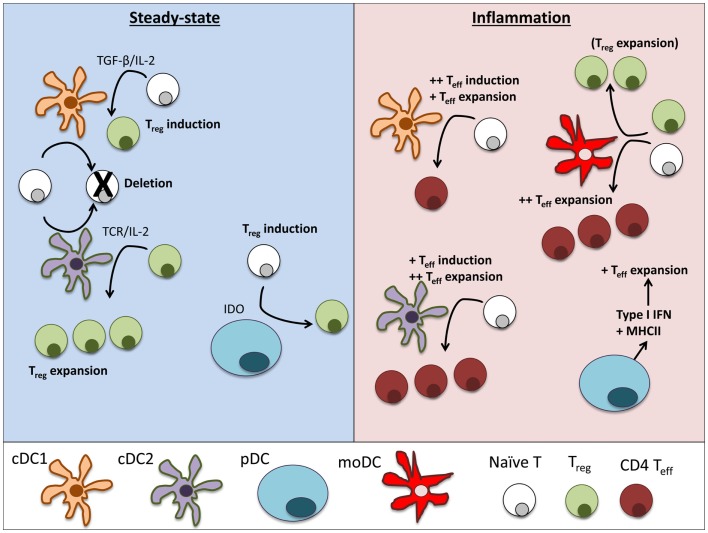
Figure 2.
Dendritic cell subsets perform particular functions in steady-state and inflammation. In steady-state tissues (left panel), lymphoid-resident cDC1 and cDC2 bearing self-antigen can both suboptimally stimulate naïve CD4+ and CD8+ T cells and cause deletional tolerance of autoreactive cells. A subset of naïve CD4+ T cells that are stimulated by cDC1 will encounter TGF-β on the DC and induce Foxp3 and become a Treg. If a Treg is stimulated by cDC2, it will clonally expand that population of Tregs. pDCs have limited capacity to stimulate CD4+ T cells directly due to low MHCII and costimulatory molecule levels. Under certain conditions, pDCs have been demonstrated to produce IDO and induce Treg generation. During inflammation (right panel), cDCs mature and can stimulate effector T cell responses, including Th1 and Th17 cells often associated with autoimmune disease. cDC1 can induce strong Th1 responses from naïve cells and cDC2 are more efficient in expanding CD4 Teff. pDCs respond to inflammation by secreting large amounts of type I interferons that can significantly alter the pathogenesis of autoimmune diseases. Inflamed pDCs also upregulate MHCII, allowing efficient antigen presentation. moDCs mature from circulating monocytes (Ly6+ in mice, CD14+ in humans) as they enter inflamed tissues. moDCs are adept at inducing Th1 responses via secretion of IL-12, but can also expand Tregs in some circumstances.