semiquantitative scoring of osteophytes and detection of subchondral cysts
| Inter-reader | Intrareader (experienced) | Intrareader (inexperienced) | ||
|---|---|---|---|---|
| Osteophytes (graded) | % agreement weighted κ [95%CI] | 61% 0.72 [0.64–0.80] | 90% 0.93 [0.83–1.00] | 75% 0.79 [0.61–0.96] |
| Osteophytes (dichotomous) | % agreement weighted κ [95%CI] | 91% 0.82 [0.69–0.94] | 95% 0.86 [0.59–1.00] | 80% 0.61 [0.30–0.93] |
| Subchondral cysts (dichotomous) | % agreement weighted κ [95%CI] | 88% 0.66 [0.46–0.85] | 95% 0.83 [0.50–1.00] | 100% 1.00 [1.00–1.00] |
CI, confidence interval.
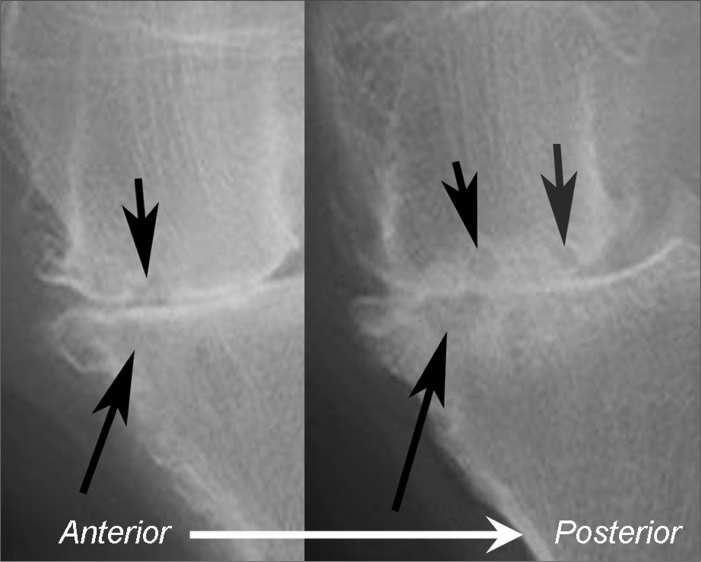
Figure 2.
Tomosynthesis images (anterior to posterior from left to right) show the right knee of a 56-year-old woman. The experienced reader detected a grade 2 osteophyte in the lateral femur (white arrow) and a grade 1 osteophyte in the lateral tibia (gray arrow). The inexperienced reader also detected the femoral grade 2 osteophyte, but failed to detect the smaller lesion.
On MRI, the expert reader detected 171 osteophytes. The experienced reader missed 33 of 171 (19%) osteophytes detected by the expert on MRI, while the inexperienced reader missed 54 of 171 MRI-detected osteophytes (32%) (Table 3). Sensitivity of osteophyte detection was 0.74–0.95 for the experienced reader and 0.54–0.75 for the inexperienced reader, for all locations of both knees. On MRI, the expert reader detected 51 subchondral cysts. On tomosynthesis images, the experienced reader detected 28 lesions and the inexperienced reader detected 37 lesions. However, the experienced and inexperienced readers missed 30 of 51 cysts (59%) and 26 of 51 cysts (51%) detected by the expert on MRI, respectively (Table 4). Both readers showed variable and same range of sensitivity (0.14–1.00) for the detection of subchondral cysts on all locations of both knees.
Table 3.
Diagnostic performance of the experienced and inexperienced readers for the detection of osteophytes using MRI reading by the expert reader as the reference standard
| Frequency (n=40) | Sensitivity | Specificity | Accuracy | |||
|---|---|---|---|---|---|---|
| Experienced reader | LF | L | 23 (58) | 0.83 (20/24) | 0.81 (13/16) | 0.83 (33/40) |
| R | 23 (58) | 0.88 (21/24) | 0.88 (14/16) | 0.88 (35/40) | ||
| MF | L | 20 (50) | 0.90 (19/21) | 0.95 (18/19) | 0.93 (37/40) | |
| R | 16 (40) | 0.89 (16/18) | 1.00 (22/22) | 0.95 (38/40) | ||
| LT | L | 23 (58) | 0.82 (18/22) | 0.72 (13/18) | 0.78 (31/40) | |
| R | 18 (45) | 0.74 (17/23) | 0.94 (16/17) | 0.83 (33/40) | ||
| MT | L | 21 (53) | 0.90 (18/20) | 0.85 (17/20) | 0.87 (35/40) | |
| R | 23 (58) | 0.95 (18/19) | 0.76 (16/21) | 0.85 (34/40) | ||
| Inexperienced reader | LF | L | 14 (35) | 0.54 (13/24) | 0.94 (15/16) | 0.70 (28/40) |
| R | 16 (40) | 0.67 (16/24) | 1.00 (16/16) | 0.80 (32/40) | ||
| MF | L | 16 (40) | 0.71 (15/21) | 0.95 (18/19) | 0.83 (33/40) | |
| R | 14 (35) | 0.72 (13/18) | 0.95 (21/22) | 0.85 (34/40) | ||
| LT | L | 18 (45) | 0.68 (15/22) | 0.83 (15/18) | 0.75 (30/40) | |
| R | 17 (43) | 0.74 (17/23) | 1.00 (17/17) | 0.85 (34/40) | ||
| MT | L | 17 (43) | 0.75 (15/20) | 0.90 (18/20) | 0.83 (33/40) | |
| R | 15 (38) | 0.68 (13/19) | 0.90 (19/21) | 0.80 (32/40) |
Frequency is given as n (%).
LF, lateral femur; L, left; R, right; MF, medial femur; LT, lateral tibia; MT, medial tibia.
Table 4.
Diagnostic performance of the experienced and inexperienced readers for the detection of subchondral cysts using MRI reading by the expert reader as the reference standard
| Frequency (n=40) | Sensitivity | Specificity | Accuracy | |||
|---|---|---|---|---|---|---|
| Experienced reader | LF | L | 1 (3) | 0.14 (1/7) | 1.00 (33/33) | 0.85 (34/40) |
| R | 4 (10) | 0.33 (2/6) | 0.94 (32/34) | 0.85 (34/40) | ||
| MF | L | 3 (8) | 0.43 (3/7) | 1.00 (33/33) | 0.90 (36/40) | |
| R | 4 (10) | 0.50 (2/4) | 0.94 (34/36) | 0.90 (36/40) | ||
| LT | L | 4 (10) | 0.38 (3/8) | 0.97 (31/32) | 0.85 (34/40) | |
| R | 4 (10) | 1.00 (2/2) | 0.95 (36/38) | 0.95 (38/40) | ||
| MT | L | 4 (10) | 0.44 (4/9) | 1.00 (31/31) | 0.88 (35/40) | |
| R | 4 (10) | 0.50 (4/8) | 1.00 (32/32) | 0.90 (36/40) | ||
| Inexperienced reader | LF | L | 1 (3) | 0.14 (1/7) | 1.00 (33/33) | 0.85 (34/40) |
| R | 3 (8) | 0.33 (2/6) | 0.97 (33/34) | 0.88 (35/40) | ||
| MF | L | 4 (10) | 0.57 (4/7) | 1.00 (33/33) | 0.93 (37/40) | |
| R | 2 (5) | 0.25 (1/4) | 0.97 (35/36) | 0.90 (36/40) | ||
| LT | L | 6 (15) | 0.63 (5/8) | 0.97 (31/32) | 0.90 (36/40) | |
| R | 7 (18) | 1.00 (2/2) | 0.87 (33/38) | 0.88 (35/40) | ||
| MT | L | 6 (15) | 0.56 (5/9) | 0.97 (30/31) | 0.88 (35/40) | |
| R | 8 (20) | 0.63 (5/8) | 0.91 (29/32) | 0.85 (34/40) |
Frequency is given as n (%).
LF, lateral femur; L, left; R, right; MF, medial femur; LT, lateral tibia; MT, medial tibia.
Discussion
The purpose of this study was to determine the reliability of tomosynthesis-based assessment of osteophytes and subchondral cysts. Overall, intra-reader agreement was “almost perfect” to “perfect” for both types of lesions in both experienced and inexperienced readers, except for the dichotomous reading of osteophytes by the inexperienced reader (which was “substantial”). For both lesions, inter-reader reliability between the two readers was “substantial” to “almost perfect” for both types of lesions.
Few publications have reported the use of tomosynthesis for in vivo imaging of skeletal pathologies (14–21). Some are simple case collections (16, 18, 19, 21); one is a scientific study but with no reported reliability assessment (20). Only three studies have reported reliability of tomosynthesis for assessment of skeletal pathology. Canella et al. (14) reported the use of tomosynthesis for evaluation of bone erosions in hand rheumatoid arthritis. They reported excellent intrareader reliability (intraclass correlation coefficient [ICC]=0.99) for an expert reader (17 years of experience in radiologic assessment of arthritis) and equally excellent inter-reader reliability (ICC=0.96) among three readers (other two readers having three and eight years of experience). Although they did not report intrareader reliability for these two readers, almost perfect inter-reader reliability implies that all readers were sufficiently “experienced”. In our study, the “experienced” reader had one year of relevant reading experience, and the “inexperienced” reader had no prior experience. Although our study cannot be directly compared with the Canella et al. (14) study since our focus is completely different (pathological features of the knee rather than the hand), both studies reported excellent intrareader reliability. In a study by Xia et al. (17), two “skilled” radiologists showed excellent inter-reader reliability (κ=0.91) for imaging assessment of subtle skeletal trauma (e.g., fractures of the bones in the limbs, nose, and pelvis) using tomosynthesis. However, the authors did not report years of experience or the type of imaging assessment the readers had. We have previously reported excellent intrareader reliability of tomosynthesis-based evaluation of osteophytes and subchondral cysts by an expert reader (15).
Because tomosynthesis offers images simulating “coronal slices” of the knee without the overlapping of normal bony contour seen on conventional anteroposterior or posteroanterior radiographs, marginal osteophytes should be clearly demonstrated, as previously reported (15). Although excellent inter-reader agreement was demonstrated for both graded reading and detection of osteophytes between the experienced and the inexperienced readers, the inexperienced reader did miss a large number of small (grade 1) osteophytes detected by the experienced reader. Using the MRI readings by the expert reader as a reference standard, the experienced reader demonstrated overall better sensitivity than the inexperienced reader for detection of osteophytes, indicating the inexperienced reader was missing the lesions that should have been detected, rather than the experienced reader over-reading the lesions that should not have been recorded as lesions. Also, when stratifying the knees according to KL grades, both readers had lower sensitivity for detection of osteophytes in lower KL grades but the experienced reader showed higher sensitivity than the inexperienced reader in all KL grades (i.e., 45% vs. 0% at KL grade 1, 87% vs. 57% at KL grade 2, 95% vs. 82% at KL grade 3, 91% vs. 87% at KL grade 4). Thus, failure of recognizing some of the small osteophytes as lesions, despite their depiction in the tomosynthesis image, seems to be a major factor affecting the inter-reader agreement. Detection of small osteophytes is important in osteoarthritis research studies because the presence of osteophytes defines the diagnosis of radiographic osteoarthritis (29). Missing small osteophytes could affect clinical studies in which participants are selected on the presence or absence of radiographic osteoarthritis. Screening images at the recruitment stage, therefore, should be read by experienced readers who have received training and validation of reading skills to avoid misclassification of subjects. Also, detection of small osteophytes on tomosynthesis images would be clinically important if they are predictive of subsequent development of symptomatic osteoarthritis. Determining whether they are in fact predictive will require longitudinal studies using tomosynthesis.
Both experienced and inexperienced readers showed a wide range of sensitivity (0.14–1.00) for detection of subchondral cysts in various locations of the knee joint. However, specificity as well as intrareader agreement was excellent for both readers. In particular, the inexperienced reader achieved perfect intrareader agreement, which is due to the fact that this reader consistently failed to detect lesions on both readings. Despite the tomographic nature of tomosynthesis, detection of subchondral cysts still seems to be difficult regardless of reader experience. This may be due to an inherent limitation of tomosynthesis as an imaging modality for depiction of subchondral cyst compared to MRI.
A limitation of the present study is the low frequency of subchondral cysts in our study sample (3%–15% in all locations). Both experienced and inexperienced readers had a notable amount of disagreement for detection of subchondral cysts (Fig. 3). However, the frequency of the lesion was so low that all three readers reliably recorded the absence of the lesion on most knees. Overall, all readers had almost perfect intrareader agreement, but inter-reader agreement was not as good. The fact that only 57% of subjects had radiographic knee osteoarthritis is likely to have contributed to the low frequency of the cysts. Including more patients with confirmed radiographic knee osteoarthritis (KL grade 2 or above) presumably would have increased the number of lesions available for detection and strengthened the analysis of reliability.
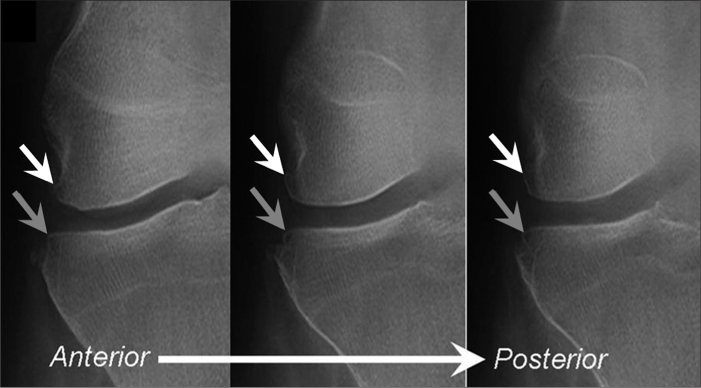
Figure 3.
Left knee of a 64-year-old woman. This case was read twice for the purpose of intrareader reliability evaluation. Tomosynthesis images (anterior to posterior from left to right) reveal small subchondral cysts in the medial femur (short black arrows) and a large subchondral cyst in the medial tibia (long black arrow). The experienced reader detected all lesions on the first and second readings, while the inexperienced reader missed the large cyst in the tibia (long black arrows) on both readings. Despite the discrepancy in the readings between the two readers, each reader demonstrated consistent readings, contributing to overall almost perfect intrareader agreement for subchondral cysts evaluation.
Using conventional radiography, intrareader reliability for assessment of knee osteoarthritis features has been reported to be lower for less experienced readers in general, even after receiving intensive training, compared to a more experienced reader (23). The same trend was observed in the present study for the tomosynthesis assessment of osteophytes, but not for subchondral cysts.
The technique of tomosynthesis has limitations compared to conventional radiography. Firstly, patients are exposed to slightly higher dose of radiation during tomosynthesis imaging. The mean total radiation dose per patient was 0.038 mGy for knee radiography and 0.16 mGy for tomosynthesis of the knee (15). The mean effective dose was 0.0018 mSv for radiography and 0.0076 mSv for tomosynthesis (15, 26). Secondly, time taken to review the acquired images takes longer for tomosynthesis since there are multiple images per patient to read. Lastly, clinical significance of the use of tomosynthesis in imaging of knee osteoarthritis remains unclear at present.
In conclusion, tomosynthesis enables radiologists with different levels of expertise to evaluate osteophytes and subchondral cysts with excellent intrareader reliability regardless of experience, so long as the reader is adequately trained. Experience, however, still seems to be a significant factor for accurate detection of osteophytes, since readers with less experience have less sensitivity compared to the expert reader.
Footnotes
Conflict of interest disclosure
This research study was financially supported by a research grant from GE Healthcare. Imaging equipment for the tomosynthesis imaging was provided by the same sponsor. However, the sponsor did not have any role in the study design, data interpretation, and analysis presented in this article. Authors had full control of the data and the information submitted for publication. None of the authors are employed by or offer consultancy services for the sponsor.
References
- 1.Dobbins JT, 3rd, McAdams HP. Chest tomosynthesis: technical principles and clinical update. Eur J Radiol. 2009;72:244–251. doi: 10.1016/j.ejrad.2009.05.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yamada Y, Jinzaki M, Hashimoto M, et al. Tomosynthesis for the early detection of pulmonary emphysema: diagnostic performance compared with chest radiography, using multidetector computed tomography as reference. Eur Radiol. 2013;23:2118–2126. doi: 10.1007/s00330-013-2814-1. [DOI] [PubMed] [Google Scholar]
- 3.Lee G, Jeong YJ, Kim KI, et al. Comparison of chest digital tomosynthesis and chest radiography for detection of asbestos-related pleuropulmonary disease. Clin Radiol. 2013;68:376–382. doi: 10.1016/j.crad.2012.05.022. [DOI] [PubMed] [Google Scholar]
- 4.Vult von Steyern K, Bjorkman-Burtscher IM, Hoglund P, Bozovic G, Wiklund M, Geijer M. Description and validation of a scoring system for tomosynthesis in pulmonary cystic fibrosis. Eur Radiol. 2012;22:2718–2728. doi: 10.1007/s00330-012-2534-y. [DOI] [PubMed] [Google Scholar]
- 5.Hakim CM, Chough DM, Ganott MA, Sumkin JH, Zuley ML, Gur D. Digital breast tomosynthesis in the diagnostic environment: A subjective side-by-side review. AJR Am J Roentgenol. 2010;195:W172–176. doi: 10.2214/AJR.09.3244. [DOI] [PubMed] [Google Scholar]
- 6.Noroozian M, Hadjiiski L, Rahnama-Moghadam S, Klein KA, Jeffries DO, Pinsky RW, et al. Digital breast tomosynthesis is comparable to mammographic spot views for mass characterization. Radiology. 2012;262:61–68. doi: 10.1148/radiol.11101763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Skaane P, Bandos AI, Gullien R, et al. Comparison of digital mammography alone and digital mammography plus tomosynthesis in a population-based screening program. Radiology. 2013;267:47–56. doi: 10.1148/radiol.12121373. [DOI] [PubMed] [Google Scholar]
- 8.Machida H, Yuhara T, Ueno E, et al. Detection of paranasal sinus opacification with digital tomosynthesis radiography: a clinical pilot study. J Comput Assist Tomogr. 2013;37:252–256. doi: 10.1097/RCT.0b013e31827c0cb1. [DOI] [PubMed] [Google Scholar]
- 9.Kitai N, Mukai Y, Murabayashi M, et al. Measurement accuracy with a new dental panoramic radiographic technique based on tomosynthesis. Angle Orthod. 2013;83:117–126. doi: 10.2319/020412-100.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gomi T, Yokoi N, Hirano H. Evaluation of digital linear tomosynthesis imaging of the temporomandibular joint: initial clinical experience and evaluation. Dentomaxillofac Radiol. 2007;36:514–521. doi: 10.1259/dmfr/26026102. [DOI] [PubMed] [Google Scholar]
- 11.Rowberry BK, Galea A. Intravenous pyelogram artefacts unique to digital tomosynthesis reconstruction. Br J Radiol. 2011;84:1050–1054. doi: 10.1259/bjr/59924754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ng SK, Zygmanski P, Lyatskaya Y, D’Amico AV, Cormack RA. Localization of a portion of an endorectal balloon for prostate image-guided radiation therapy using cone-beam tomosynthesis: a feasibility study. Int J Radiat Oncol Biol Phys. 2012;83:e257–264. doi: 10.1016/j.ijrobp.2011.12.036. [DOI] [PubMed] [Google Scholar]
- 13.Kim EY, Chung MJ, Choe YH, Lee KS. Digital tomosynthesis for aortic arch calcification evaluation: performance comparison with chest radiography with CT as the reference standard. Acta Radiol. 2012;53:17–22. doi: 10.1258/ar.2011.110347. [DOI] [PubMed] [Google Scholar]
- 14.Canella C, Philippe P, Pansini V, Salleron J, Flipo RM, Cotten A. Use of tomosynthesis for erosion evaluation in rheumatoid arthritic hands and wrists. Radiology. 2011;258:199–205. doi: 10.1148/radiol.10100791. [DOI] [PubMed] [Google Scholar]
- 15.Hayashi D, Xu L, Roemer FW, et al. Detection of osteophytes and subchondral cysts in the knee with use of tomosynthesis. Radiology. 2012;263:206–215. doi: 10.1148/radiol.12111649. [DOI] [PubMed] [Google Scholar]
- 16.Lacout A, Thariat J, El Hajjam M, Marcy PY. Insight into osteo-articular digital tomosynthesis: a pictorial essay. J Med Imaging Radiat Oncol. 2013;57:45–49. doi: 10.1111/j.1754-9485.2012.02412.x. [DOI] [PubMed] [Google Scholar]
- 17.Xia W, Yin XR, Wu JT, Wu HT. Comparative study of DTS and CT in the skeletal trauma imaging diagnosis evaluation and radiation dose. Eur J Radiol. 2013;82:e76–80. doi: 10.1016/j.ejrad.2012.09.008. [DOI] [PubMed] [Google Scholar]
- 18.Machida H, Yuhara T, Sabol JM, Tamura M, Shimada Y, Ueno E. Postoperative follow-up of olecranon fracture by digital tomosynthesis radiography. Jpn J Radiol. 2011;29:583–586. doi: 10.1007/s11604-011-0589-3. [DOI] [PubMed] [Google Scholar]
- 19.Gazaille RE, 3rd, Flynn MJ, Page W, 3rd, Finley S, van Holsbeeck M. Technical innovation: digital tomosynthesis of the hip following intra-articular administration of contrast. Skeletal Radiol. 2011;40:1467–1471. doi: 10.1007/s00256-011-1247-7. [DOI] [PubMed] [Google Scholar]
- 20.Geijer M, Borjesson AM, Gothlin JH. Clinical utility of tomosynthesis in suspected scaphoid fracture. A pilot study. Skeletal Radiol. 2011;40:863–867. doi: 10.1007/s00256-010-1049-3. [DOI] [PubMed] [Google Scholar]
- 21.Mermuys K, Vanslambrouck K, Goubau J, Steyaert L, Casselman JW. Use of digital tomosynthesis: case report of a suspected scaphoid fracture and technique. Skeletal Radiol. 2008;37:569–572. doi: 10.1007/s00256-008-0470-3. [DOI] [PubMed] [Google Scholar]
- 22.Duryea J, Dobbins JT, 3rd, Lynch JA. Digital tomosynthesis of hand joints for arthritis assessment. Med Phys. 2003;30:325–333. doi: 10.1118/1.1543573. [DOI] [PubMed] [Google Scholar]
- 23.Gunther KP, Sun Y. Reliability of radiographic assessment in hip and knee osteoarthritis. Osteoarthritis Cartilage. 1999;7:239–246. doi: 10.1053/joca.1998.0152. [DOI] [PubMed] [Google Scholar]
- 24.Kothari M, Guermazi A, von Ingersleben G, et al. Fixed-flexion radiography of the knee provides reproducible joint space width measurements in osteoarthritis. Eur Radiol. 2004;14:1568–1573. doi: 10.1007/s00330-004-2312-6. [DOI] [PubMed] [Google Scholar]
- 25.GE Healthcare. Digitial X-ray systems and advanced applications from GE Health-care are driving workflow and helping facilities change patient protocols: diagnosis and treatment. Available at: http://genewscenter.com/Press-Releases/Digital-X-Ray-Systems-and-Advanced-Applications-From-GE-Healthcare-Are-Driving-Workflow-and-Helping-23d3.aspx. Accessed April 2, 2013.
- 26.Sabol JM. A Monte Carlo estimation of effective dose in chest tomosynthesis. Med Phys. 2009;36:5480–5487. doi: 10.1118/1.3250907. [DOI] [PubMed] [Google Scholar]
- 27.Altman RD, Gold GE. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthritis Cartilage. 2007;15(Suppl A):A1–56. doi: 10.1016/j.joca.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 28.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 29.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]