Abstract
Background
Although a number of studies have examined the factor structure of the Edinburgh Postnatal Depression Scale (EPDS) in predominately White or African American samples, no published research has reported on the factor structure among Hispanic women who reside in the United States.
Objective
The current study examined the factor structure of the EPDS among Hispanic mothers in the United States.
Method
Among 220 Hispanic women, drawn from a pediatric primary care setting, with an infant aged 0 to 10 months, 6 structural models guided by the empirical literature were evaluated using confirmatory factor analysis.
Results
Results supported a 2-factor model of depression and anxiety as the best fitting model. Multigroup models supported the factorial invariance across women who completed the EDPS in English and Spanish.
Conclusion
These findings provide initial support for the 2-factor structure of the EPDS among Hispanic women in the United States.
Keywords: postpartum depression, anxiety, factor structure, Hispanic women
Postpartum depression (PPD) is prevalent, occurring in 10%–15% of mothers (Gavin et al., 2005; Vesga-Lopez et al., 2008). According to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR; American Psychiatric Association [APA], 2000), PPD refers to a major depressive episode that begins within the 4 weeks after childbirth, although researchers increasingly view major depressive disorder (MDD) within the first year to constitute PPD (O’Hara, 2009). The DSM-IV-TR (APA, 2000) symptom criteria for PPD are identical to the symptom criteria for a major depressive episode without postpartum onset, including somatic symptoms. Somatic symptoms such as sleep disturbances and weight and appetite changes are common during the postpartum period, even in the absence of other depressive symptoms. This overlap between MDD diagnostic criteria and common somatic experiences among women during the postpartum period has raised concern about the possibility of misinterpreting such experiences as depressive symptoms, which could lead to false positives on PPD screenings.
In response to this concern, the Edinburgh Postnatal Depression Scale (EPDS; Cox, Holden, & Sagovsky, 1987), a widely used 10-item self-report measure, was developed to screen for major depression in the postpartum period without confounding somatic symptoms that are common to the postpartum period. Although the EPDS has been conceptualized as a unidimensional measure of PPD symptoms (Cox et al., 1987), research indicates that it likely assesses multiple factors including depression, anxiety (for a review, see Phillips, Charles, Sharpe, & Matthey, 2009), anhedonia (Lee King, 2012; Chabrol & Teissedre, 2004; Montazeri, Torkan, & Omidvari, 2007; Tuohy & McVey, 2008), and suicide (Brouwers, van Baar, & Pop, 2001; Jomeen & Martin 2005; Ross, Gilbert Evans, Sellers, & Romach, 2003; Tuohy & McVey, 2008).
Previous research examining the factor structure of the EPDS has generally supported two-or three-factor models. In studies using exploratory techniques such as principal components analysis (PCA) or exploratory factor analysis (EFA), support has been obtained for three-factor models comprising depression, anxiety, and suicide (Brouwers et al., 2001; Ross et al., 2003) and depression, anxiety, and anhedonia (Tuohy & McVey, 2008). Other studies using PCA or EFA, including a study conducted among mothers in Spain (Maroto Navarro, Garcia Calvante, & Fernandez Parra, 2005), found support for a two-factor model comprising depression and anxiety (Phillips et al., 2009).
Based on the findings from EFA on the EPDS, recent studies have used confirmatory factor analysis (CFA) to evaluate and compare the fit of proposed structural models. For example, Jomeen and Martin (2005) used CFA to evaluate a one-factor model, multiple two-factor models, and multiple three-factor models among 101 women in the United Kingdom. A two-factor model comprising depression and anxiety provided the best fit to the data. Phillips et al. (2009) used EFA and CFA to evaluate a one-factor model and multiple two-factor models among 309 mothers in Australia. Each of the two-factor models provided an adequate fit to the data and provided a superior fit than the one-factor model. A two-factor model comprised of Depression and Anxiety provided the best fit. Recently, Lee King (2012) used CFA to evaluate the fit of five structural models in a sample of 169 postpartum African American women. A three-factor model comprising depression, anxiety, and anhedonia provided the best fit to the data.
Thus, research examining the factor structure of the EPDS consistently supports either a two-or three-factor model over a one-factor model. To date, however, no study has examined the factor structure of the EPDS among Hispanic women in the United States. This is an important gap in the knowledge base because of the growing size of the Hispanic population in the United States and the high rate of childbirth among Hispanic women in the United States. Hispanics currently represent the nation’s largest ethnic minority group (U.S. Census Bureau, 2011) and had the highest birth rate of any ethnic group in the United States from 1990 to 2007, indicating that (a) the population continues to grow at a rapid pace (U.S. National Center for Health Statistics, 2010) and (b) a large percentage of the population includes women of childbearing age.
Additionally, Hispanic women have been found to report significantly higher levels of post-partum depressive symptoms and to be more likely to meet criteria for a diagnosis of PPD than non-Hispanic White and non-Hispanic Black women (Howell, Mora, Horowitz, & Leventhal, 2005; Liu & Tronick, 2013). These population and depression estimates highlight the need to ensure the appropriateness of PPD measures for Hispanic women in the United States.
The purpose of the current study was to examine the factor structure and psychometric properties of the EPDS among Hispanic mothers in the United States. The first aim was to identify the best fitting structural model for Hispanic mothers who completed the EPDS in English and Hispanic mothers who completed the EPDS in Spanish from six different models guided by past research: the five separate models evaluated in Lee King (2012) and a two-factor model previously supported among mothers in Spain (Maroto Navarro et al., 2005). We selected these six models because they included the one-, two-, and three-factor models evaluated in prior studies of the EPDS among non-Hispanic women (Lee King, 2012), as well as the two-factor model supported for the Spanish version of the EPDS (Maroto Navarro et al., 2005). The second aim was to examine factorial invariance across mothers who completed the EDPS in English and mothers who completed the EPDS in Spanish. Finally, we examined the internal reliability of the total EPDS score and EPDS factor scores and explored the scale’s convergent validity via associations between the EPDS scores and history of mental health treatment.
Method
Participants and Procedures
Participants were recruited from a large outpatient pediatric primary care clinic housed in a pediatric hospital in an urban area in the Southeastern United States. Participants attended the clinic for either a well or sick visit for their infants. Approximately 90% of patients at the pediatric clinic receive Medicaid or other state-funded insurance programs. Research assistants approached 522 mothers of child patients between 0 and 10 months of age to briefly describe the study. After explanation of the study, 280 mothers (53.6%) expressed interest and provided informed consent to participate; the remaining mothers declined to participate. Common reasons that mothers declined were as follows: not interested, not enough time at the appointment, and too busy. This study was approved by the institutional review boards at both the pediatric hospital and affiliated university.
Because of the focus on the EPDS among Hispanic women, only the 220 (78.6%) participants who self-identified as Hispanic were included in the present study. Participants self-identified as Hispanic by answering yes to the question, “Are you Hispanic or Latino?” Hispanic mothers did not differ significantly from non-Hispanic mothers on any measured variables, including total EPDS scores, age, or level of education (ps > .05). Descriptive statistics for the demographic variables are shown in Table 1. As shown in the table, most of the sample was either currently married or never married and about one third of the sample had a high school education or failed to complete high school.
Table 1.
Sample Characteristics for EPDS Completed in English and Spanish
| English Sample | Spanish Sample | |
|---|---|---|
| No. of mothers | 122 | 98 |
| Mean age of mom (SD) | 26.76 (6.34) | 30.26 (5.67) |
| Mean age of infant in months (SD) | 4.05 (3.25) | 4.59 (3.16) |
| Mean score on EPDS (SD) | 6.61 (5.12) | 5.38 (4.86) |
| Relationship status | ||
| % Married | 34.4% | 56.1% |
| % Seperated | 4.1% | 4.1% |
| % Divorced | 3.3% | 3.1% |
| % Widowed | 1% | 0% |
| % Single | 55.7% | 35.7% |
| Education level | ||
| No high school | 11.4% | 6.1% |
| High school degree | 16.4% | 29.6% |
| Some college | 48.4% | 26.5% |
| College degree | 19.7% | 18.4% |
| Graduate degree | 4.1% | 18.4% |
Note. SD = standard deviation; EPDS = Edinburgh Postnatal Depression Scale.
Of the participants, 122 (55.5%) completed the EPDS in English and 98 (44.5%) completed the EPDS in Spanish. Those who completed the EPDS in English versus Spanish did not differ significantly on total EPDS score, education level, or age of infant (ps > .05). However, participants who completed the EPDS in English (mean [M] = 26.76, standard deviation [SD] = 6.34, range = 18 to 44) were significantly younger than participants who completed the EPDS in Spanish (M = 30.26, SD = 5.67, range = 18 to 44), t(217) = −4.24, p < .001. Participants whose infant was younger than 2 weeks old did not significantly differ from participants whose infants who were older than 2 weeks old on total EPDS score (p = .65). Factor models were examined before and after excluding participants with infants younger than 2 weeks old and the conclusions did not differ between groups. Thus, we present results from the total sample including mothers with infants younger than 2 weeks old.
Measures
Postpartum depressive symptoms were measured by the EPDS (Cox et al., 1987). The EPDS was administered orally to participants. Each of the 10 items is scored on a 4-point scale (0 to 3). Total scores range from 0 to 30 and a cutoff of ≥ 13 has demonstrated adequate specificity and sensitivity for a diagnosis of PPD with non-Hispanic postpartum populations (Harris, Huckle, Thomas, Johns, & Fung, 1989; Matthey, Henshaw, Elliott, & Barnett, 2006). Convergent validity has been established via significant associations with a diagnosis of PPD (Murray & Cox, 1990) and with other depressive symptom scales (Pen, Wang, Jin, & Fan, 1994).
Garcia-Esteve et al. (2003) developed a Spanish translation of the EPDS and evaluated it among mothers in Spain; that translation was used in the present study for mothers who elected to complete the measure in Spanish. To ensure the appropriateness of the Spanish translation for Hispanic women in the United States, five English–Spanish bilingual mental health professionals from different countries of origin (e.g., Cuba, United States) independently reviewed the scale for words or phrases that were difficult to understand. No difficult words or phrases were identified.
A demographic and background form was administered to all participants. In addition to collecting information on demographic variables, this form also included items assessing history of mental health treatment utilization (counseling/therapy and prescription medication for mental health problems). Eleven participants (5.0%) declined to respond to the questions about prior history of mental health treatment. These 11 participants did not differ significantly from the other 209 participants on the total EPDS score (ps > .05).
Data Analysis
CFAs were conducted in the Mplus Version 7 software program (Muthén & Muthén, 1998–1998) using maximum likelihood estimation with robust standard errors to evaluate six models guided by the literature. Maximum likelihood estimation with robust standard errors was selected due to its relative robustness with ordinal variables and small samples (Sass, 2011). Models were first evaluated separately among participants who completed the EPDS in English and among participants who completed the EPDS in Spanish. Factors from multifactor models were allowed to correlate, which is consistent with theorized associations between depressed mood, anxiety, and anhedonia, and with previous research indicating significant associations between depression, anxiety, and anhedonia factors (Brouwers et al., 2001; Karimova & Martin, 2003; Watson, 2005).
Given the absence of a compelling theoretical justification for correlated error terms, we did not allow them. The six models used to evaluate the best model fit were as follows: (a) Cox et al.’s (1987) one-factor model; (b) Brouwer et al.’s (2001) two-factor model of depression and anxiety; (c) Ross et al.’s (2003) two-factor model of depression and anxiety; (d) Maroto Navarro et al.’s (2005) two-factor model of depression and anxiety; (e) Phillips et al.’s (2009) two-factor model of depression and anxiety; and (f) Tuohy and McVey’s (2008) three-factor model of anhedonia, depression and anxiety. Brouwers et al.’s and Ross et al.’s models were originally three-factor models; however, the third factor was omitted because only one item (the suicide item) loaded on that factor. In the current sample, there were no missing data on the EPDS.
Following recommendations of Bollen and Long (1993), a variety of global fit indices were used to examine model fit, including indices of absolute fit, indices of relative fit, and indices of fit with a penalty function for lack of parsimony. These included the traditional overall chi-square test of model fit (which should not be statistically significant), the root mean square error of approximation (RMSEA; which should be less than 0.08 to declare good fit), the comparative fit index (CFI; which should be equal to or greater than 0.95 to declare good fit and equal to or greater than 0.90 to declare adequate fit), and the standardized root mean square residual (SMSR; which should be equal to or less than 0.05; Hu & Bentler, 1999; Brown, 2006).
In addition to the global fit indices, more focused tests of fit were pursued. These included examination of the standardized residual covariances (which should be between −2.00 and 2.00) and modification indices (which should be less than 4.00; Jaccard & Wan, 1996). Parameter estimates were examined for Heywood cases, or offending estimates. Comparisons of nested models using the Satorra Bentler chi-square difference test were used to examine measurement invariance across participants who completed the EPDS in English and participants who completed the EPDS in Spanish (Satorra, 2000).
Results
Factor Structure of the EPDS
CFAs were conducted to examine the fit of the six structural models among the English- and Spanish-language participants. Tables 2 and 3 present the six models with corresponding fit indices among each group. Examination of the fit indices (chi-square, RMSEA, CFI, and the SRMR) revealed that the two-factor models of depression and anxiety reported by Brouwers et al. (2001), Ross et al. (2003), and Phillips et al. (2009) provided good fits to the data among English-language participants. Because the models were not nested, we were not able to statistically compare the fit of the three models that provided good fits. Among Spanish-language participants, only the two-factor model of depression and anxiety reported by Ross et al. (2003) provided a good fit to the data. No other model provided an acceptable fit among Spanish-language participants.
Table 2.
CFA of English Version of EPDS for Six Models and Fit Indices (n = 122)
| Model | Factor structure | X2 | df | p | RMSEA | CFI | SRMR |
|---|---|---|---|---|---|---|---|
| Cox et al. (1987) | F1: 1, 2, 3, 4, 5, 6, 7, 8, 9, 10 | 59.14 | 35 | 0.01 | 0.08 | 0.92 | 0.06 |
| Brouwers et al. (2001) | F1: 1, 2, 8 F2: 3, 4, 5 |
12.57 | 8 | 0.13 | 0.07 | 0.97 | 0.04 |
| Ross et al. (2003) | F1: 1, 2, 8, 9 F2: 3, 4, 5 |
21.02 | 13 | 0.07 | 0.07 | 0.96 | 0.04 |
| Navarro et al. (2005) | F1: 2, 3, 4, 5, 6, 9 F2: 1, 7, 8, 10 |
59.27 | 34 | 0.00 | 0.08 | 0.92 | 0.06 |
| Tuohy & McVey (2008) | F1: 1, 2 F2: 3, 4, 5 F3: 7, 8, 9, 10 |
88.65 | 35 | 0.00 | 0.11 | 0.82 | 0.15 |
| Phillips et al. (2009) | F1: 1, 2, 6, 7, 8, 9, 10 F2: 3, 4, 5 |
43.19 | 34 | 0.13 | .05 | .97 | .05 |
Note. CFA = confirmatory factor analysis; EPDS = Edinburgh Postnatal Depression Scale; df = degree of freedom; RMSEA = root mean square error of approximation; CFI = comparative fit index; SMSR = standardized root mean square residual.
Table 3.
CFA of Spanish Version of EPDS for Six Models and Fit Indices (n = 98)
| Model | Factor structure | X2 | df | p | RMSEA | CFI | SRMR |
|---|---|---|---|---|---|---|---|
| Cox et al. (1987) | F1: 1, 2, 3, 4, 5, 6, 7, 8, 9, 10 | 105.87 | 35 | 0.00 | 0.14 | 0.78 | 0.09 |
| Brouwers et al. (2001) | F1: 1, 2, 8 F2: 3, 4, 5 |
15.23 | 8 | 0.05 | 0.09 | 0.89 | 0.05 |
| Ross et al. (2003) | F1: 1, 2, 8, 9 F2: 3, 4, 5 |
21.94 | 13 | 0.06 | 0.08 | 0.93 | 0.05 |
| Navarro et al. (2005) | F1: 2, 3, 4, 5, 6, 9 F2: 1, 7, 8, 10 |
112.29 | 34 | 0.00 | 0.15 | 0.75 | 0.09 |
| Tuohy & McVey (2008) | F1: 1, 2 F2: 3, 4, 5 F3: 7, 8, 9, 10 |
142.83 | 35 | 0.00 | 0.18 | 0.67 | 0.18 |
| Phillips et al. (2009) | F1: 1, 2, 6, 7, 8, 9, 10 F2: 3, 4, 5 |
102.64 | 34 | 0.00 | 0.14 | 0.79 | 0.09 |
Note. CFA = confirmatory factor analysis; EPDS = Edinburgh Postnatal Depression Scale; df = degree of freedom; RMSEA = root mean square error of approximation; CFI = comparative fit index; SMSR = standardized root mean square residual.
Measurement Invariance
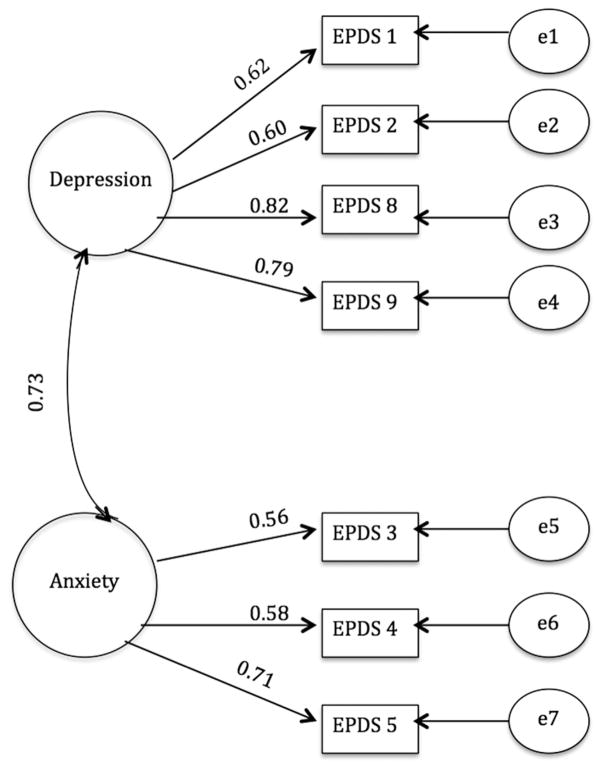
Because the Ross et al. (2003) was the only model to provide acceptable fit among both English-and Spanish-language participants, we retained it for evaluation of measurement invariance across languages. For this analysis, the model was evaluated among the combined sample of English- and Spanish-language participants. This model yielded an acceptable fit: X2(13) = 38.60, p = .01; RMSEA = 0.07; CFI = 0.94; SMSR = 0.04. The chi-square (X2) value was significant (p < .05), which is common with large sample sizes and does not necessarily indicate poor fit (e.g., Kline, 2011; Marsh, Balla, & McDonald, 1988). Figure 1 presents the standardized parameter estimates for the final model combining English- and Spanish-language participants. All factor loadings in the final model were statistically significant.
Figure 1.
The two-factor model of the EPDS among Hispanic women in the Unites States (n = 220). Note. Standardized factor loadings are presented and all are significant at p < .05.
Two additional models were tested to examine measurement invariance across participants who completed the EPDS in English and participants who completed the EPDS in Spanish. A multigroup solution was pursued with English- and Spanish-language participants representing the two groups. The first model, the equal form model, sought to establish a common model form in the two groups; thus, there were no equality constraints across groups. The equal form model yielded adequate fit (Table 4). More focused tests of fit did not reveal theoretically meaningful and sizeable modification indices, nor were any of the absolute standardized residuals larger than 1.96.
Table 4.
Models used in testing for measurement invariance across
| Model | Constraints | X2 | df | p | RMSEA | CFI | SRMR |
|---|---|---|---|---|---|---|---|
| Equal Form Model | None | 49.32 | 31 | 0.02 | 0.07 | 0.94 | 0.05 |
| Measurement Invariance Model | Corresponding factor loadings equal across groups | 50.68 | 36 | 0.05 | 0.06 | 0.95 | 0.06 |
The second model, the measurement invariance model, tested for measurement invariance across the groups for the latent variables. This model was identical to the equal form model but constrained corresponding factor loadings to be equivalent across groups (i.e., English and Spanish). This model also yielded an adequate fit (Table 4). More focused tests of fit revealed no theoretically meaningful and sizeable modification indices, nor were any of the absolute standardized residuals larger than 1.96. The Satorra Bentler chi-square test comparing the measurement invariance model to the equal form model yielded a statistically nonsignificant chi-square difference, X2 diff(5) = 0.79, ps > .05, indicating no significant difference in model fit. On the basis of parsimony, therefore, the measurement invariance model was retained over the equal form model.
Internal Reliability and Convergent Validity
EPDS scores ranged from 0 to 24 with a mean of 6.06 (SD = 5.07), indicating minimal to mild depressive symptoms on average. Internal reliability for the total scale score was acceptable for the total sample (α = .84, average inter-item correlation [AIC] = .36), for those who completed the EPDS in English (α = .84, AIC = .3–6), and for those who completed the EDPS in Spanish (α = .84, AIC = .35). The average AICs indicate a moderate and acceptable degree of association between items (Spector, 1992). For the retained two-factor model of depression and anxiety reported by Ross et al. (2003), internal reliability in the combined sample was acceptable for the depression factor (items 1, 2, 8, 9; α = .80; AIC = 0.50) and adequate for the anxiety factor (items 3, 4, 5; α = .65; AIC = 0.38).
A minority of participants (17.7%) endorsed a history of mental health treatment. Specifically, 11.8% endorsed a history of counseling/therapy and 5.9% endorsed a history of prescription medication use for mental health problems. Two independent samples t tests were conducted to compare the EPDS total score across participants with and without a history of counseling/therapy and across participants with and without a history of prescription medication usage for mental health problems. In support of convergent validity, there were significant differences in the total EPDS score across groups, such that participants who endorsed a history of counseling/therapy (M = 9.69, SD = 6.23) had significantly higher scores on the EPDS than participants who did not (M = 5.71, SD = 4.78), t(205) = −3.81, p < .001. Similarly, participants who endorsed a history of prescription medication use (M = 10.15, SD = 5.35) had significantly higher scores on the EPDS than participants who did not (M = 5.76, SD = 4.79), t(205) = −3.18, p < .05.
Discussion
The purpose of the current study was to examine the factor structure and psychometric properties of the EDPS among Hispanic women in the United States. We compared six models guided by the empirical literature to identify the best fitting model in a sample of 220 Hispanic mothers of infants, 122 of whom completed the EPDS in English and 98 of whom completed the EPDS in Spanish. A two-factor model of depression and anxiety, as reported by Ross et al. (2003), provided a good, but not excellent, fit to the data among English- and Spanish-language participants. Measurement invariance of the two-factor model was supported across English and Spanish versions. Two other two-factor models comprising depression and anxiety (Brouwers et al., 2001; Phillips et al., 2009) provided good fits to the data among English-language participants, but not among Spanish-language participants. Because these three models that provided good fits to the data among English-language participants were not nested, we were unable to statistically evaluate whether one provided a better fit to the data than the others. However, each of the three models was characterized by the same general factor structure of depression and anxiety.
The findings from the CFA suggest that the EPDS does not have a unidimensional structure among Hispanic women, which is consistent with findings on the EPDS factor structure among women from other ethnic backgrounds (Lee King, 2012). Rather, the EPDS is best characterized by a bidimensional structure of depression and anxiety. Our finding of this two-factor structure is consistent with several prior studies among samples of non-Hispanic women, although there are minor variations across studies with respect to which specific items load on the depression factor (Brouwers et al., 2001; Ross et al., 2003; Jomeen & Martin, 2005; Phillips et al., 2009). However, the items that load on the anxiety factor are consistent across studies.
One implication of the bidimensional structure of the EPDS is that it can be used as a screen for not only postpartum depression but also possibly postpartum anxiety. Additional research on the screening properties and validity of the Anxiety factor among Hispanic women is an important avenue for future research. Although the suicide/self-harm item (item 10) is not included on either the depression factor or the anxiety factor, its inclusion is warranted when assessing postpartum depressive symptoms given the clinical importance of identifying mothers who are at risk for self-harm.
The total scale displayed acceptable internal reliability, and each of the two factors displayed adequate internal reliability. The somewhat low reliability of the anxiety factor is likely at least in part due to the low number of items on that factor (three). The internal reliability was highly consistent across English- and Spanish-language versions. Further, significant associations between the total scale score and history of mental health treatment utilization provide initial support for the convergent validity of the EPDS among Hispanic mothers. These findings thus provide initial support for the use of the EPDS among both English- and Spanish-speaking mothers of Hispanic ethnicity in the United States.
This study’s findings should be interpreted in light of its limitations. The sample was drawn from Hispanic woman attending a pediatric primary care clinic in the Southeastern United States, and the rate of participation was somewhat low (54%). Data were not available on participants’ ethnic subgroup, country of origin, and years living in the United States. It is unclear the extent to which these findings would generalize to Hispanic women from other geographical locations in the United States. The absence of diagnostic data on PPD prevented the identification of an optimal cutoff score for use as a screener among Hispanic women in primary care settings. Additionally, the absence of other measures of depression and anxiety prevented a thorough evaluation of the scale’s convergent validity. Finally, history of mental health treatment utilization was obtained by self-report, and it is possible participants may have underreported treatment utilization due to concerns about stigma or social desirability.
Conclusion
Despite these limitations, the current study is the first to evaluate the factor structure and internal reliability of the EPDS among English- and Spanish speaking Hispanic women in the United States. Preliminary support for the convergent validity of the EPDS was demonstrated via significant associations between total scale scores and history of mental health treatment utilization. Thus, the EPDS appears appropriate for use as a PPD screener among Hispanic women in the United States. Given the brevity of administering and scoring the EPDS as well as the high prevalence and public health impact of PPD, routine use of the EPDS as a screening instrument in primary care settings is encouraged.
Acknowledgments
This work was supported by a faculty development award from Florida International University to the fourth author and a career development award from the National Institute of Mental Health to the fifth author (K23 MH85659).
We thank Ryan Hill, Gabriela Hungerford, Dainelys Linares, and Michael Meinzer for their assistance with this project.
Footnotes
We report no conflicts of interest.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Press; 2000. text rev. [Google Scholar]
- Bollen K, Long S. Testing structural equation models. Thousand Oaks, CA: Sage; 1993. [Google Scholar]
- Brouwers EPM, van Baar AL, Pop VJM. Does the Edinburgh Postnatal Depression Scale measure anxiety? Journal of Psychosomatic Research. 2001;51(5):659–663. doi: 10.1016/S0022-3999(01)00245-8. [DOI] [PubMed] [Google Scholar]
- Brown TA. Confirmatory factor analysis for applied research. New York, NY: Guilford Press; 2006. [Google Scholar]
- Chabrol H, Teissedre F. Relation between Edinburgh Postnatal Depression Scale scores at 2–3 days and 4–6 weeks postpartum. Journal of Reproductive and Infant Psychology. 2004;22(1):33–39. doi: 10.1080/02646830310001643067. [DOI] [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Garcia-Esteve L, Ascaso C, Ojuel J, Navarro P. Validation of the Edinburgh Postnatal Depression Scale (EPDS) in Spanish mothers. Journal of Affective Disorders. 2003;75(1):71–76. doi: 10.1016/s0165-0327(02)00020-4. Retrieved from http://www.sciencedirect.com.ezproxy.fiu.edu/science/article/pii/S0165032702000204. [DOI] [PubMed] [Google Scholar]
- Gavin N, Gaynes B, Lohr K, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: A systematic review of prevalence and incidence. Obstetrics & Gynecology. 2005;106(5):1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- Harris B, Huckle P, Thomas R, Johns S, Fung H. The use of rating scales to identify post-natal depression. The British Journal of Psychiatry. 1989;154:813–817. doi: 10.1192/bjp.154.6.813. [DOI] [PubMed] [Google Scholar]
- Howell EA, Mora PA, Horowitz CR, Leventhal H. Racial and ethnic differences in factors associated with early postpartum depressive symptoms. Obstetrics & Gynecology. 2005;105(6):1442–1450. doi: 10.1097/01.AOG.0000164050.34126.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Jaccard J, Wan CK. LISREL approaches to interaction effects in multiple regression. Thousand Oaks, CA: Sage; 1996. [Google Scholar]
- Jomeen J, Martin CR. Replicability and stability of the multidimensional model of the edinburgh postnatal depression scale in late pregnancy. Journal of Psychiatric and Mental Health Nursing. 2007;14(3):319–324. doi: 10.1111/j.1365-2850.2007.01084.x. [DOI] [PubMed] [Google Scholar]
- Karimova GK, Martin CR. A psychometric evaluation of the Hospital Anxiety and Depression Scale during pregnancy. Psychology, Health and Medicine. 2003;8:89–103. doi: 10.1080/1354850021000059296. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 3. New York, NY: Guilford Press; 2011. [Google Scholar]
- Lee King PA. Replicability of structural models of the Edinburgh Postnatal Depression Scale (EPDS) in a community sample of postpartum African American women with low socioeconomic status. Archives of Women’s Mental Health. 2012;15(2):77–86. doi: 10.1007/s00737-012-0260-8. [DOI] [PubMed] [Google Scholar]
- Liu C, Tronick E. Rates and predictors of postpartum depression by race and ethnicity: Results from the 2004 to 2007 New York City PRAMS Survey (Pregnancy Risk Assessment Monitoring System) Maternal and Child Health Journal. 2013;17:1599–1610. doi: 10.1007/s10995-012-1171-z. [DOI] [PubMed] [Google Scholar]
- Maroto Navarro G, García Calvente MdM, Fernández Parra A. Evaluación del estado de ánimo en el puerperio con la Escala de Depresión Postnatal de Edimburgo. [Evaluation of mood in the postpartum period with the Edinburgh Postnatal Depression Scale]. International Journal of Clinical and Health Psychology. 2005;5(2):305–318. Retreieved from http://www.redalyc.org/articulo.oa?id=33750206. [Google Scholar]
- Marsh HW, Balla JR, McDonald RP. Goodness-of-fit indexes in confirmatory factor analysis: The effect of sample size. Psychological Bulletin. 1988;103(3):391–410. doi: 10.1037/0033-2909.103.3.391. [DOI] [Google Scholar]
- Matthey S, Henshaw C, Elliott S, Barnett B. Variability in use of cut-off scores and formats on the Edinburgh Postnatal Depression Scale –implications for clinical and research practice. Archives of Women’s Mental Health. 2006;9(6):309–315. doi: 10.1007/s00737-006-0152-x. [DOI] [PubMed] [Google Scholar]
- Montazeri A, Torkan B, Omidvari S. The Edinburgh Postnatal Depression Scale (EPDS): Translation and validation study of the iranian version. BMC Psychiatry. 2007:7. doi: 10.1186/1471-244X-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray D, Cox JL. Screening for depression during pregnancy with the Edinburgh Postnatal Depression Scale (EPDS) Journal of Reproductive and Infant Psychology. 1990;8(2):99–107. doi: 10.1080/02646839008403615. [DOI] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 6. Los Angeles, CA: Muthén & Muthén; 1998–2011. [Google Scholar]
- O’Hara MW. Postpartum depression: What we know. Journal of Clinical Psychology. 2009;65(12):1258–1269. doi: 10.1002/jclp.20644. [DOI] [PubMed] [Google Scholar]
- Pen T, Wang L, Jin Y, Fan X. The evaluation and application of the Edinburgh Postnatal Depression Scale. Chinese Mental Health Journal. 1994;8(1):18–19. 4. [Google Scholar]
- Phillips J, Charles M, Sharpe L, Matthey S. Validation of the subscales of the Edinburgh Postnatal Depression Scale in a sample of women with unsettled infants. Journal of Affective Disorders. 2009;118(1–3):101–112. doi: 10.1016/j.jad.2009.02.004. [DOI] [PubMed] [Google Scholar]
- Ross LE, Evans SEG, Sellers EM, Romach MK. Measurement issues in postpartum depression part 1: Anxiety as a feature of postpartum depression. Archives of Women’s Mental Health. 2003;6(1):51–57. doi: 10.1007/s00737-002-0155-1. [DOI] [PubMed] [Google Scholar]
- Sass D. Testing measurement invariance and comparing latent factor means within a confirmatory factor analysis framework. Journal of Psychoeducational Assessment. 2011;29:347–363. doi: 10.1177/0734282911406661. [DOI] [Google Scholar]
- Satorra A. Scaled and adjusted restricted tests in multi-sample analysis of moment structures. In: Heijmans RDH, Pollock DSG, Satorra A, editors. Innovations in multivariate statistical analysis. A Festschrift for Heinz Neudecker. London: Kluwer; 2000. pp. 233–247. [Google Scholar]
- Spector PE. Summated rating scale construction: An introduction. Thousand Oaks, CA: Sage; 1992. [Google Scholar]
- Tuohy A, McVey C. Subscales measuring symptoms of non-specific depression, anhedonia, and anxiety in the Edinburgh Postnatal Depression Scale. British Journal of Clinical Psychology. 2008;47(2):153–169. doi: 10.1111/j.2044-8260.2008.tb00463.x. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. Annual estimates of the resident population by sex, race, and Hispanic origin for the United States: April 1 2010 to July 1, 2011. 2011 Retrived from http://www.census.gov/popest/data/national/asrh/2011/index.html.
- U.S National Center for Health Statistics, National Vital Statistics Reports. Births: Final Data for 2007. 2010 Retrieved from http://www.cdc.gov/nchs/data/nvsr/nvsr58/nvsr58_24.pdf. [PubMed]
- Vesga-López O, Blanco C, Keyes K, Olfson M, Grant BF, Hasin DS. Psychiatric disorders in pregnant and postpartum women in the united states. Archives of General Psychiatry. 2008;65(7):805–815. doi: 10.1001/archpsyc.65.7.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D. Rethinking the mood and anxiety disorders: A quantitative hierarchical model for DSM-V. Journal of Abnormal Psychology. 2005;114(4):522–536. doi: 10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]