Abstract
Background:
Distal radius fractures (DRFs) are much more prone to malunion than unstable extra-articular fractures. There is no clear consensus concerning what the proper treatment should be, and the best approach to use for displaced DRFs remains challenging.
Objective:
To compare the effect of two different therapeutic surgical methods, i.e., volar plate fixators and external fixators, on outcomes of patients with intra-articular distal radius fractures.
Methods:
From May 2010 to November 2014, 76 subjects who had experienced intra-articular fractures of the distal radius were enrolled in this double-blind, randomized, controlled trial in Imam Ali Hospital in Bojnourd, Iran. The patients were divided into two groups, i.e., 1) patients who were treated with internal fixation using the volar plate (group A) and 2) patients who were treated with external fixators (group B). The primary outcome was a composite measure of the patient’s quality of life using three different scores, i.e., 1) the MAYO score, 2) Disabilities of the Arm, Shoulder, and Hand (DASH (score, and 3) the Short Form (36) (SF-36) Health Survey score.
Results:
A total of 76 patients were allocated randomly to groups A and B. The mean ages for external fixator cases and volar plate cases were 51.7 and 46.3, respectively. No significant age distribution was seen between the two groups (p=0.348). Gender distribution between the two groups was not significantly different (p=0.022). Grip power was significantly different between the two groups, but no significant differences were detected in range of motion (p=0.008, p=0.367, respectively). The MAYO score was significantly higher in the open reduction and internal fixation (ORIF) group, and, according to the SF-36 test, the ORIF group also a higher level of general mental and physical health, social functioning, and personal physical functioning than the other group. However, postoperatively, the mental discomfort and physical discomfort were more prevalent in the external fixator group. The DASH score was not significantly different between the two groups (p=0.124).
Conclusions:
ORIF and its subtitle, volar plate fixation, is a more preferred surgical procedure than the external fixator for the treatment of intra-articular distal radius fractures. This conclusion is important when one considers cost-effectiveness and an earlier return to work.
Trial registration:
The trial is registered at the Thai Clinical Trial Registry (clinicaltrials.in.th) with the TCR identification number TCTR20150609002
Funding:
The authors received no financial support for the research, authorship, and/or publication of this article.
Keywords: Distal radius fracture, External fixator method, Internal fixation
1. Introduction
Distal radius fractures (DRFs) comprise 16% of all fractures that are treated surgically. Despite the high prevalence of this kind of fracture and more than two decades of experience in treating DRFs, there is still no consensus concerning the preferred way to manage this type of fracture. Another issue of significant concern is that the approach to dealing with intra-articular fractures of the distal radius remains even more challenging to treat than unstable extra-articular fractures (1). DRFs are of the most prevalent fractures in middle-aged and elderly people (2, 3), so such fractures are an important concern. According to recent findings, distal radius fractures are occurring at an increasing rate in both males and females. There has been an especially sharp increase in incidents among women older than 40, and this brings into sharper focus the possible consequence of estrogen withdrawal and loss of bone density (4). Unfortunately, such fractures are difficult to reduce and stabilize, so they are prone to malunion (5). Also, they are prone to result in malfunctioning of the wrist and hand (which depends on radius alignment and the positioning of the carpal and ulnar joints) (6). Such fractures can cause deterioration of the long-term functional outcome they are not reduced well and in an anatomically correct manner (7, 8).
Since these fractures can occur at any age and can affect the daily functions of life, different treatment modalities have been developed, ranging from casting, which is the oldest modality, to the use of external fixators, percutanous insertion of pins, and open fixation with a plate. Even so, there seems to be no preferred means for managing displaced DRFs based on a comparison of the results achieved by the various approaches (9). It is important to recognize that ancient evidence suggested that locking plate fixation allowed the patients to move their hands and wrists much sooner, which allowed them to conduct various activities for themselves in a shorter period of time and to return to work sooner. So, treatment modalities for these fractures have gone through significant changes during the last 20 years. Nevertheless, even though these outcomes are favorable, to our knowledge, no randomized controlled clinical trial has been conducted in Iran to clarify whether the more invasive and more costly plating modality is preferable to the other simpler approaches. This study compared clinical outcomes of the two surgical modalities, i.e., open reduction and internal fixation (ORIF) and the use of external fixators on our patients whose ages ranged from 25 to 70 years.
2. Material and Methods
2.1. Trial design
We conducted a single-center, prospective, double-blind, randomized controlled trial that was approved by review board of Bojnourd University of Medical Sciences. Seventy-six subjects with 80 intra-articular fractures of the distal radius, who were admitted to the Orthopedics Ward at Imam Ali Hospital in Bojnourd, Iran, from 2010 to 2014, were enrolled in the study. The patients were divided into two groups, i.e., 1) the patients who were treated with internal fixation using the volar plate (group A) and 2) the patients who were treated with external fixators (group B). We allocated the patients randomly to the two groups, and they were randomized to two study arms in two phases. At the first randomization, the participants who had been chosen for the internal fixation underwent further randomization for treatment with either a volar plate or a radial column plate. Then, the patients were selected randomly to be treated with either augmented external fixation or internal fixation. The primary outcome was a composite measure of the patient’s quality of life based on the MAYO, DASH, and SF-36 scores.
2.2. Participants
All patients with unstable distal radial fractures who were at least 25 years old were enrolled in the study. The fractures were presumed to be unstable if they had been displaced after initial open or closed reduction and splinting. Patients who had stable fractures, who were less than 25 years old, or who had any systemic diseases that made them unable to undergo surgery were excluded from the study.
2.3. Interventions
A plate was inserted on the radial column through an approximately 8-cm incision in the forearm, from the tip of the radial styloid to the proximal. In order to reduce the deforming forces of the brachioradialis on the distal fracture fragment and also on the usage of the brachioradialis tendon, this tendon was reflected approximately 10 cm proximal to its distal insertion into the radial metaphysis for soft-tissue coverage over the plate. The operation was performed on the fracture through an incision on the radial aspect and was reduced by direct manipulation, under visual and as well as a fluoroscopic guide. All patients were provided standardized follow-up care, including instructions for immediately beginning the move the fingers, a volar splint for the patient’s comfort, and hand therapy that included wrist motion and strengthening exercises. This care began at the tenth to fourteenth day after surgery. Some additional therapies were done, such as cancellous bone allograft filling of a metaphyseal space and/or insertion of buttress plates, based on the surgeon’s request. Pins also were inserted, and all external fixators were removed during the fifth or sixth week after surgery. Hand strengthening and wrist range of motion exercises were initiated at the same time.
2.4. Outcomes
After surgery, the patients were evaluated on day 14, during the sixth week, during the third month, and during the sixth month concerning the presumed primary outcome measure. Pain was recorded, based on the 10-point visual analog scale, and all patients also were asked to complete the DASH questionnaire concerning disabilities of the arm, shoulder, and hand at each follow-up visit. The scores that were obtained at their first visit immediately after their injury were used as the baseline level of their functionality. The DASH questionnaire is a 30-item, self-reported questionnaire that measures the ability of a patient to perform certain upper extremity activities after injury, by rating from 0 points (no disability) to 100 points (maximum disability) (3). Secondary outcomes, such as wrist and forearm motion and also grip and lateral pinch strength were measured at the sixth week after surgery. We also evaluated the wrist flexion-extension motion and amounts of radioulnar deviation using a goniometer. The range of motion and lateral pinch strength ratios also were calculated because they were more sensitive in the appraisal of clinical changes. The means of these three trials for both hands was recorded for all strength measurements.
2.5. Sample size
This study was performed on 76 patients with 80 intra-articular fractures of the distal radius who were treated with internal fixation using the volar plate and an external fixator. These patients underwent either volar plate fixation or external fixator procedure after considering the inclusion and exclusion criteria.
2.6. Randomization
Patients were randomized to two study arms in two phases. The patients who were treated with internal fixation were randomized again to determine whether a volar plate or a radial column plate would be inserted. Then, the patients were selected randomly to be treated with either augmented external fixation. We chose this randomization scheme to balance the two kinds of surgery (internal and external fixation), thereby eliminating comparative bias. A single surgeon only did the augmented external fixation, and a second surgeon only did the internal fixation surgery. The patients were not aware of the kind of surgery that had been selected for them.
2.7. Blinding
This was a partially-blinded study because the kind of modality used for the patients was evident due to the residual surgical scars. We tried to diminish the bias by blinding the collector and analyzer of the clinical and radiographic outcomes data to the type of modalities that was used for each group. We used anyone except the surgeons to collect the data.
2.8. Statistical methods
Demographic features and standard radiographic values were documented, and MAYO, DASH and SF-36 exams were performed. The results were compared between the two groups, i.e., those with volar plate fixation and those with external fixators. We visited the patients at two weeks, six weeks, and six months after surgery, and control radiographs were taken. At the last visit, MAYO, DASH and SF-36 questionnaires were completed. X-rays were used to evaluate the radiological values, and we used a dynamometer to assess the grip power. An orthopedic ruler was used to evaluate range of motion. The results of the treatments were assessed using the MAYO, DASH, and SF-36 questionnaires. The MAYO questionnaire consisted of four rankings, including pain, range of motion, grip power, and function, each of which could be scored from 0 to 25, with 25 in all four of these rankings indicating favorable function of the wrist. The DASH questionnaire consisted of 30 questions that assessed the mental and physical health condition considering physical function, physical role limitation, pain, general health, energy, fatigue, social function, emotional role limitation, and mental health. All of the data that were collected were analyzed statistically.
2.9. Research ethics
All patients signed an informed consent form. In addition, the study was approved by the Ethics Committee at Bojnourd University of Medical Sciences.
3. Results
This was a clinical trial performed on 80 patients with intra-articular distal radius fractures. During the first follow-up visit, all of the patients revealed a mean post-operative baseline DASH score of 82±21 points, indicating significant function impairment. There was no significant difference among the groups at this time. At the follow-up during the sixth week, the mean DASH score in the volar plate group was significantly better than that in the external fixation group (p=0.047). Interestingly, at follow-up during the sixth month after surgery, the mean DASH score in the volar plate group was significantly better than that in both the external fixation group (p=0.035) and radial column group (p=0.000). At the final follow-up six months after surgery, the mean DASH score for all patients was 15±16 points. The mean ages for the patients who received the external fixator and those who received the volar plate were 51.7 and 46.3, respectively. No significant age distribution was seen between the two groups (p=0.348) (Table 1).
Table 1.
Mean and SD of age distribution in the external fixator and volar plate fixation groups, analyzed by t-test
| Group | Minimum age (Year) | Maximum age (Year) | Mean (Year) | Standard deviation | P value |
|---|---|---|---|---|---|
| External fixator | 27 | 49 | 48.3 | 4.2 | 0.193 |
| Volar Plate | 23 | 49 | 46.3 | 5.5 | 0.119 |
| All patient | 23 | 49 | 45 | 5.5 | 0.348 |
The patients’ ages were the only data that was normally distributed (p>0.05). In the external fixator group, 27 of the patients (55%) were female and 23 (45%) were male. There were 14 (35%) females and 26 (65%) males in the plate group. The distribution of the genders between the two groups was not significantly different (p=0.022) (Table 2). No significant difference was seen in dominant hand (p=0.53). There was a significant difference in the length of the radius (p=0.012). In order to evaluate the effect of age, gender, and treatment modality in the length of the radius, a multivariable logistic regression modality had a significant effect (p=0.027), but age and gender did not (p>0.05).
Table 2.
Gender distribution in external fixator and volar plate fixation groups analyzed by Pearson Chi-Squared
| Gender | Male | Female | All patients | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| External fixator group | 23 | 45 | 27 | 55 | 50 | 100 |
| Volar Plate fixation group | 32.5 | 65 | 17.5 | 35 | 50 | 100 |
| All patients | 55 | 55 | 45 | 45 | 100 | 100 |
| P value | p=0.123 | p=0.345 | p=0.022 | |||
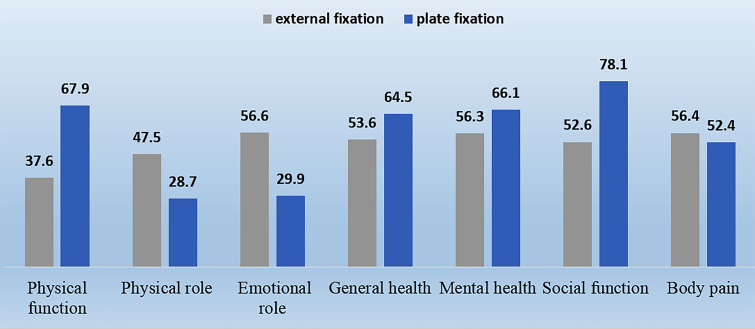
There was no significant difference in volar tilt between two groups (p=0.057). We assessed the effect of age, gender, and treatment modality on volar tilt using a multivariate logistic regression model, which showed no significant effect (p>0.05). There was a noticeable difference between the grip power of the two groups (p<0.05). A multivariate linear model was used to assess the effects of age, gender, and treatment modality on grip power, and the effects were significant (p<0.05). There was no significant difference between the DASH scores of the groups (p=0.578). There was a noticeable statistical difference in the MAYO scores of the groups (p<0.05). Figure 1 summarizes the data concerning the patients’ quality of life.
Figure 1.
Quality of life (SF-36) in the external fixator and volar plate fixation groups
No significant differences were observed between the two groups based on age or gender. Acceptable radiographic values, volar tilt, and radial length were observed to a greater extent in the ORIF group, and grip power was significantly different between the two groups. However, no significant differences was detected in range of motion (p=0.008, p=0.367). In addition, the MAYO score was significantly higher in the ORIF group, and, according to the SF-36 test, all of the members of the ORIF group had higher levels of general mental and physical health as well as social, personal, and physical functioning. Conversely, mental discomfort and physical discomfort were more prevalent post-operatively in the external fixator group. The DASH scores were not significantly different between the two groups (p=0.124).
4. Discussion
In this study, variables such as age, gender, the dominant hand, standard radiographic values, grip power, and range of motion in flexion–extension were evaluated. Also, MAYO, DASH, and SF-36 tests were performed, and the results were compared between the plate fixation group and the external fixation group. In the external fixation group, 55% of the patients were female, and 45% were male. In the plate fixation group, 35% of the patients were female, and 65% were male. Gender distribution was not significantly different between the two groups. In the Rizzo’s study, most of the patients were female. The ratios of females to males for the external fixation and plate fixation groups were 8/6 and 25/6, respectively (9). In this study, the mean ages of the external fixation and plate fixation patients were 40.1 and 38.3, respectively. The age distribution between the two groups was not noticeably different. In the Rizzo study, the mean ages in the external fixation and plate fixation groups were 48 and 45, respectively (9).
Judys et al. suggested that performing plate fixation on youth will have more favorable outcomes. Generally, neither age nor gender distribution made a significant difference between the two groups, an observation that was similar to Phandis’ results (10). In our study, 55% of the patients in the external fixator group had dominant hand involvement, while this was true of only 45% of the patients in the plate fixation group. The difference between the groups with respect to the dominant hand was not significant. Our radiographic results in the plate fixation group were more favorable than in the external fixator group. The percentage of patients with acceptable volar tilt and radial length in plate fixation group was 97.5%, these two variables for the external fixator group were 82.5 and 80%, respectively. No significant difference was seen for the volar tilt in the two groups, but the difference in radial length was significant. In the Rizzo study, the number of patients with acceptable volar tilt and radial length in the plate fixation group was noticeably greater than the number in the external fixator group, which supports our results. Neander also indicated great outcomes of plate fixation in radiographic assessments, but Dorbetz showed that both plate fixation and external fixator gave the same radiographic values, range of motion, and grip power which was different from our results (11, 12).
Kilick showed that post-operative radiographic values, such as volar tilt, radial length, and ulnar length were completely different from their pre-operative values and similar to the uninvolved hand, which also supports our results (13). Zhang et al. also suggested that palmar tilt after performing plate fixation in distal radius fractures is quite different from the pre-operative value and similar to the uninvolved hand; they also stated that radius shortening or decrease in the radial length did not occur after plate fixation, which also supports our results (13, 14). In our study, the use of the SF-36 test showed that general and mental health and physical and social function levels were higher in the plate fixation group. The test results also indicated that post-operative pain and mental and physical discomfort were observed more often among members of the external fixator group.
The mean DASH scores were not significantly different between the two groups; they showed the same range of disability for both of these modalities. Aktekia estimated the DASH score in patients in the external fixator group to be 21.9, which was less than our findings (15, 16). Phandi et al. reported a score of 2.3 for the plate fixation group, which was also less than our result. In this study, assessing the radiographic and functional values after performing either external fixator of plate fixation on distal radius fractures showed that the latter had more favorable outcomes and was preferred if its requirements are accessible and it is possible to perform surgery (17).
5. Conclusions
Collectively, we concluded that ORIF (volar plate fixation) was the preferred surgical procedure for the treatment of intra-articular distal radius fracture. This is important, especially when cost-effectiveness and a faster return to work are considered. Large-scale clinical trials should be conducted to confirm the validity of our findings.
Acknowledgments
We thank the Research Vice Chancellor at Bojnourd University of Medical Sciences for supporting this study. We also express our grateful appreciation for the kind assistance of the personnel in the Orthopedic Ward at Imam Ali Hospital in Bojnourd, Iran.
Footnotes
Registration code:
TCTR20150609002
Funding:
The authors received no financial support for the research, authorship, and/or publication of this article.
Conflict of Interest:
There is no conflict of interest to be declared.
Authors’ contributions:
Both of authors contributed to this project and article equally. Both authors read and approved the final manuscript.
References
- 1.Cooney W, Linscheid R, Dobyns J. External pin fixation for unstable Colles’ fractures. J Bone Joint Surg Am. 1979;61(6A):840–5. [PubMed] [Google Scholar]
- 2.Arora R, Lutz M, Deml C, Krappinger D, Haug L, Gabl M. A prospective randomized trial comparing nonoperative treatment with volar locking plate fixation for displaced and unstable distal radial fractures in patients sixty-five years of age and older. J Bone Joint Surg Am. 2011;93(23):2146–53. doi: 10.2106/JBJS.J.01597. [DOI] [PubMed] [Google Scholar]
- 3.Arora R, 1, Gabl M, Erhart S, Schmidle G, Dallapozza C, Lutz M. Aspects of current management of distal radius fractures in the elderly individuals. Geriatr Orthop Surg Rehabil. 2011;2(5–6):187–94. doi: 10.1177/2151458511426874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Plate JF, Gaffney DL, Emory CL, Mannava S, Smith BP, Koman LA, et al. Randomized comparison of volar locking plates and intramedullary nails for unstable distal radius fractures. J Hand Surg Am. 2015;40(6):1095–101. doi: 10.1016/j.jhsa.2015.02.014. [DOI] [PubMed] [Google Scholar]
- 5.Xia S, Lu Y, Wang H, Wu Z, Wang Z. Open reduction and internal fixation with conventional plate via L-shaped lateral approach versus internal fixation with percutaneous plate via a sinus tarsi approach for calcaneal fractures - a randomized controlled trial. Int J Surg. 2014;12(5):475–80. doi: 10.1016/j.ijsu.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 6.Osada D, Kamei S, Masuzaki K, Takai M, Kameda M, Tamai K. Prospective study of distal radius fractures treated with a volar locking plate system. J Hand Surg Am. 2008;33(5):691–700. doi: 10.1016/j.jhsa.2008.01.024. [DOI] [PubMed] [Google Scholar]
- 7.Noble P, Marshall A, Barron O, Catalano L. Malpractice in distal radius fracture management: an analysis of closed claims. J Hand Surg Am. 2014;39(8):1480–8. doi: 10.1016/j.jhsa.2014.02.019. [DOI] [PubMed] [Google Scholar]
- 8.Chung K, Shauver M, Birkmeyer J. Trends in the United States in the treatment of distal radial fractures in the elderly. J Bone Joint Surg Am. 2009;91(8):1868–73. doi: 10.2106/JBJS.H.01297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leung F, Tu Y, Chew W, Chow S. Comparison of external and percutaneous pin fixation with plate fixation for intra-articular distal radial fractures. A randomized study. J Bone Joint Surg Am. 2008;90(1):16–22. doi: 10.2106/JBJS.F.01581. [DOI] [PubMed] [Google Scholar]
- 10.Valdes K, Naughton N, Burke C. Therapist-supervised hand therapy versus home therapy with therapist instruction following distal radius fracture. J Hand Surg Am. 2015;40(6):1110–16. doi: 10.1016/j.jhsa.2015.01.036. [DOI] [PubMed] [Google Scholar]
- 11.Brehmer J, Husband J. Accelerated rehabilitation compared with a standard protocol after distal radial fractures treated with volar open reduction and internal fixation: a prospective, randomized, controlled study. J Bone Joint Surg Am. 2014;96(19):1621–30. doi: 10.2106/JBJS.M.00860. [DOI] [PubMed] [Google Scholar]
- 12.Gradl G, Mielsch N, Wendt M, Falk S, Mittlmeier T, Gierer P, et al. Intramedullary nail versus volar plate fixation of extra-articular distal radius fractures. Two year results of a prospective randomized trial. Injury. 2014;45(Suppl 1):S3–8. doi: 10.1016/j.injury.2013.10.045. [DOI] [PubMed] [Google Scholar]
- 13.Goehre F, Otto W, Schwan S, Mendel T, Vergroesen P, Lindemann L. Comparison of palmar fixed-angle plate fixation with K-wire fixation of distal radius fractures (AO A2, A3, C1) in elderly patients. J Hand Surg Eur. 201439(3):249–57. doi: 10.1177/1753193413489057. [DOI] [PubMed] [Google Scholar]
- 14.Arora R, Lutz M, Deml C, Krappinger D, Haug L, Gabl M. A prospective randomized trial comparing nonoperative treatment with volar locking plate fixation for displaced and unstable distal radial fractures in patients sixty-five years of age and older. J Bone Joint Surg Am. 2011;93(23):2146–53. doi: 10.2106/JBJS.J.01597. [DOI] [PubMed] [Google Scholar]
- 15.Fadyen I, Field J, McCann P, Ward J, Nicol S, Curwen C. Should unstable extra-articular distal radial fractures be treated with fixed-angle volar-locked plates or percutaneous Kirschner wires? A prospective randomised controlled trial. Injury. 2011;42(2):162–6. doi: 10.1016/j.injury.2010.07.236. [DOI] [PubMed] [Google Scholar]
- 16.Zettl R, Clauberg E, Nast-Kolb D, Ruchholtz S, Kühne C. Volar locking compression plating versus dorsal plating for fractures of the distal radius: a prospective, randomized study. Unfallchirurg. 2009;112(8):712–8. doi: 10.1007/s00113-008-1526-5. [DOI] [PubMed] [Google Scholar]
- 17.Wei D, Raizman N, Bottino C, Jobin C, Strauch R, Rosenwasser M. Unstable distal radial fractures treated with external fixation, a radial column plate, or a volar plate. A prospective randomized trial. J Bone Joint Surg Am. 2009;91(7):1568–77. doi: 10.2106/JBJS.H.00722. [DOI] [PubMed] [Google Scholar]