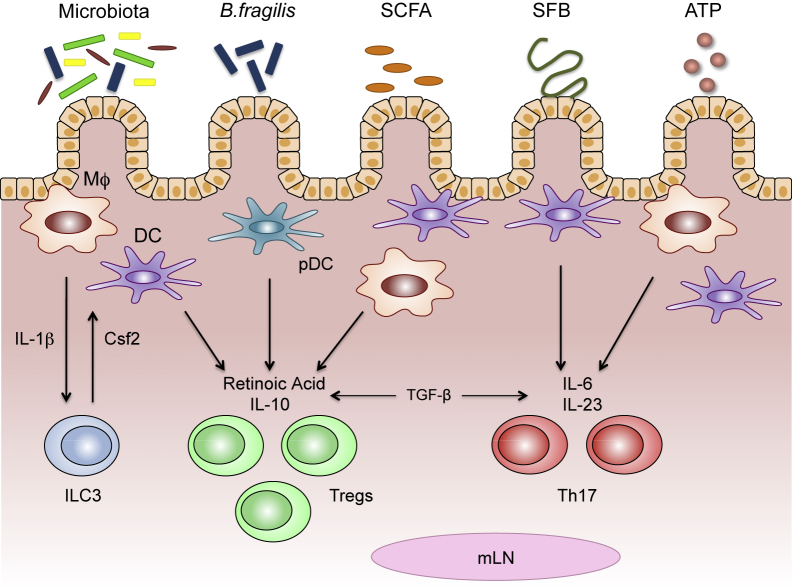
Figure 3.
Microbial factors condition intestinal macrophages (MΦ) and dendritic cells (DCs) to promote unique T-cell responses. Different members of the microbiota and their components can stimulate intestinal macrophages and/or DCs to induce regulatory T cells (Tregs) or type 17 helper T cells (Th17). Macrophages secrete IL-1β in response to commensal bacteria, prompting the production of colony-stimulating factor 2 (Csf2) from type 3 innate lymphoid cells (ILC3s). Csf2 can then engage macrophages and DCs to produce regulatory molecules (eg, retinoic acid and IL-10) involved in the induction of Treg cells. Polysaccharide A (PSA), expressed by Bacteroides fragilis and commensal-derived short-chain fatty acids (SCFAs), can also act on intestinal macrophages and DCs to stimulate retinoic acid and IL-10 production, and induce Treg cell differentiation. Segmented filamentous bacteria (SFB) can gain close contact with the intestinal epithelium, initiating signaling programs that drive the secretion of IL-6 and IL-23 from macrophages and DCs, leading to Th17 differentiation. ATP derived from commensal bacteria can bind receptors on intestinal macrophages and/or DCs, leading to enhanced IL-6 and IL-23 expression and the induction of Th17 cells. Both Treg and Th17 differentiation also require transforming growth factor (TGF)-β, which is constitutively expressed in the intestine. mLN, mesenteric lymph node; pDC, plasmacytoid dendritic cell.